Deep brain stimulation dbs – Deep brain stimulation (DBS) offers a revolutionary approach to treating neurological and psychiatric conditions. This innovative procedure involves implanting electrodes deep within the brain to deliver electrical impulses, effectively modulating neural activity. Understanding the history, procedures, and ethical considerations surrounding DBS is crucial for anyone seeking information on this advanced medical technology.
The journey of DBS began with early experiments and has evolved into a sophisticated technique. Modern DBS systems offer precise targeting of specific brain regions, aiming to alleviate debilitating symptoms. This article will explore the intricacies of DBS, from the initial procedure to the long-term management of patients, touching upon its various applications, surgical considerations, and ethical implications.
Introduction to Deep Brain Stimulation (DBS)
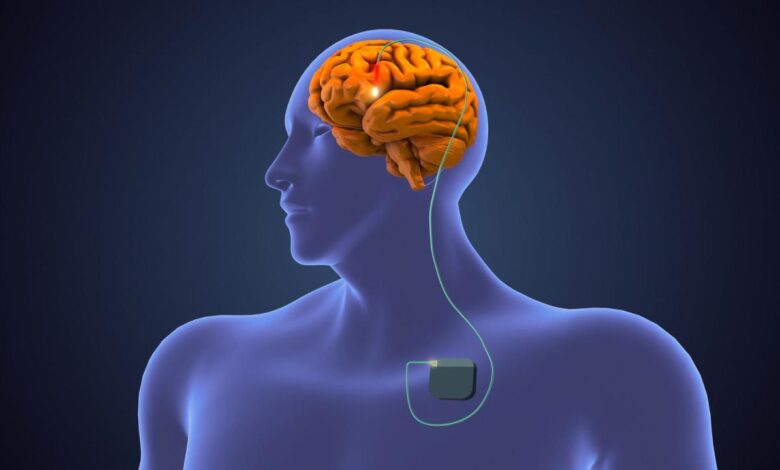
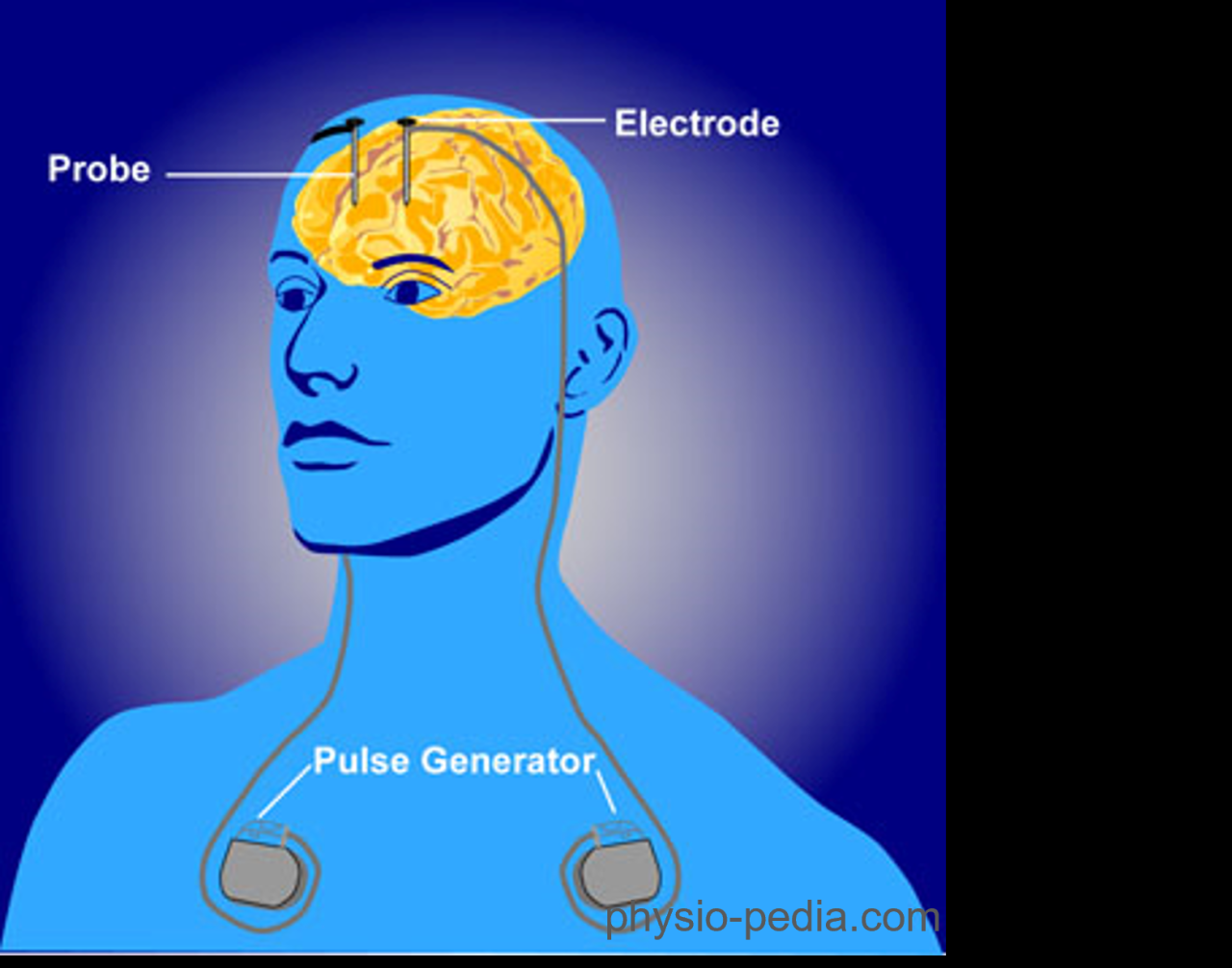
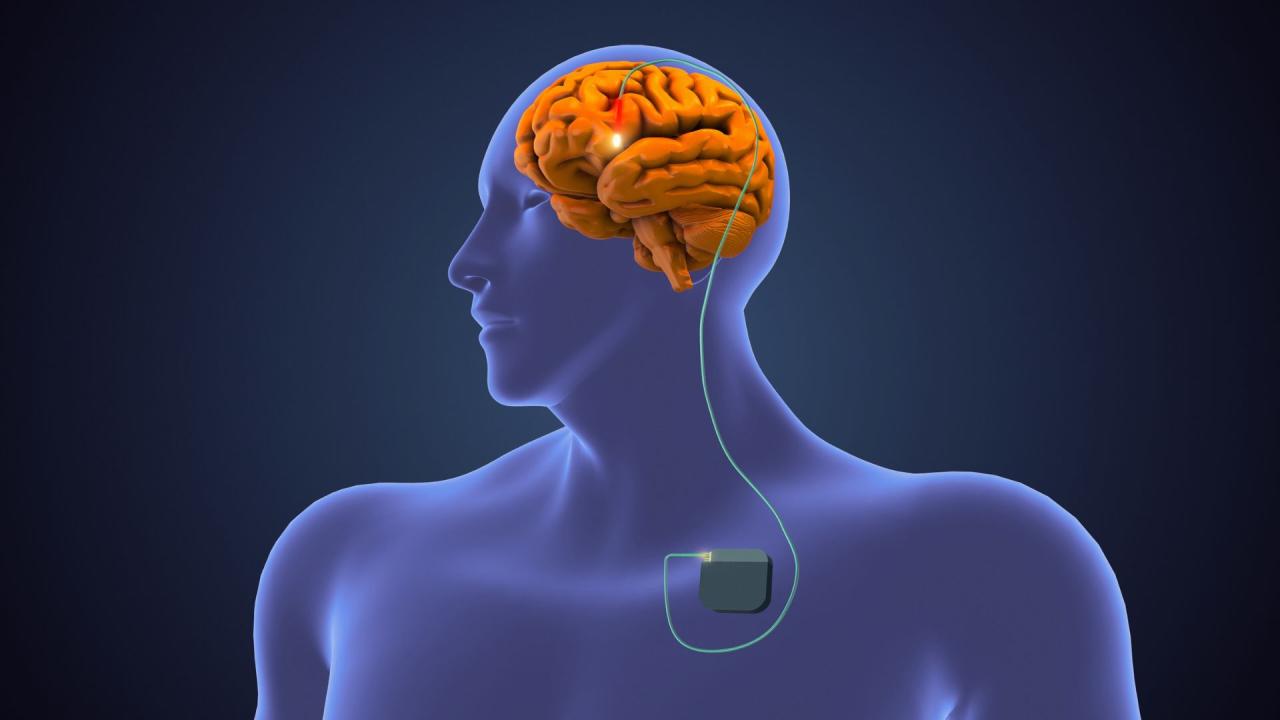
Deep Brain Stimulation (DBS) is a neurosurgical procedure that involves implanting electrodes into specific areas of the brain to deliver electrical impulses. These impulses are designed to modulate the abnormal electrical activity that can cause various neurological and movement disorders. DBS has revolutionized the treatment of conditions previously considered largely intractable.The fundamental principle behind DBS is to interrupt the abnormal neural pathways causing symptoms.
This is achieved by precisely targeting specific brain regions implicated in the disorder and delivering electrical stimulation to those regions. By modulating the activity of these regions, DBS can help alleviate symptoms and improve quality of life for many patients.
History and Evolution of DBS
The concept of using electrical stimulation to treat neurological disorders has a long history. Early experiments in the late 19th and early 20th centuries demonstrated the potential of electrical stimulation to affect brain function. However, it wasn’t until the development of more sophisticated surgical techniques and precise targeting methods that DBS became a viable and effective treatment option.
Early DBS devices were relatively bulky and required frequent adjustments. Over time, advancements in battery technology, electrode design, and surgical techniques led to smaller, more reliable, and longer-lasting devices. Modern DBS systems are highly sophisticated and precisely controlled, enabling more targeted stimulation and minimizing potential side effects.
Basic Principles of DBS
The effectiveness of DBS hinges on precise targeting of specific brain regions. Neurologists use a variety of imaging techniques, including MRI and CT scans, to identify the specific areas of the brain associated with the patient’s symptoms. This detailed mapping process is crucial for accurate electrode placement. Neurologists work closely with neurosurgeons to ensure the electrodes are implanted in the intended locations.
Careful pre-operative planning is paramount to maximize the potential benefits of DBS while minimizing risks.
Targeting Specific Brain Regions
Precise targeting of specific brain regions is critical for the efficacy of DBS. Neurologists and neurosurgeons employ various techniques to achieve this. They use advanced imaging techniques to identify the specific areas of the brain that are implicated in the patient’s symptoms. This allows for the placement of electrodes in the most appropriate locations. The specific brain regions targeted will vary depending on the condition being treated.
For example, for Parkinson’s disease, the subthalamic nucleus or globus pallidus interna might be targeted.
Table: DBS Targeting and Effects
| Brain Region Targeted | Symptoms Improved | Surgical Procedure | Potential Side Effects |
|---|---|---|---|
| Subthalamic Nucleus | Tremors, rigidity, bradykinesia (slow movement) in Parkinson’s disease | Precise surgical implantation of electrodes into the subthalamic nucleus under MRI guidance. | Headache, infection, bleeding, stroke, speech difficulties, dysphagia, dyskinesias (involuntary movements), cognitive impairment, and mood changes. |
| Globus Pallidus Interna | Tremors, rigidity, bradykinesia (slow movement) in Parkinson’s disease, dystonia (sustained muscle contractions) | Precise surgical implantation of electrodes into the globus pallidus interna under MRI guidance. | Headache, infection, bleeding, stroke, speech difficulties, dysphagia, dyskinesias (involuntary movements), cognitive impairment, and mood changes. |
| Ventral Intermediate Nucleus (thalamus) | Tremors, pain, and other symptoms in essential tremor, dystonia, and other movement disorders | Precise surgical implantation of electrodes into the ventral intermediate nucleus (thalamus) under MRI guidance. | Headache, infection, bleeding, stroke, speech difficulties, dysphagia, dyskinesias (involuntary movements), cognitive impairment, and mood changes. |
| Anterior Nucleus (thalamus) | Obsessive-compulsive disorder (OCD) symptoms | Precise surgical implantation of electrodes into the anterior nucleus (thalamus) under MRI guidance. | Headache, infection, bleeding, stroke, speech difficulties, dysphagia, dyskinesias (involuntary movements), cognitive impairment, and mood changes. |
Types of Deep Brain Stimulation (DBS)
Deep brain stimulation (DBS) devices have evolved significantly, offering diverse options tailored to specific neurological conditions and patient needs. Understanding the different types, their functionalities, and surgical approaches is crucial for optimizing treatment outcomes. This exploration will delve into the various DBS devices, stimulation parameters, and surgical procedures.
DBS Device Types and Functionalities
Different DBS systems offer various features. Some systems are designed for single-target stimulation, while others allow for simultaneous stimulation of multiple targets. This flexibility is important for treating complex neurological conditions. The device typically comprises an implanted pulse generator (IPG), which delivers electrical impulses to the targeted brain region. The IPG contains a battery that powers the device, and wires (leads) connect the IPG to the electrodes implanted in the brain.
Stimulation Parameters and Effects, Deep brain stimulation dbs
Stimulation parameters are critical for achieving optimal therapeutic effects. These parameters include pulse width, pulse frequency, and voltage. Pulse width refers to the duration of each electrical pulse. Pulse frequency describes how often these pulses are delivered. Voltage indicates the intensity of the electrical current.
Each parameter has a distinct effect on the neural activity. Adjustments in these parameters are often made through programming sessions to fine-tune the stimulation and minimize side effects. For instance, adjusting the frequency of stimulation can significantly improve tremor control. Proper parameter selection and careful monitoring are vital for minimizing potential complications.
Surgical Approaches for DBS Implantation
Various surgical approaches are used for DBS implantation, each with its own advantages and considerations. The most common approach involves stereotactic surgery, guided by advanced imaging techniques. This approach allows surgeons to precisely target the specific brain region requiring stimulation. The procedure involves creating small openings in the skull to implant the electrodes and connecting them to the IPG.
The choice of surgical approach depends on the individual patient’s anatomy and the specific condition being treated.
DBS Electrode Types, Materials, and Applications
Different DBS electrode types, materials, and applications are designed to optimize treatment effectiveness and patient safety.
| Electrode Type | Material | Applications |
|---|---|---|
| Micro-electrodes | Platinum-iridium alloys, tungsten | Targeted stimulation of small, precisely defined areas, especially useful in movement disorders. |
| Macro-electrodes | Stainless steel, platinum-iridium alloys | Stimulation of larger brain regions, effective for treating conditions involving widespread neural activity, like Parkinson’s disease. |
| Lead electrodes | Biocompatible polymers, metals | Connecting the pulse generator to the brain targets. These vary in length and shape, depending on the patient’s anatomy and the targeted brain region. |
These electrodes are meticulously designed to ensure minimal tissue damage during implantation and long-term compatibility with the body.
Applications of Deep Brain Stimulation (DBS)
Deep brain stimulation (DBS) has emerged as a powerful therapeutic tool for a range of neurological and psychiatric disorders. It involves implanting electrodes in specific brain regions to deliver electrical impulses, modulating neural activity and potentially alleviating debilitating symptoms. This targeted approach allows for precise control over the stimulation parameters, offering a degree of personalization in treatment. DBS is not a cure, but rather a means of managing symptoms and improving quality of life for those affected.DBS targets specific brain regions implicated in various neurological and psychiatric conditions, aiming to restore or normalize disrupted neural pathways.
Its efficacy is highly variable and dependent on numerous factors, including the specific condition, the patient’s individual response, and the expertise of the medical team administering the procedure.
Neurological Conditions Treatable with DBS
DBS is increasingly being used to treat a variety of neurological conditions characterized by motor, cognitive, or sensory impairments. These conditions often involve dysfunctions in specific brain circuits that can be targeted with DBS. Understanding these conditions and their responses to DBS is critical for successful implementation and outcome prediction.
Deep brain stimulation (DBS) is fascinating, isn’t it? While I was researching DBS, I couldn’t help but think about how much my beauty routine in quarantine beauty routine in quarantine changed. It made me realize how much our daily habits can be affected by unexpected circumstances, even those impacting the brain directly. I’m still learning about the nuances of DBS, but I’m hooked on the potential it holds.
- Parkinson’s Disease: DBS can effectively manage motor symptoms like tremors, rigidity, and bradykinesia (slowness of movement). For example, in Parkinson’s patients, DBS targeting the subthalamic nucleus can significantly reduce tremors and improve gait. Other regions like the globus pallidus internus are also targeted for motor symptom control.
- Essential Tremor: This condition, characterized by involuntary tremors, particularly affecting the hands, can be significantly improved with DBS. In these cases, the thalamus is often the target region for DBS. Patients experience a reduction in tremor severity and an improvement in daily activities like eating and writing.
- Dystonia: DBS is a promising treatment option for patients with dystonia, a movement disorder characterized by sustained muscle contractions. By targeting specific brain regions involved in motor control, DBS can alleviate the involuntary muscle spasms and improve the patient’s ability to perform everyday tasks.
- Tourette Syndrome: Although less commonly used, DBS can offer some symptom relief for patients with Tourette syndrome. The focus here is on reducing the severity and frequency of tics, which can significantly improve the patient’s quality of life.
Psychiatric Conditions Treatable with DBS
DBS is increasingly being explored as a treatment option for certain psychiatric disorders, though its application is still evolving and under research.
- Major Depressive Disorder: DBS, particularly targeting the subgenual cingulate cortex, has shown some promise in treating severe, treatment-resistant major depressive disorder. Early studies suggest that DBS may help alleviate symptoms of depression in carefully selected patients. It’s important to note that the effectiveness and safety of DBS in this context remain areas of active research.
- Obsessive-Compulsive Disorder (OCD): DBS, targeting the anterior cingulate cortex or other specific brain regions, has shown some potential in managing severe, treatment-resistant OCD. Research suggests that DBS may help reduce the frequency and intensity of obsessions and compulsions, improving the patient’s overall well-being.
Effectiveness in Different Patient Populations
The efficacy of DBS varies significantly across different patient populations, depending on factors like the severity of the condition, the patient’s age, and their overall health. Factors like pre-operative functional abilities and post-operative follow-up are also critical to assess the impact.
- Age: DBS can be effective across a broad age range, but the selection criteria and post-operative management need to be tailored to the specific age group. Younger patients might have different expectations and challenges, and thus require a tailored approach.
- Severity of Condition: Patients with more severe conditions might benefit more from DBS, particularly if other treatments have proven ineffective. The extent of improvement is directly correlated to the severity of the condition.
- Individual Response: Response to DBS is highly individualistic, and not all patients experience the same level of improvement. Factors such as pre-existing medical conditions and patient compliance play a significant role.
Comparative Efficacy of DBS for Neurological Disorders
| Neurological Disorder | Targeted Brain Region | Typical Improvements | Effectiveness (High/Medium/Low) |
|---|---|---|---|
| Parkinson’s Disease | Subthalamic Nucleus, Globus Pallidus Internus | Tremor reduction, improved gait, reduced rigidity | High |
| Essential Tremor | Thalamus | Reduced tremor severity, improved daily activities | Medium |
| Dystonia | Globus Pallidus, Thalamus, Subthalamic Nucleus | Reduced muscle spasms, improved function | Medium-High |
| Tourette Syndrome | Various regions, often involving basal ganglia | Reduced tics, improved quality of life | Medium |
Note: Effectiveness ratings are approximate and can vary significantly based on individual patient responses.
Procedure and Surgical Considerations
Deep brain stimulation (DBS) surgery is a complex procedure requiring meticulous planning and execution. The process involves precisely targeting specific brain regions to deliver electrical impulses, modulating abnormal neural activity. This section delves into the surgical steps, pre-operative considerations, imaging techniques, and potential risks associated with DBS implantation.
Surgical Procedure
The DBS surgical procedure is typically performed in stages over several days. A neurosurgeon carefully creates a small opening in the skull to access the targeted brain region. Precise placement of the electrodes is crucial for optimal therapeutic effect. Advanced imaging guides the placement of the electrodes, ensuring that they are located in the desired area. After precise placement, the electrodes are connected to a pulse generator, which is implanted under the skin, usually in the chest area.
The pulse generator delivers the electrical stimulation to the electrodes, thereby modulating neural activity in the target brain region.
Pre-Operative Planning and Patient Preparation
Thorough pre-operative planning is paramount for successful DBS surgery. Neurological evaluations and detailed medical history are vital. Electroencephalography (EEG), magnetic resonance imaging (MRI), and computed tomography (CT) scans are essential for visualizing brain anatomy and identifying any pre-existing abnormalities. Furthermore, careful assessment of the patient’s cognitive function and mental health is crucial. Pre-operative psychological evaluation and counseling are also important for managing expectations and minimizing potential anxiety.
Deep brain stimulation (DBS) is a fascinating procedure that can significantly improve quality of life for those with neurological conditions. Choosing the right equipment, like the best convertible car seat for your child, can also impact your family’s comfort and safety. Thankfully, resources like best convertible car seat reviews can make the process easier. Ultimately, whether it’s selecting the optimal DBS parameters or the right car seat, thoughtful consideration and research are key.
Patients must be adequately informed about the procedure, potential risks, and benefits to allow for informed consent.
Imaging Techniques
Various imaging techniques play a critical role in guiding DBS surgery. Stereotactic frame-based systems are frequently used to precisely locate the target area in the brain. Frameless stereotactic systems, an alternative, offer increased patient comfort and reduce the risk of complications associated with frame placement. MRI and CT scans provide detailed anatomical information, aiding in the localization of the target region.
Intraoperative MRI, which allows for real-time imaging during the surgery, provides further guidance in confirming the electrode placement.
Potential Complications and Risks
| Potential Complications | Description |
|---|---|
| Hemorrhage | Bleeding at the surgical site, potentially leading to swelling and pressure on the brain. |
| Infection | Bacterial or viral infection at the surgical site, potentially requiring antibiotic treatment. |
| Stroke | Disruption of blood flow to the brain, leading to neurological deficits. |
| Intracranial Hematoma | Collection of blood within the skull, potentially compressing brain tissue. |
| Electrode Displacement | Shifting of the electrodes from the intended location, potentially leading to ineffective stimulation or damage to adjacent brain tissue. |
| Lead Fracture | Breaking of the electrode leads, rendering them ineffective. |
| Neuropsychological Effects | Temporary or permanent changes in cognitive function, mood, or behavior. |
| Speech or Swallowing Difficulties | Transient or lasting difficulties with speech or swallowing. |
| Device Malfunction | Battery failure, programming errors, or other device issues. |
These complications are rare, but patients should be fully informed about them prior to consenting to the procedure. Careful surgical technique, meticulous pre-operative planning, and ongoing post-operative monitoring significantly minimize the risk of complications.
Post-Operative Care and Management: Deep Brain Stimulation Dbs
Deep brain stimulation (DBS) surgery, while highly effective, necessitates meticulous post-operative care. This crucial period demands a multidisciplinary approach encompassing close monitoring, targeted rehabilitation, and proactive management of potential complications. Patient well-being and optimal outcome hinge on a comprehensive and individualized post-operative strategy.
Importance of Post-Operative Follow-Up and Rehabilitation
Post-operative follow-up appointments are vital for assessing the patient’s recovery, adjusting stimulation parameters, and addressing any emerging issues. Regular evaluations allow for early detection and management of complications, ensuring the long-term effectiveness of the DBS system. Rehabilitation plays a critical role in restoring functional independence and quality of life. This encompasses physical therapy to regain motor skills, occupational therapy to adapt to daily activities, and speech therapy to address communication challenges if relevant.
Individualized plans are essential to cater to each patient’s specific needs and recovery trajectory.
Monitoring of Stimulation Parameters and Adjustments
Precise monitoring of stimulation parameters is crucial post-operatively. Changes in the patient’s condition can necessitate adjustments to the voltage, pulse width, and frequency of stimulation. Neurologists use sophisticated equipment to track brain activity and stimulation delivery, enabling them to fine-tune the therapy for optimal results. These adjustments are performed iteratively, guided by ongoing assessments of symptom improvement or deterioration.
Deep brain stimulation (DBS) is a fascinating procedure, but it’s crucial to remember that a healthy lifestyle is key to any treatment’s success. For example, while DBS can help manage certain neurological conditions, a balanced diet, including limiting red and processed meats, as detailed in this excellent piece on red meat processed meat is still bad for your health , is still essential for overall well-being.
So, even with DBS, prioritizing a nutritious diet remains vital for a positive outcome.
Regular assessments and adjustments are essential for maintaining therapeutic efficacy and minimizing potential side effects.
Potential Post-Operative Complications
A range of complications can arise following DBS surgery. These can span from minor discomfort to more serious issues. These potential complications can include: infection at the incision site, bleeding, hematoma formation, stroke, seizures, and temporary or permanent neurological deficits. Careful monitoring and prompt intervention are essential for minimizing the risk and severity of these complications.
Post-Operative Therapies
A variety of therapies can be employed to support the patient’s recovery. These therapies are tailored to the individual needs and recovery stage of the patient.
| Type of Therapy | Description | Example |
|---|---|---|
| Physical Therapy | Focuses on regaining motor skills, improving range of motion, and enhancing strength. This often involves exercises, gait training, and assistive devices. | Range of motion exercises, strengthening exercises, balance training. |
| Occupational Therapy | Aims to improve daily living skills and adapt to activities of daily living. This may include adapting the home environment, teaching assistive techniques, and improving self-care abilities. | Modifying home environment, teaching adaptive techniques, improving self-care. |
| Speech Therapy | Addresses communication difficulties and swallowing problems that might arise as a result of the surgery or its effect on the patient. | Improving speech clarity, managing swallowing difficulties. |
| Psychological Support | Addresses emotional well-being and coping strategies associated with the surgery and its effects. This can include counseling and support groups. | Counseling, support groups, stress management techniques. |
Ethical Considerations in DBS
Deep brain stimulation (DBS) presents a powerful therapeutic tool, but its application raises complex ethical considerations. The profound impact on patients’ lives, coupled with the invasive nature of the procedure, necessitates a careful examination of the ethical principles governing its use. These principles guide the responsible development and implementation of DBS technology, ensuring patient well-being and societal benefit.The ethical landscape surrounding DBS is multifaceted, encompassing patient autonomy, potential for misuse, and societal implications.
This exploration delves into these critical areas, highlighting the challenges and potential solutions involved in navigating the ethical complexities of DBS.
Patient Consent and Informed Decision-Making
Informed consent is paramount in any medical procedure, and DBS is no exception. Patients undergoing DBS must fully comprehend the procedure, potential risks and benefits, and alternative treatments. This necessitates clear and accessible communication from medical professionals. Furthermore, patients’ autonomy must be respected throughout the decision-making process. They should be empowered to make choices aligned with their values and preferences, even if those choices differ from the recommendations of medical professionals.
This includes the right to refuse treatment. The process of informed consent must also address potential cognitive impairments that might affect a patient’s ability to comprehend the information presented.
Societal Implications of DBS Technology
DBS technology’s potential for enhancing human capabilities raises societal concerns. The possibility of “cognitive enhancement” through DBS has ethical implications for equality and access. Unintended consequences of widespread DBS use, such as social stratification based on access to the technology, need careful consideration. Furthermore, the potential for misuse, such as using DBS for non-therapeutic purposes, necessitates strict regulations and ethical guidelines.
The potential for altering human behavior through DBS warrants ongoing dialogue and research.
Ethical Frameworks Surrounding DBS
Different ethical frameworks offer diverse perspectives on the use of DBS. Utilitarianism, emphasizing the greatest good for the greatest number, could support DBS if its benefits outweigh the risks for a substantial portion of the population. Deontology, focusing on moral duties and rights, necessitates a strong emphasis on respecting patient autonomy and avoiding potential harms. Virtue ethics, centering on character and moral excellence, encourages medical professionals to practice DBS with compassion, integrity, and a commitment to patient well-being.
Ethical Concerns in DBS Procedures
| Ethical Concern | Explanation | Examples |
|---|---|---|
| Patient Autonomy | Ensuring patients have the right to make informed decisions about their treatment, including the right to refuse treatment. | Patients with cognitive impairments might require support in understanding the procedure and its implications. |
| Potential Misuse | The potential for using DBS for non-therapeutic purposes, such as enhancing cognitive abilities for competitive advantage. | Strict regulations and oversight are necessary to prevent unethical use. |
| Equity and Access | Ensuring equitable access to DBS technology and addressing potential disparities in access based on socioeconomic factors. | Public health initiatives and subsidies could help to ensure more widespread access. |
| Long-Term Effects | Understanding the long-term effects of DBS on brain function and behavior. | Longitudinal studies are needed to fully understand potential impacts. |
| Informed Consent for Future Use | Addressing the ethical considerations of consent for research and potential future uses of DBS technology. | Developing clear protocols and informed consent procedures for research involving DBS. |
Future Directions in DBS
Deep brain stimulation (DBS) has revolutionized the treatment of neurological and movement disorders. While current applications are highly effective, ongoing research and development promise even greater precision, safety, and therapeutic potential. The future of DBS hinges on innovative technologies and a deeper understanding of the complex neural circuits involved.
Advanced Stimulation Techniques
Emerging techniques in DBS are focusing on optimizing stimulation parameters beyond the traditional constant-current approach. These advancements aim to improve treatment efficacy and reduce side effects. Variable stimulation, adaptive stimulation, and closed-loop stimulation are examples of these innovative approaches. Variable stimulation involves adjusting the stimulation parameters based on real-time physiological data, potentially leading to more personalized and effective treatments.
Adaptive stimulation can dynamically modify the stimulation parameters in response to the patient’s changing condition, providing a more responsive and adaptive therapeutic strategy. Closed-loop DBS systems, utilizing real-time monitoring and feedback, could offer even greater precision and reduce the risk of side effects by adjusting stimulation according to the patient’s brain activity.
Neuroimaging and Targeting
Precise targeting is crucial for successful DBS. Improvements in neuroimaging techniques are enhancing our ability to visualize and understand the brain’s intricate structures and networks. Advanced MRI, fMRI, and diffusion tensor imaging (DTI) are being utilized to create highly detailed 3D models of the brain, allowing for more precise targeting and minimizing the risk of unintended side effects.
The integration of these advanced imaging techniques with DBS allows for real-time adjustments during the procedure, enabling surgeons to optimize targeting and minimize damage to healthy brain tissue. This also allows for individualized treatment plans tailored to each patient’s unique brain anatomy and pathology.
Neuromodulation beyond Movement Disorders
The potential applications of DBS extend beyond movement disorders. Researchers are exploring its use in treating a broader range of neurological and psychiatric conditions, including depression, obsessive-compulsive disorder (OCD), and addiction. Preliminary studies show promising results in these areas, suggesting a wider therapeutic window for DBS. This could lead to the development of novel therapies for conditions that currently lack effective treatment options.
Further research is needed to validate these promising findings and establish DBS as a viable treatment for these conditions.
Key Research Areas in DBS
| Research Area | Potential Future Developments |
|---|---|
| Advanced Stimulation Techniques | Variable stimulation, adaptive stimulation, closed-loop stimulation, and personalized stimulation protocols. |
| Neuroimaging and Targeting | High-resolution neuroimaging techniques (e.g., advanced MRI, fMRI, DTI), real-time feedback systems, and individualized treatment plans. |
| DBS for Non-Movement Disorders | Treating depression, OCD, addiction, and other neurological and psychiatric conditions. |
| Implantable Devices | Miniaturization, wireless technology, and biocompatible materials for enhanced safety and patient comfort. |
| Biofeedback and Machine Learning | Integration of biofeedback and machine learning algorithms to optimize stimulation parameters and personalize treatments. |
Patient Experiences and Quality of Life
Deep brain stimulation (DBS) offers a transformative opportunity for individuals grappling with neurological disorders. While the surgical procedure and subsequent recovery are significant, the true impact of DBS lies in the profound changes it can bring to patients’ lives, positively impacting their quality of life and overall well-being. This section explores the diverse patient experiences, highlighting both the remarkable improvements and the challenges encountered during this journey.Understanding the patient’s perspective is crucial in evaluating the efficacy and impact of DBS.
Their experiences, from pre-operative anticipation to post-operative adjustments, shape the overall success story of this innovative treatment. Challenges and concerns, along with the intricate role of family dynamics and support systems, will also be examined.
Patient Experiences with Improvements in Quality of Life
DBS has demonstrably improved the quality of life for many patients. This improvement is multifaceted, impacting various aspects of daily functioning. For instance, individuals with Parkinson’s disease often experience significant reductions in tremors and rigidity, enabling them to perform activities of daily living with greater ease and independence. Similarly, those with dystonia may find relief from painful muscle spasms, leading to a more comfortable and functional existence.
These improvements are often accompanied by enhanced emotional well-being and a greater sense of control over their lives.
Common Challenges and Concerns of Patients Undergoing DBS
While DBS offers significant benefits, patients may encounter various challenges. Common concerns include the need for ongoing monitoring and adjustments to the device settings, the potential for side effects such as speech difficulties or cognitive changes, and the psychological adjustment to a chronic medical condition. These challenges can be addressed through open communication with healthcare professionals and a strong support system.
Proper management and proactive strategies for coping with these side effects can greatly improve the patient experience.
Impact of DBS on Family Dynamics and Support Systems
The impact of DBS extends beyond the individual patient to encompass family dynamics and support systems. The surgical procedure and the ongoing care requirements often necessitate significant adjustments within the family structure. Family members may need to adapt to the patient’s changing needs and provide emotional and practical support. Strong communication and understanding between the patient, family members, and healthcare providers are essential for a successful outcome.
Support groups and resources dedicated to DBS patients and their families can play a crucial role in navigating these challenges.
Case Studies of Patients with Various Conditions
| Patient Condition | Initial Symptoms | DBS Outcome | Quality of Life Improvement |
|---|---|---|---|
| Parkinson’s Disease | Severe tremors, rigidity, bradykinesia | Significant reduction in tremors and rigidity, improved motor skills | Improved mobility, increased independence in daily activities, enhanced participation in social events |
| Essential Tremor | Intense hand tremors, impacting daily tasks | Significant reduction in tremor severity, enabling improved dexterity | Improved hand function, allowing for improved fine motor skills and resumption of hobbies |
| Dystonia | Painful muscle spasms, limiting mobility | Reduction in muscle spasms, improved mobility and range of motion | Increased comfort and ease of movement, enabling improved participation in social and physical activities |
“The patient’s experience is paramount in the success of DBS. A multidisciplinary approach that considers the patient’s physical, emotional, and social needs is crucial.”
The table above showcases examples of positive outcomes following DBS procedures. Each case represents a unique journey, demonstrating the variability of responses to this innovative treatment. The impact of DBS can be profound, altering patients’ lives and restoring a sense of well-being.
Outcome Summary
In conclusion, deep brain stimulation (DBS) stands as a remarkable therapeutic option for a variety of neurological and psychiatric disorders. While presenting surgical risks, DBS offers the potential to significantly improve quality of life for many patients. Further research and advancements in DBS technology are expected to expand its applications and refine its procedures, ensuring even more patients benefit from this transformative treatment.
Ethical considerations will remain paramount as the technology continues to evolve.
