Limiting tumors and infections is a critical area of research, focusing on strategies to prevent and treat these devastating conditions. This exploration delves into various biological mechanisms driving tumor and infection development, examining successful strategies and the hurdles involved. From immunological approaches to targeted therapies and infection control measures, we’ll uncover a multifaceted landscape of treatment options.
This comprehensive guide will examine the intricate interplay of the immune system, therapeutic strategies, and infection control measures in combating these health threats. We’ll explore the science behind these approaches, highlighting clinical trials and emerging trends. Furthermore, we will discuss the ethical considerations and public health implications of these strategies, emphasizing the importance of equitable access.
Introduction to Tumor and Infection Limiting Strategies: Limiting Tumors And Infections
Combating the relentless growth of tumors and infections is a critical aspect of modern medicine. These biological processes, if unchecked, can lead to devastating consequences, from localized tissue damage to systemic failure. Effective strategies to limit their spread are paramount for improving patient outcomes and public health. This exploration delves into the biological underpinnings of tumor and infection development, examines successful interventions, and highlights the considerable challenges involved in curbing their progress.Tumorigenesis and infection, though distinct, share some common threads.
Both involve uncontrolled cellular proliferation and disruption of normal tissue homeostasis. Tumors arise from genetic mutations and epigenetic changes, leading to uncontrolled cell division. Infections, on the other hand, involve the invasion and multiplication of pathogens, which trigger inflammatory responses and tissue damage. Understanding these intricate mechanisms is crucial for developing targeted therapies.
Biological Mechanisms of Tumor Development
The transformation of normal cells into cancerous cells is a multi-step process. Genetic mutations, often caused by environmental factors, can disrupt the regulatory pathways that control cell growth and division. These mutations can activate oncogenes, which promote cell proliferation, or inactivate tumor suppressor genes, which normally restrain cell growth. Accumulation of such mutations creates a cascade of events that eventually leads to uncontrolled cell growth and tumor formation.
Furthermore, epigenetic changes, which modify gene expression without altering the DNA sequence, can also contribute to tumor development.
Biological Mechanisms of Infection Development
Infectious agents, such as bacteria, viruses, fungi, and parasites, invade the body and initiate a complex interplay with the host’s immune system. The pathogen’s ability to evade the immune response, replicate within host cells, and disseminate throughout the body are key factors in infection development. Virulence factors produced by pathogens play a critical role in this process, enabling them to adhere to host cells, invade tissues, and evade the immune system.
Successful Strategies to Limit Tumor Growth
Various strategies have demonstrated success in limiting tumor growth. Surgical removal, often combined with radiation therapy and chemotherapy, remains a cornerstone of cancer treatment. Targeted therapies, which specifically attack cancer cells while minimizing harm to healthy tissues, are revolutionizing cancer treatment. Immunotherapy, which harnesses the power of the immune system to fight cancer, is an emerging field with promising results.
Challenges in Limiting Tumor and Infection Spread
Despite significant progress, several challenges persist in limiting tumor and infection spread. Tumor heterogeneity, the diverse characteristics of cancer cells within a single tumor, makes treatment difficult. Drug resistance, the ability of cancer cells to adapt and resist the effects of treatment, is a significant hurdle. Infectious agents can rapidly evolve, developing resistance to existing treatments. The complexity of the human immune response and the intricate interplay between pathogens and the host add further layers of difficulty.
Table of Tumor and Infection Types
| Tumor Type | Characteristics | Potential Treatments |
|---|---|---|
| Carcinoma | Originates from epithelial cells; most common type. | Surgery, radiation, chemotherapy, targeted therapy, immunotherapy |
| Sarcoma | Originates from connective tissues (bone, muscle, cartilage). | Surgery, radiation, chemotherapy, targeted therapy |
| Leukemia | Cancer of the blood and bone marrow. | Chemotherapy, bone marrow transplant |
| Lymphoma | Cancer of the lymphatic system. | Chemotherapy, radiation, immunotherapy |
| Bacterial Infections | Caused by bacteria; can range from mild to severe. | Antibiotics |
| Viral Infections | Caused by viruses; can cause acute or chronic diseases. | Antivirals, supportive care |
| Fungal Infections | Caused by fungi; can affect various organs. | Anti-fungal medications |
Immunological Approaches to Limiting Tumors and Infections
The immune system plays a crucial role in defending the body against foreign invaders, including pathogens and cancerous cells. This intricate network of cells and molecules constantly patrols the body, identifying and eliminating threats. Understanding and harnessing these mechanisms can lead to innovative therapies for combating tumors and infections.The body’s immune response is not a simple “on/off” switch.
It is a sophisticated and multifaceted system, capable of distinguishing between self and non-self, and employing various strategies to eliminate threats. These strategies, when properly activated and modulated, can be instrumental in preventing and treating both tumors and infections.
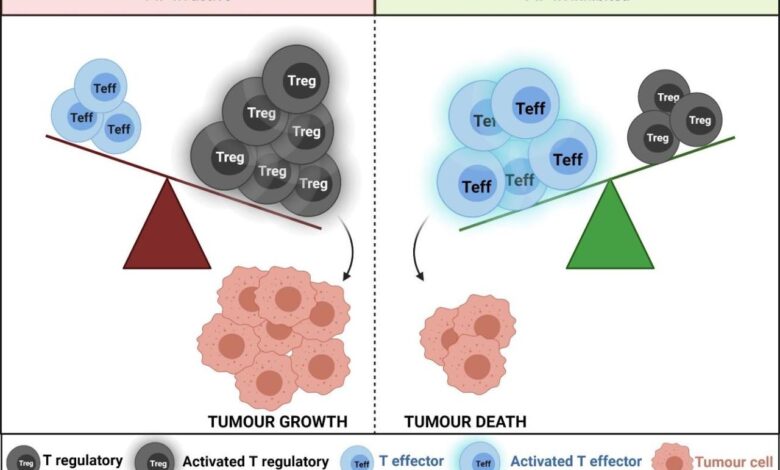
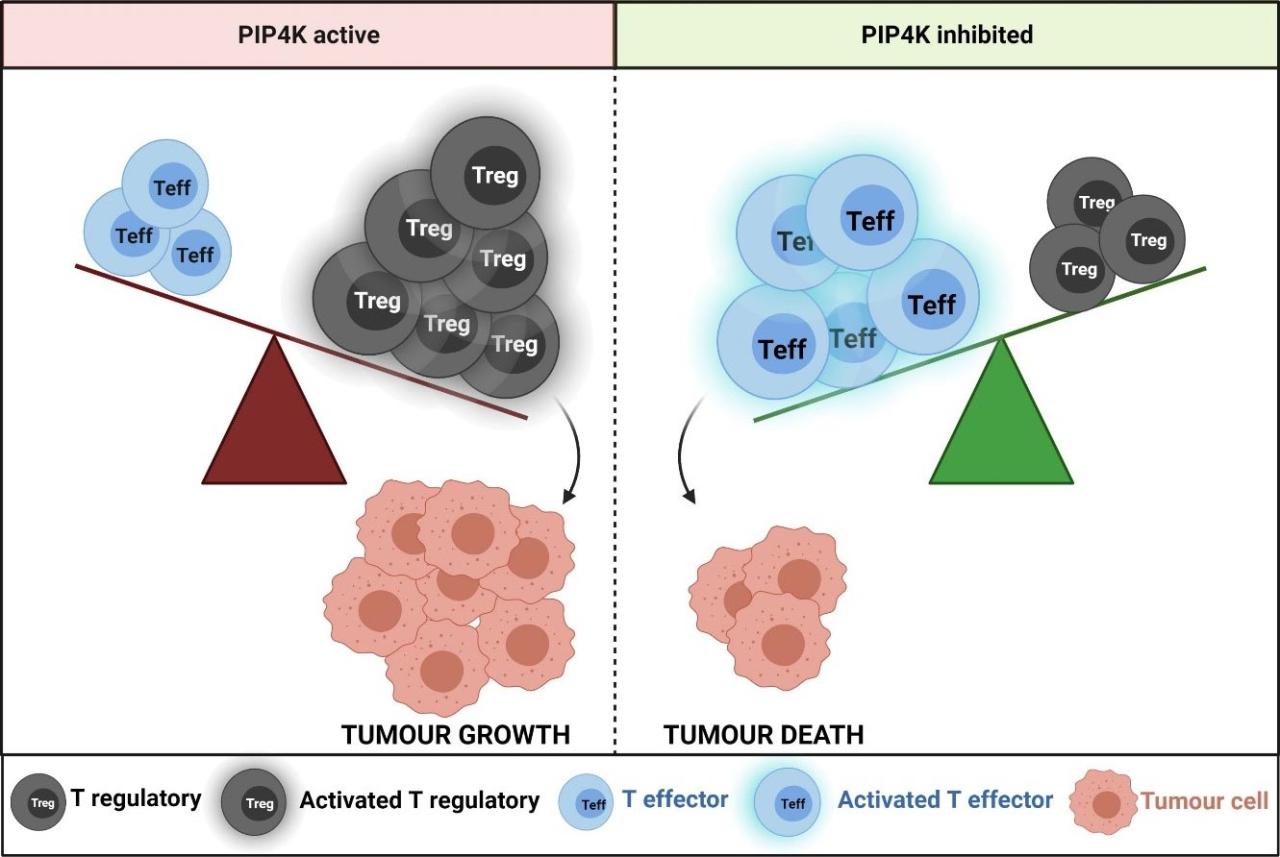
Immune System Recognition and Elimination of Tumors
The immune system employs a variety of mechanisms to identify and eliminate tumor cells. Tumor cells, unlike healthy cells, often display abnormal proteins or molecules on their surface. These “tumor-associated antigens” (TAAs) are recognized by immune cells as foreign entities, triggering an immune response. The immune system’s initial line of defense often involves cytotoxic T lymphocytes (CTLs) that directly kill tumor cells.
Natural killer (NK) cells, another critical component of the immune system, can also recognize and eliminate tumor cells without prior sensitization.
Focusing on limiting tumors and infections is crucial for overall well-being. However, obstacles like systemic issues, particularly the unequal access to mental healthcare, disproportionately affect Black Americans. This significantly impacts their overall health, including the ability to effectively combat conditions like tumors and infections. For more on this critical issue, check out this article on access to mental healthcare is harder for black americans heres why.
Ultimately, addressing these disparities is essential to improving the health outcomes of all communities, and in turn, limiting tumors and infections.
Immune Responses Against Infections
The immune system employs several key strategies to combat infections. The initial response often involves innate immunity, where macrophages and neutrophils engulf and destroy pathogens. Subsequently, adaptive immunity kicks in, with T cells and B cells playing critical roles. T cells directly attack infected cells, while B cells produce antibodies that neutralize pathogens and mark them for destruction.
The effectiveness of the immune response often depends on the type of pathogen, its virulence, and the individual’s immune status.
Different Types of Immunotherapies
Various immunotherapies are currently used to boost the immune system’s response against tumors and infections. These therapies aim to either enhance the activity of the immune cells or modify the tumor microenvironment to make it more susceptible to immune attack. Examples include checkpoint inhibitors, adoptive cell therapies, and vaccines.
Comparison of Immunotherapies
| Immunotherapy | Mechanism of Action | Efficacy | Limitations |
|---|---|---|---|
| Checkpoint Inhibitors | Block immune checkpoints (e.g., PD-1, CTLA-4) that normally suppress immune responses, thus unleashing anti-tumor T cells. | Effective in some cancers, leading to significant tumor regression in certain patient populations. | Potential for side effects like autoimmune reactions, and not effective in all patients. |
| Adoptive Cell Therapies | Isolate and expand immune cells (e.g., T cells) from a patient’s blood, modify them to enhance their anti-tumor activity, and then infuse them back into the patient. | High efficacy in certain hematological malignancies, offering long-lasting responses. | Complex procedures, high costs, and the need for careful selection of patients. |
| Cancer Vaccines | Stimulate an immune response against specific tumor antigens, thereby promoting the destruction of tumor cells. | Show promise in preventing and treating various cancers, particularly those with identifiable tumor antigens. | Varied efficacy depending on the target antigen and the vaccine design. |
Strategies to Enhance Immune Responses
Several strategies are being explored to enhance immune responses against tumors and infections. These include modifying the tumor microenvironment to make it more susceptible to immune attack, enhancing the presentation of tumor antigens, and combining different immunotherapies for synergistic effects. Research in this area is continuously evolving, leading to new possibilities for improving treatment outcomes.
Therapeutic Strategies Targeting Tumor Growth

Fighting cancer involves a multifaceted approach, and targeting tumor growth is a crucial component. This involves a range of strategies, each with its own mechanisms of action, efficacy profiles, and potential side effects. Understanding these strategies is essential for developing personalized treatment plans and improving patient outcomes.
Chemotherapy
Chemotherapy drugs work by targeting rapidly dividing cells, which includes cancer cells. However, normal cells that divide rapidly, such as those in the hair follicles, bone marrow, and digestive tract, are also affected, leading to side effects. Different chemotherapeutic agents have varying mechanisms of action, such as interfering with DNA replication, damaging cell membranes, or disrupting cell cycle progression.
- Examples of chemotherapy drugs include cisplatin, doxorubicin, and 5-fluorouracil.
- Clinical trials have shown varying degrees of success in different tumor types, demonstrating the importance of personalized treatment strategies.
- Common side effects include nausea, hair loss, fatigue, and myelosuppression (suppression of bone marrow function).
- Strategies to mitigate side effects include antiemetics (to combat nausea), supportive care, and hematopoietic stem cell transplantation (in cases of severe myelosuppression).
Radiation Therapy
Radiation therapy uses high-energy radiation to damage the DNA of cancer cells, thereby inhibiting their growth and proliferation. Different types of radiation, such as X-rays, gamma rays, and proton beams, have different properties and potential side effects. Precise targeting is crucial to minimize damage to surrounding healthy tissues.
- External beam radiation therapy directs radiation from a machine outside the body.
- Internal radiation therapy (brachytherapy) involves placing radioactive materials directly into or near the tumor.
- Clinical trials have demonstrated the effectiveness of radiation therapy in shrinking tumors and controlling cancer progression.
- Potential side effects include fatigue, skin irritation, and damage to healthy tissues in the vicinity of the tumor. Proper shielding and treatment planning minimize these risks.
Targeted Therapies
Targeted therapies aim to exploit specific characteristics of cancer cells, such as abnormal growth signals or specific genetic mutations. These therapies often have fewer side effects compared to chemotherapy or radiation therapy, as they are designed to target cancer cells more specifically.
- Examples include monoclonal antibodies, small molecule inhibitors, and hormone therapies.
- Monoclonal antibodies can bind to specific proteins on the surface of cancer cells, triggering their destruction or inhibiting their growth.
- Small molecule inhibitors can block specific enzymes or pathways crucial for cancer cell growth.
- Clinical trials have shown promising results for targeted therapies in specific cancers, highlighting the potential of personalized medicine.
- Side effects vary depending on the specific targeted therapy, but generally tend to be milder than those associated with chemotherapy.
Table Summarizing Therapeutic Approaches
| Therapeutic Approach | Mechanism of Action | Advantages | Disadvantages |
|---|---|---|---|
| Chemotherapy | Targets rapidly dividing cells | Effective in various cancers, often used in combination | Significant side effects, affects healthy cells |
| Radiation Therapy | Damages cancer cell DNA | Precise targeting, effective for localized tumors | Potential for damage to healthy tissues, treatment duration |
| Targeted Therapies | Exploits specific cancer characteristics | High specificity, often fewer side effects | Limited effectiveness in some cancers, drug resistance |
Strategies for Limiting Infection Spread
Containing the spread of infections is crucial for public health. Effective strategies rely on a multi-faceted approach encompassing vaccination, antimicrobial therapies, infection control measures, and robust hygiene practices. This proactive stance significantly reduces the burden of infectious diseases, preventing outbreaks and mitigating their impact on individuals and communities.
Want to help limit tumors and infections? It’s a complex issue, but focusing on overall well-being plays a huge role. A great way to do this is by incorporating delicious and accessible foods into your diet, like those highlighted in this helpful article about healthy eating, healthy eating refresh not everyone likes raw kale 8 delicious accessible foods that promote overall well being.
By nourishing your body with the right nutrients, you’re essentially bolstering your body’s natural defenses, making it better equipped to fight off these issues. This approach to healthy eating is a powerful tool in the arsenal for limiting tumors and infections.
Vaccination Strategies
Vaccination is a cornerstone of infection prevention. By stimulating the immune system to recognize and respond to specific pathogens, vaccines prime the body for a swift and effective defense. Different types of vaccines employ various strategies, each with its own advantages and limitations.
- Inactivated vaccines utilize killed forms of the pathogen, inducing an immune response without the risk of infection. Examples include inactivated polio vaccine and influenza vaccines.
- Live-attenuated vaccines employ weakened versions of the pathogen, stimulating a robust immune response while posing a minimal risk of causing disease. The MMR vaccine is a prime example of this type.
- Subunit vaccines focus on specific components of the pathogen, such as proteins or polysaccharides, prompting the immune system to recognize and target the pathogen. Hepatitis B vaccine exemplifies this approach.
- Toxoid vaccines target bacterial toxins, neutralizing their harmful effects. The tetanus vaccine is a classic example.
Antimicrobial Therapies
Antimicrobial therapies, including antibiotics, antivirals, antifungals, and antiparasitics, play a critical role in treating established infections. The mechanism of action varies widely depending on the specific class of antimicrobial agent.
- Antibiotics target bacterial cell wall synthesis, protein synthesis, or nucleic acid replication, disrupting essential bacterial functions. Penicillin, for instance, interferes with bacterial cell wall synthesis.
- Antivirals, on the other hand, interfere with various stages of viral replication, such as viral entry, DNA/RNA synthesis, or assembly. Examples include antiviral medications for HIV or influenza.
- Antifungals and antiparasitics use diverse mechanisms to inhibit fungal or parasitic growth, often targeting specific metabolic pathways. The specific mechanisms vary greatly depending on the type of infection and the chosen medication.
Infection Control Measures
Infection control measures are essential in preventing the spread of infections in healthcare settings, communities, and other environments. These measures are aimed at minimizing exposure to infectious agents.
- Hand hygiene, including frequent and thorough handwashing with soap and water or alcohol-based hand sanitizers, is paramount in preventing the transmission of pathogens. This simple practice is highly effective in reducing the risk of infection.
- Proper disinfection and sterilization of surfaces, equipment, and medical instruments are critical in preventing the spread of infection in hospitals and clinics. These procedures eliminate or significantly reduce the number of pathogens on surfaces.
- Isolation of infected individuals is crucial in limiting the spread of highly contagious diseases. This strategy confines the pathogen to a controlled environment, reducing its transmission to susceptible individuals.
- Environmental sanitation plays a critical role in controlling the spread of infectious diseases. Proper waste disposal, water treatment, and vector control are critical in preventing the transmission of diseases through contaminated water or vectors such as mosquitoes.
Emerging Strategies
New approaches are continuously being developed to combat infectious diseases.
- Nanotechnology offers exciting possibilities for targeted drug delivery and enhanced antimicrobial efficacy. Nanoscale materials can be designed to deliver antimicrobial agents directly to infected sites, reducing systemic side effects and increasing effectiveness.
- Novel antiviral agents and therapies are being investigated to combat emerging viral threats, such as COVID-19. These developments include the development of mRNA vaccines, which offer a rapid and effective response to evolving viral strains.
- Combination therapies, using a combination of different antimicrobials, are sometimes employed to enhance efficacy and reduce the development of drug resistance. This approach is particularly important in managing multi-drug resistant pathogens.
Hygiene and Sanitation
Hygiene and sanitation are fundamental to preventing infection spread. Maintaining clean environments and proper waste disposal significantly reduce the risk of pathogen transmission.
Staying on top of research to limit tumors and infections is crucial. It’s inspiring to see the innovative work being done in the field, and I’ve been particularly impressed by some of the insights in recent posts. For a great overview of thought-provoking health-related blogs, check out the best blogs of the year. Ultimately, keeping up with these advancements helps us better understand how to combat these diseases effectively.
- Proper handwashing techniques, regular cleaning of surfaces, and safe food handling practices are essential components of maintaining good hygiene. These practices are critical in preventing the spread of infectious agents.
- Access to clean water and sanitation facilities is crucial in preventing the spread of waterborne diseases. This includes proper sewage treatment and safe water sources.
Effectiveness of Vaccination Strategies
| Vaccination Strategy | Infectious Agent | Effectiveness (e.g., % protection) |
|---|---|---|
| Inactivated Polio Vaccine | Poliovirus | >90% |
| Live-attenuated Measles Vaccine | Measles virus | >95% |
| Subunit Hepatitis B Vaccine | Hepatitis B virus | >95% |
| Toxoid Tetanus Vaccine | Corynebacterium tetani | >90% |
Note: Effectiveness figures can vary depending on factors such as individual immune response and vaccination regimen.
Combination Therapies and Synergistic Effects
Combining different therapies to target tumors and infections can often lead to more effective treatment outcomes than using a single approach. This synergistic effect arises from the complementary actions of various drugs or methods, resulting in a greater impact than the sum of their individual effects. This approach is increasingly employed in oncology and infectious disease management.The principle behind combination therapies is that different treatment modalities can target different aspects of the disease process, exploiting vulnerabilities that a single treatment might miss.
This approach is particularly valuable when dealing with complex diseases like cancer, where multiple genetic and cellular alterations contribute to tumor development, or infectious diseases where multiple mechanisms of infection are involved. By combining therapies that target various aspects of the disease, the probability of success is significantly enhanced.
Potential Benefits of Combination Therapies
Combination therapies offer several potential benefits compared to monotherapy, including increased efficacy, reduced side effects, and improved patient outcomes. Increased efficacy is often achieved by targeting multiple pathways simultaneously, thus overcoming resistance mechanisms and enhancing the overall treatment effect. Reduced side effects can be achieved by lowering the dose of individual drugs while maintaining the same level of therapeutic benefit, minimizing the adverse effects.
This approach is particularly relevant for cancer treatments where the aim is to reduce the burden of side effects without compromising efficacy. Furthermore, the combination of therapies can lead to improved patient compliance due to fewer side effects.
Synergistic Effects in Combination Therapies
Synergistic effects in combination therapies refer to the observed therapeutic benefit exceeding the combined effect of individual components. This phenomenon occurs when the interaction between the components leads to a magnified response compared to the simple addition of their individual effects. The mechanism of synergy is complex and can involve various interactions, such as the inhibition of drug metabolism, the enhancement of drug uptake, or the disruption of specific pathways involved in tumor growth or infection.
Examples of Successful Combination Therapies
Several successful combination therapies have been implemented in clinical settings. For instance, in oncology, chemotherapy regimens often combine different drugs targeting various aspects of cancer cell growth and division. Similarly, in infectious diseases, antibiotic combinations are frequently used to combat bacterial infections and prevent the development of antibiotic resistance. These examples highlight the potential of combining therapies to achieve better outcomes.
Comparison of Different Combination Strategies
Different combination strategies can have varying degrees of effectiveness. Factors influencing the effectiveness of a combination strategy include the compatibility of the drugs, their pharmacokinetic properties, and the specific disease being treated. For example, the optimal combination for a particular type of cancer may differ from the optimal combination for a specific bacterial infection. Therefore, careful consideration of these factors is crucial for developing effective and safe combination therapies.
Table Illustrating Synergistic Effects
| Therapy Combination | Mechanism of Synergy | Tumor/Infection Limiting Effect |
|---|---|---|
| Chemotherapy (e.g., Taxol and Cisplatin) | Synergistic inhibition of tumor cell growth | Enhanced tumor regression and survival rates |
| Antibiotics (e.g., Beta-lactam and Aminoglycoside) | Synergistic inhibition of bacterial growth | Faster resolution of infection and reduced risk of resistance |
| Immunotherapy and Chemotherapy | Enhancement of anti-tumor immune response | Improved cancer control and reduced recurrence |
Emerging Trends and Future Directions
The fight against tumors and infections is constantly evolving, driven by innovative research and technological advancements. We are moving beyond traditional approaches, exploring new strategies and combinations to achieve more effective and personalized treatments. This evolution promises a future with higher success rates and fewer side effects.
Personalized Medicine Approaches
Personalized medicine is transforming cancer and infectious disease treatment. By tailoring therapies to individual patient characteristics, including genetic profiles, immune responses, and tumor microenvironment, we can optimize treatment efficacy and minimize adverse reactions. This approach considers the unique biology of each patient’s disease, leading to more precise and effective treatments. The use of genomic sequencing and proteomic analysis allows for the identification of specific targets for therapeutic intervention, potentially improving outcomes.
Immunotherapy Advancements
Immunotherapy is rapidly advancing as a powerful tool for treating both tumors and infections. New approaches are being developed to enhance the body’s own immune system to recognize and eliminate cancer cells and pathogens. These include checkpoint inhibitors, adoptive cell therapies, and oncolytic viruses. The combination of immunotherapy with other modalities, such as chemotherapy or targeted therapies, is showing promise in enhancing anti-tumor and anti-infective responses.
Further research will likely lead to improved targeting and efficacy of immune-based therapies.
Nanotechnology and Targeted Drug Delivery
Nanotechnology offers promising avenues for developing more targeted and effective drug delivery systems. Nanocarriers can deliver drugs directly to tumor cells or infected sites, minimizing damage to healthy tissues and reducing systemic side effects. These systems can be engineered to release drugs in a controlled manner, maximizing therapeutic efficacy and minimizing the need for high doses. Nanoparticles conjugated with imaging agents allow for real-time monitoring of drug delivery and tumor response, which enhances treatment accuracy.
Artificial Intelligence and Machine Learning
Artificial intelligence (AI) and machine learning (ML) are increasingly being utilized in cancer and infectious disease research. AI algorithms can analyze vast amounts of data, including genomic data, clinical records, and imaging scans, to identify patterns and predict treatment responses. This information can be used to develop personalized treatment plans and predict disease progression. AI tools are also being used to design novel drugs and therapies.
Table: Potential of New Technologies for Personalized Medicine
| Technology | Potential Application in Tumor Limiting | Potential Application in Infection Limiting |
|---|---|---|
| Genomic Sequencing | Identifying specific genetic mutations driving tumor growth, enabling targeted therapies. | Identifying genetic factors contributing to infection susceptibility and severity. |
| Proteomic Analysis | Identifying specific protein targets for therapeutic intervention. | Identifying biomarkers for infection diagnosis and prognosis. |
| Nanotechnology | Targeted drug delivery to tumor cells, minimizing side effects. | Targeted drug delivery to infected sites, minimizing side effects. |
| AI/ML | Predicting treatment responses, developing personalized treatment plans, and identifying novel therapeutic targets. | Predicting infection outcomes, identifying novel therapeutic targets, and developing personalized treatment plans. |
Ethical Considerations and Public Health Implications
Navigating the development and implementation of tumor and infection-limiting strategies necessitates careful consideration of ethical principles and potential public health ramifications. These powerful tools, while promising, demand a thoughtful approach that balances scientific advancements with the well-being of individuals and society as a whole. Ignoring ethical considerations can lead to unintended consequences and undermine public trust in the medical community.
Ethical Considerations in Development
The development of novel therapies must prioritize the safety and well-being of research participants. Rigorous ethical review boards and adherence to established guidelines are crucial. Informed consent, ensuring participants understand the risks and benefits, is paramount. Equitable access to clinical trials is essential, preventing biases that could disproportionately affect certain populations. Furthermore, the potential for exploitation, particularly in vulnerable populations, must be carefully considered and mitigated.
Public Health Implications, Limiting tumors and infections
These strategies have far-reaching public health implications. Successfully limiting tumors and infections could dramatically reduce morbidity and mortality rates, improving overall population health. However, potential unintended consequences must be carefully assessed. These include the potential for resistance development, the emergence of new diseases, and the alteration of existing ecosystems. Furthermore, access to these advanced therapies must be considered from a public health perspective, ensuring equitable distribution across diverse populations.
Equitable Access to Therapies
Ensuring equitable access to innovative tumor and infection-limiting strategies is a critical public health imperative. Factors like socioeconomic status, geographic location, and access to healthcare infrastructure can significantly influence access. Addressing these disparities through policies that promote affordability, accessibility, and culturally sensitive interventions is crucial. For example, telemedicine and mobile health initiatives can help bridge geographical gaps.
Balancing Scientific Advancements with Ethical Considerations
The pursuit of scientific advancement must be tempered by careful ethical reflection. A collaborative approach involving scientists, ethicists, policymakers, and the public is essential. Transparent communication about potential benefits and risks is crucial for informed decision-making. Establishing clear regulatory frameworks and guidelines can help ensure ethical implementation. An example of balancing these considerations is the ongoing debate about gene editing technologies.
The potential for significant advancements in disease prevention must be weighed against the unknown long-term effects and ethical concerns.
Table of Ethical Considerations and Public Health Implications
| Treatment Approach | Ethical Considerations | Potential Public Health Implications |
|---|---|---|
| Immunotherapy | Potential for adverse immune reactions, equitable access to costly treatments, informed consent regarding potential long-term effects. | Improved cancer survival rates, possible emergence of new autoimmune diseases, potential for increased healthcare costs. |
| Targeted Therapies | Potential for drug resistance, cost-effectiveness, and access to personalized medicine for all socioeconomic strata. | Reduced tumor growth, potential for increased healthcare costs, possibility of creating new forms of drug resistance. |
| Antimicrobial Strategies | Antibiotic resistance development, informed consent regarding potential side effects, responsible use to avoid overuse. | Reduced infection rates, potential for antibiotic resistance crisis, importance of promoting responsible use and preventing misuse. |
| Combination Therapies | Synergistic effects and risks, need for extensive testing, potential for drug interactions and complications. | Improved treatment efficacy, possibility of adverse effects, necessity of balancing risks and benefits. |
Final Summary
In conclusion, limiting tumors and infections requires a multi-pronged approach that encompasses immunology, targeted therapies, infection control, and combination strategies. The field is dynamic, with emerging technologies and personalized medicine holding significant promise. Ethical considerations and equitable access are paramount as we strive to develop effective and responsible solutions for combating these global health challenges.