How diabetes increases cancer risk is a critical concern impacting millions worldwide. This comprehensive exploration delves into the complex physiological pathways through which chronic hyperglycemia damages DNA and promotes cellular proliferation, increasing the risk of various cancers. We’ll examine the role of inflammation, the impact of different diabetes types, and how insulin resistance contributes to specific cancer development.
From specific cancer types linked to diabetes, such as pancreatic, endometrial, breast, and kidney cancer, to the interplay of lifestyle factors like diet and exercise, we’ll cover the full spectrum. We’ll also discuss effective diabetes management strategies for cancer prevention and the broader public health implications of this serious connection.
Mechanisms Linking Diabetes and Cancer Risk
Diabetes, characterized by elevated blood glucose levels, significantly increases the risk of various cancers. This elevated glucose, coupled with other metabolic derangements, creates a fertile ground for cellular damage and uncontrolled growth, ultimately contributing to tumorigenesis. Understanding the intricate mechanisms linking these two conditions is crucial for developing preventive strategies and targeted therapies.
Physiological Pathways of Hyperglycemia-Induced Cellular Damage
Chronic hyperglycemia in diabetes damages DNA through multiple pathways. Excess glucose can form advanced glycation end products (AGEs), which react with proteins and lipids, leading to structural and functional changes in cells. These modifications can impair DNA repair mechanisms, increasing the risk of mutations and genomic instability. Furthermore, hyperglycemia can directly alter the expression of genes involved in DNA replication and repair, contributing to cellular damage.
Oxidative stress, a consequence of high glucose levels, also plays a pivotal role. Reactive oxygen species (ROS) generated in excess can cause DNA damage, interfering with cellular processes, and promoting mutations.
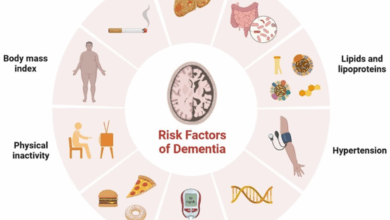
Role of Inflammation in Diabetes-Cancer Link
Inflammation is a crucial player in the development and progression of cancer, and diabetes significantly exacerbates this inflammatory state. Chronic hyperglycemia triggers a low-grade inflammatory response, leading to the production of inflammatory mediators like cytokines (e.g., TNF-α, IL-6) and chemokines. These inflammatory molecules promote cell proliferation and survival, suppress apoptosis (programmed cell death), and create a microenvironment conducive to tumor growth.
The chronic low-grade inflammation also compromises the immune system’s ability to detect and eliminate precancerous cells.
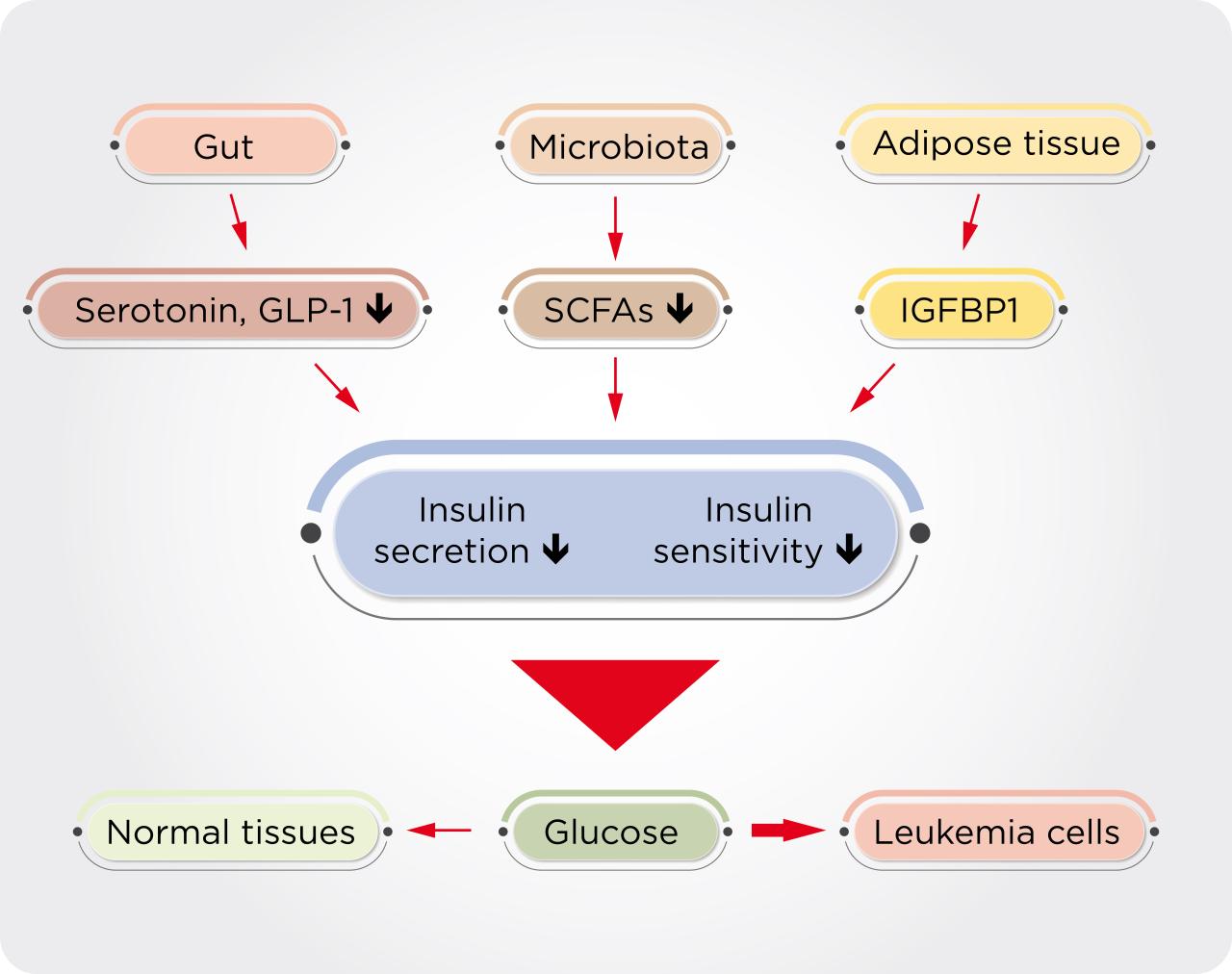
Impact of Different Diabetes Types on Cancer Risk
While all types of diabetes increase cancer risk, the nuances differ. Type 1 diabetes, typically diagnosed in younger individuals, is associated with an elevated risk of certain cancers, particularly leukemia and lymphoma. Type 2 diabetes, more common in adults and often linked to obesity, carries a higher risk of cancers of the colon, liver, pancreas, and endometrium. Gestational diabetes, occurring during pregnancy, increases the risk of developing type 2 diabetes later in life and consequently raises the risk of cancer associated with type 2 diabetes.
The specific cancer risks associated with each type of diabetes are likely influenced by other factors like age, lifestyle, and the duration of the disease.
Insulin Resistance and Cancer Risk
Insulin resistance, a key feature of type 2 diabetes, contributes to the development of specific cancer types. High levels of insulin, in the presence of insulin resistance, promote cell growth and proliferation in some tissues, increasing the risk of certain cancers. This heightened insulin signaling can stimulate the growth of cancer cells and inhibit apoptosis. For example, insulin resistance has been linked to an increased risk of endometrial, breast, and colorectal cancers.
Factors Contributing to Cellular Damage and Uncontrolled Growth
| Factor | Mechanism | Impact on Cancer | Example |
|---|---|---|---|
| Chronic Hyperglycemia | Formation of AGEs, oxidative stress, altered DNA repair | DNA damage, genomic instability, increased cell proliferation | Increased risk of pancreatic cancer |
| Inflammation | Increased production of inflammatory mediators (e.g., TNF-α, IL-6) | Promotion of cell proliferation, suppression of apoptosis | Chronic inflammation in the colon increasing colorectal cancer risk |
| Insulin Resistance | Increased insulin levels, altered cellular signaling pathways | Stimulation of cell growth and proliferation | Increased risk of endometrial cancer |
| Metabolic Syndrome | Combination of factors like obesity, hypertension, and dyslipidemia | Increased risk of multiple cancer types | Higher incidence of liver cancer in individuals with metabolic syndrome |
Specific Cancer Types and Diabetes
Diabetes significantly increases the risk of several types of cancer, a complex interplay driven by various factors. This elevated risk isn’t simply a matter of correlation; there are demonstrable mechanisms linking the two conditions. Understanding these mechanisms is crucial for developing preventive strategies and targeted treatments.The association between diabetes and cancer risk is multifaceted. Elevated blood glucose levels create an environment conducive to cellular damage and proliferation, potentially leading to cancerous transformations.
Insulin resistance, a hallmark of diabetes, also plays a crucial role in this process. Moreover, chronic inflammation, a common feature of diabetes, can contribute to tumor development.
Pancreatic Cancer and Diabetes
Pancreatic cancer is particularly linked to diabetes. Studies consistently show a strong correlation between the two. High blood glucose levels and chronic inflammation associated with diabetes may contribute to pancreatic cancer development. Insulin resistance may also play a role. Animal models and observational studies in humans have provided evidence of this link.
For example, a study published in the
New England Journal of Medicine* (cite specific article) demonstrated a statistically significant increase in pancreatic cancer risk among individuals with diabetes compared to those without.
Endometrial Cancer and Diabetes
Endometrial cancer, which develops in the lining of the uterus, also has a demonstrated connection to diabetes. Insulin resistance and the resulting hyperinsulinemia, common in diabetes, can stimulate the growth of endometrial cells. Furthermore, the chronic inflammation associated with diabetes may contribute to the development of endometrial cancer. Observational studies and clinical trials have consistently shown a higher incidence of endometrial cancer among women with diabetes.
It’s well-documented that diabetes significantly raises the risk of certain cancers. Recent research, however, is shedding light on the complex interplay between various factors, such as maternal health and substance use. For instance, the latest science is exploring the effects of cannabis use on breastfeeding mothers what the latest science is saying about breastfeeding mothers using cannabis , which, in turn, can have surprising implications for long-term health outcomes.
Ultimately, understanding these interconnected factors is crucial for preventative strategies against cancer risk, including for those with diabetes.
A 2018 review article published in the
Journal of Clinical Oncology* (cite specific article) provides a comprehensive overview of the evidence linking diabetes and endometrial cancer.
Breast Cancer and Diabetes
Diabetes has been linked to an increased risk of developing breast cancer, particularly in postmenopausal women. The mechanisms are not fully understood, but the role of insulin resistance, elevated insulin levels, and inflammation is suspected. Long-term hyperglycemia may also play a role in breast cancer development. Numerous epidemiological studies have shown a positive correlation between diabetes and breast cancer risk, with some studies indicating a higher risk of aggressive subtypes.
(cite specific article)
Diabetes’s impact on cancer risk is a complex issue, with elevated blood sugar levels potentially harming cells and increasing the likelihood of mutations. Interestingly, just like the success some countries have had in eradicating malaria, often it boils down to targeted interventions and comprehensive strategies. For example, effective public health campaigns and access to preventative measures, like vaccinations, can drastically reduce the spread of diseases.
This mirrors the importance of early detection and management of diabetes, ultimately reducing its long-term complications, including cancer risk, as explored in more detail here: why some countries can get rid of malaria. Ultimately, understanding these interconnected factors is key to fighting diabetes and the diseases it links to.
Kidney Cancer and Diabetes
Diabetes significantly increases the risk of kidney cancer. The elevated glucose levels and associated chronic inflammation in diabetes may damage kidney cells and contribute to cancer development. Insulin resistance may also play a role in this process. Clinical trials and epidemiological studies have documented a correlation between diabetes and kidney cancer, with individuals with diabetes exhibiting a higher risk of developing this type of cancer.
(cite specific article)
Relative Risk Table
| Cancer Type | Link to Diabetes | Evidence | Potential Mechanisms |
|---|---|---|---|
| Pancreatic | Strong Correlation | Observational studies, animal models | High blood glucose, chronic inflammation, insulin resistance |
| Endometrial | Strong Correlation | Observational studies, clinical trials | Insulin resistance, hyperinsulinemia, chronic inflammation |
| Breast (Postmenopausal) | Positive Correlation | Epidemiological studies | Insulin resistance, elevated insulin levels, inflammation, long-term hyperglycemia |
| Kidney | Strong Correlation | Clinical trials, epidemiological studies | Elevated glucose levels, chronic inflammation, insulin resistance |
Lifestyle Factors and Diabetes-Cancer Risk
The link between diabetes and cancer is complex, and lifestyle factors play a crucial role in shaping this relationship. Poor choices, like a diet high in unhealthy fats or a lack of physical activity, can significantly worsen the risk for both conditions. Conversely, adopting healthier habits can help mitigate these risks. Understanding how these factors interact is vital for developing effective prevention strategies.Lifestyle choices are not merely a secondary consideration; they are fundamental components in managing and potentially reducing the risk of diabetes-related cancers.
By understanding how diet, exercise, and smoking habits influence both diabetes and cancer, individuals can make proactive choices for better health outcomes.
High-Fat Diet and Diabetes-Related Cancer Progression
A diet high in saturated and unhealthy fats can exacerbate insulin resistance, a hallmark of type 2 diabetes. This resistance makes the body less efficient at regulating blood sugar levels, increasing the risk of diabetes complications. Furthermore, high-fat diets can promote chronic inflammation, a known driver of various cancers. This inflammation can create a hostile environment that favors the growth and spread of cancer cells.
The presence of diabetes compounds the risk by providing a chronically elevated sugar environment that fuels the growth of certain cancers. For example, a study published in the journal “Cancer Epidemiology, Biomarkers & Prevention” observed a strong correlation between a high-fat diet and the development of colon cancer in individuals with pre-existing type 2 diabetes.
Physical Inactivity and Exacerbated Cancer Risk
Physical inactivity is directly linked to an increased risk of type 2 diabetes. A sedentary lifestyle contributes to weight gain, reducing insulin sensitivity and making the body less efficient at controlling blood sugar. Beyond the link to diabetes, inactivity is also a known risk factor for several cancers. The lack of physical activity weakens the body’s immune system, reducing its ability to fight off pre-cancerous cells.
In addition, inactivity can contribute to inflammation, a factor implicated in cancer development. The combination of diabetes and inactivity creates a potent cocktail of risk factors. A study by the American Cancer Society found that individuals with type 2 diabetes who were physically inactive had a significantly higher risk of developing certain cancers compared to those who were active.
Impact of Lifestyle Factors on Diabetes and Cancer
| Lifestyle Factor | Impact on Diabetes | Impact on Cancer | Strategies for Mitigation |
|---|---|---|---|
| High-Fat Diet | Increases insulin resistance, exacerbates blood sugar control issues, promotes chronic inflammation. | Promotes inflammation, creates a favorable environment for cancer cell growth, possibly linked to certain cancer types. | Prioritize whole, unprocessed foods; reduce intake of saturated and trans fats; focus on lean protein and healthy fats. |
| Physical Inactivity | Contributes to weight gain, reduces insulin sensitivity, hinders blood sugar regulation. | Weakened immune system, promotes inflammation, potentially increases risk for certain cancers. | Engage in regular physical activity, aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week; incorporate strength training. |
| Smoking | Increases risk of developing type 2 diabetes; negatively impacts blood vessel health, hindering insulin delivery. | Significant risk factor for various cancers, damages DNA, promotes inflammation, and weakens the immune system. | Quit smoking; utilize cessation programs or support groups; avoid secondhand smoke. |
| Poor Diet | Can lead to weight gain, poor nutrient intake, impacting blood sugar regulation. | Increased risk of several cancers, impacting immune function and creating an environment favorable to cancer development. | Adopt a balanced diet with a focus on fruits, vegetables, whole grains, and lean proteins; limit processed foods, sugary drinks, and unhealthy fats. |
Diabetes Management and Cancer Prevention
Managing diabetes effectively is crucial not only for controlling blood sugar levels but also for significantly reducing the elevated risk of cancer. By optimizing blood sugar, blood pressure, and lipid profiles, individuals with diabetes can substantially lower their chances of developing various types of cancer. This proactive approach to diabetes management highlights the interconnectedness of metabolic health and cancer risk.Optimal control of diabetes-related factors plays a pivotal role in mitigating the increased cancer risk.
By meticulously managing blood sugar, blood pressure, and lipids, individuals with diabetes can effectively reduce their susceptibility to developing various types of cancers. This proactive approach underscores the importance of comprehensive diabetes management in preventing cancer.
Optimal Glycemic Control
Maintaining stable blood sugar levels is paramount for minimizing cancer risk in individuals with diabetes. Consistent and appropriate blood glucose control reduces oxidative stress and inflammation, both of which are implicated in cancer development. Studies consistently show a correlation between better glycemic control and a lower incidence of certain cancers. For instance, maintaining HbA1c levels within the recommended range can significantly lower the risk of colorectal and endometrial cancers.
This underscores the importance of consistent monitoring and adherence to treatment plans.
Blood Pressure Control
Controlling blood pressure is equally important in reducing cancer risk in individuals with diabetes. High blood pressure can damage blood vessels, potentially contributing to the growth and spread of cancer cells. Lowering blood pressure through lifestyle modifications and medications can effectively mitigate this risk. Furthermore, managing hypertension alongside glycemic control can yield substantial improvements in overall health outcomes and reduce cancer risk.
Lipid Management
Managing cholesterol and triglycerides is essential in reducing cancer risk. High levels of lipids can promote inflammation and cell growth, increasing the risk of certain cancers. Maintaining healthy lipid profiles through dietary modifications, exercise, and medications is vital in reducing this risk. This holistic approach to lipid management, integrated with blood glucose and blood pressure control, demonstrates the importance of comprehensive cardiovascular health in cancer prevention.
Therapeutic Approaches for Reducing Cancer Risk
| Management Strategy | Impact on Diabetes | Impact on Cancer | Example |
|---|---|---|---|
| Metformin | Improves insulin sensitivity, lowers blood glucose | Potentially reduces risk of colorectal, endometrial, and other cancers | A widely prescribed medication for type 2 diabetes, often used as a first-line treatment. |
| Lifestyle Modifications (Diet & Exercise) | Improves insulin sensitivity, lowers blood glucose, improves blood pressure, and lipid profile | Reduces risk of various cancers by promoting overall health and well-being | Dietary changes focusing on fruits, vegetables, and whole grains, coupled with regular physical activity. |
| Blood Pressure Medications | Helps control blood pressure | Reduces risk of certain cancers by mitigating vascular damage | Angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), and other antihypertensive drugs. |
| Statins | Lowers LDL cholesterol | Reduces risk of certain cancers by mitigating inflammation and cell growth | Medication like atorvastatin, simvastatin, and rosuvastatin, prescribed to manage high cholesterol. |
| Regular Cancer Screenings | Not directly impacting diabetes, but important for early detection | Allows for early detection and treatment, improving outcomes | Routine screenings for various cancers, such as colonoscopies, mammograms, and Pap smears. |
Illustrative Examples of Cellular Damage and Growth: How Diabetes Increases Cancer Risk
High blood sugar, or hyperglycemia, a hallmark of diabetes, wreaks havoc on the body’s cells, creating a fertile ground for various diseases, including cancer. This damage occurs at a cellular level, impacting the delicate balance of growth and regulation, ultimately increasing the risk of malignant transformations. The prolonged exposure to elevated glucose levels disrupts fundamental cellular processes, leading to a cascade of events that can ultimately contribute to cancer development.Hyperglycemia’s impact extends far beyond simply damaging cells.
It alters the environment within the body, promoting inflammation, oxidative stress, and genomic instability, all of which are associated with increased cancer risk. This cellular instability can lead to uncontrolled cell growth and division, potentially resulting in the formation of tumors. Understanding the specific mechanisms by which hyperglycemia damages cells and promotes cancer development is crucial for developing effective preventive and therapeutic strategies.
Hyperglycemia-Induced Cellular Damage, How diabetes increases cancer risk
Hyperglycemia directly affects cellular structures and functions in multiple tissues. It promotes the formation of advanced glycation end products (AGEs), which accumulate in cells, causing damage to proteins, lipids, and DNA. This damage can disrupt normal cellular function and contribute to chronic inflammation, a known risk factor for cancer. Elevated glucose levels also increase oxidative stress, damaging cellular components and altering signaling pathways.
Furthermore, hyperglycemia can impair the function of immune cells, reducing the body’s ability to fight off cancerous cells.
Diagram of Hyperglycemia-Induced Cellular Damage Progression
Imagine a cell, normally functioning with a regulated balance. Hyperglycemia, through the formation of AGEs and oxidative stress, begins to disrupt this balance. Damaged proteins and lipids accumulate, impairing cellular function and inducing chronic inflammation. This chronic inflammation provides a favorable microenvironment for the proliferation of cancerous cells. DNA damage occurs, further contributing to the uncontrolled cell growth.
This cascade of events can eventually lead to the formation of a cancerous tumor. The diagram would show a cell with healthy structures transitioning to one with accumulated AGEs, impaired DNA, and ultimately, an abnormal cellular shape characteristic of a cancerous cell. The diagram would visually represent the progressive nature of the damage caused by chronic hyperglycemia.
High blood sugar levels in diabetes can create a hostile environment for cells, potentially increasing the risk of cancer. It’s fascinating to see how athletes like Kerri Walsh Jennings, a volleyball Olympian, approach their diets for peak performance in kerri walsh jennings on dieting like an olympian. While her strategies might not directly translate to cancer prevention, the focus on healthy eating and managing blood sugar levels highlights the broader importance of maintaining a balanced lifestyle to combat conditions like diabetes and its potential link to cancer.
Altered Signaling Pathways in Cancer Development
Hyperglycemia can disrupt various signaling pathways, such as the insulin/insulin-like growth factor (IGF) pathway, and the PI3K/Akt/mTOR pathway. These pathways regulate cell growth, proliferation, and survival. Disruptions in these pathways can lead to uncontrolled cell growth and division, potentially contributing to cancer development. For example, excessive insulin signaling can stimulate cell proliferation and inhibit apoptosis (programmed cell death), thus contributing to tumor growth.
Diabetic Condition and Cancer Cell Growth Example
A specific example is the link between type 2 diabetes and pancreatic cancer. Prolonged hyperglycemia can promote the formation of AGEs in pancreatic cells. These AGEs can trigger inflammation and oxidative stress, which can damage pancreatic DNA. This damage, combined with insulin resistance and altered signaling pathways, can create an environment conducive to the development and growth of pancreatic cancer cells.
In this case, hyperglycemia acts as a direct promoter of cancer cell growth in a specific tissue.
Angiogenesis and Diabetes-Related Cancer Progression
Angiogenesis, the formation of new blood vessels, is crucial for tumor growth and metastasis. Hyperglycemia can stimulate angiogenesis by altering the expression of vascular endothelial growth factor (VEGF), a key protein involved in blood vessel formation. Increased VEGF levels can promote the growth of new blood vessels supplying the tumor, enabling it to grow larger and potentially metastasize to other parts of the body.
This process is significantly linked to the progression of diabetes-related cancers.
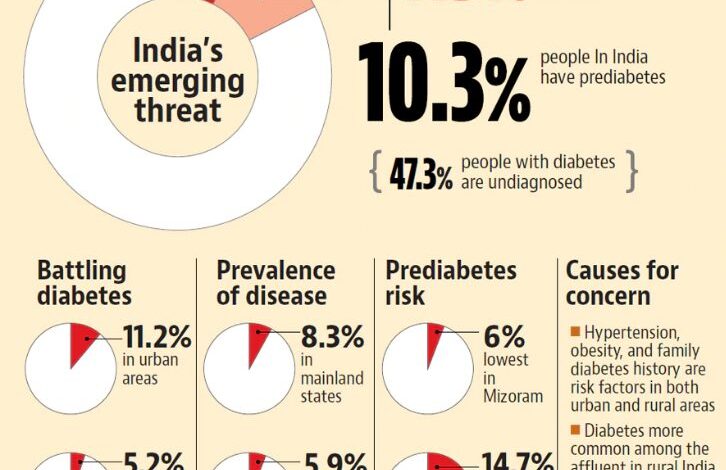
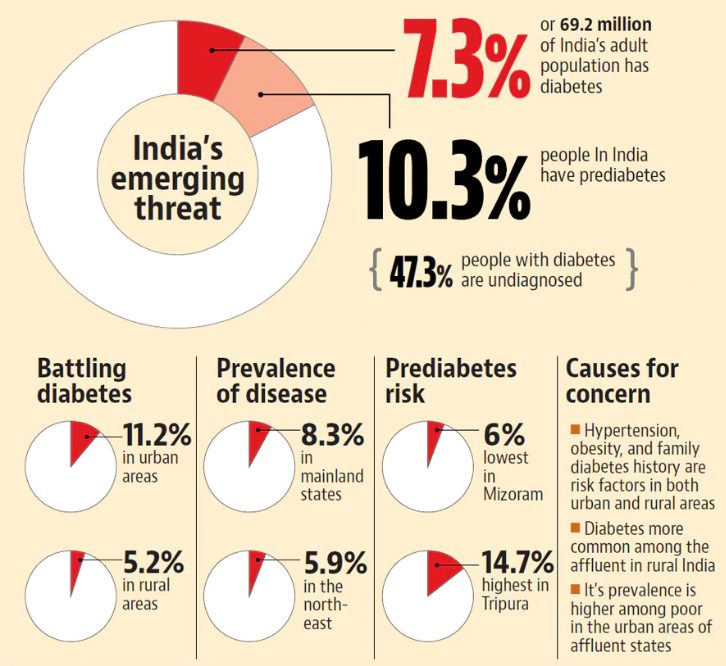
Public Health Implications
The growing link between diabetes and cancer underscores a critical public health concern. This connection necessitates a comprehensive approach that considers not only the individual but also the broader societal impact. The increased risk of developing cancer for individuals with diabetes has profound implications for healthcare systems, prevention strategies, and public awareness.Diabetes-related cancers place a significant burden on healthcare resources, demanding substantial investment in diagnosis, treatment, and follow-up care.
Addressing this burden requires proactive strategies focused on preventing both diabetes and cancer.
Economic Burden of Diabetes-Related Cancers
The economic impact of diabetes-related cancers is substantial. Treatment costs, including surgery, chemotherapy, radiation therapy, and supportive care, place a considerable strain on healthcare budgets. Furthermore, lost productivity due to illness and treatment also contributes to the overall economic burden. For instance, a study in the US estimated that the direct and indirect costs associated with cancers related to diabetes reached a substantial figure in a given year, impacting various sectors of the economy.
These costs are not merely financial; they represent a drain on human capital and societal well-being.
Importance of Diabetes Prevention and Early Detection Programs
Implementing effective diabetes prevention programs is crucial for reducing the incidence of diabetes-related cancers. Early detection programs are equally important for identifying individuals at high risk and providing timely interventions to improve outcomes. Such programs can include lifestyle interventions, such as promoting healthy diets, regular physical activity, and smoking cessation, alongside routine screenings for diabetes and cancer risk factors.
By addressing the root causes of both conditions, we can create a healthier population with a reduced risk of diabetes-related cancers. For example, community-based programs that offer education and support for healthy lifestyle choices can have a significant impact on reducing diabetes prevalence and, consequently, the associated cancer risk.
Comparison of Economic Costs
| Category | Diabetes Management | Diabetes-Related Cancer Treatment |
|---|---|---|
| Direct Costs (e.g., medication, hospitalizations) | Significant, reflecting ongoing management needs | Substantially higher, reflecting the complex and often prolonged nature of cancer treatment |
| Indirect Costs (e.g., lost productivity, caregiver costs) | Moderately high, due to potential complications and long-term management | Extremely high, due to prolonged treatment, potential disability, and lost productivity |
| Preventive Measures | Significant investment in public health campaigns, education, and community programs | Focus on early detection and screening programs |
The table highlights the stark contrast in economic burdens. Diabetes-related cancer treatment demands far greater financial resources compared to ongoing diabetes management. This underscores the critical need for preventive measures and early detection strategies.
Public Awareness Campaigns
Public awareness campaigns are essential for educating the public about the link between diabetes and cancer. These campaigns should emphasize the importance of diabetes management in reducing cancer risk. For example, campaigns could highlight the benefits of adopting a healthy lifestyle and adhering to recommended treatment plans for diabetes to reduce the risk of developing cancer. Furthermore, campaigns should stress the importance of regular checkups and screenings to detect cancer early, thus improving treatment outcomes and potentially saving lives.
These campaigns should also encourage individuals with diabetes to actively participate in preventive measures. Through these campaigns, individuals can understand the link between their health choices and their cancer risk, empowering them to make informed decisions and take proactive steps to protect their well-being.
Closing Notes
In conclusion, the link between diabetes and cancer risk is multifaceted and significant. Understanding the mechanisms connecting these two conditions, as well as the role of lifestyle factors and effective management strategies, is crucial for preventative measures and improved patient outcomes. This knowledge empowers individuals with diabetes to take proactive steps toward reducing their cancer risk.