6 things people living with alzheimers want you to know, a profound look at the daily realities of this challenging condition. This isn’t just about facts and figures; it’s about understanding the lived experience of those affected.
This article delves into six crucial aspects of living with Alzheimer’s: understanding the varying stages, fostering meaningful communication, respecting dignity and independence, navigating behavioral changes, accessing support networks, and ultimately, enhancing quality of life. Each section is designed to offer practical insights and compassionate strategies for those navigating this journey alongside someone with Alzheimer’s.
Understanding the Alzheimer’s Experience
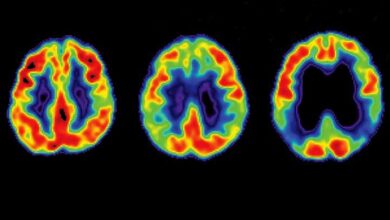
The journey of living with Alzheimer’s disease is profoundly challenging, not only for the individual but also for their loved ones. It’s a progressive neurodegenerative disorder that gradually erodes cognitive functions, impacting memory, thinking, and behavior. This gradual decline necessitates a multifaceted understanding of the daily struggles and the emotional toll it takes.This exploration delves into the intricacies of the Alzheimer’s experience, shedding light on the daily challenges, emotional impact, common misconceptions, and the varying stages of the disease.
Understanding these facets is crucial for providing support and fostering empathy for those affected.
Daily Challenges Faced by Individuals with Alzheimer’s
The daily life of someone with Alzheimer’s is often characterized by a struggle with fundamental tasks. Simple activities that most of us take for granted, like remembering appointments, managing finances, or even recognizing familiar faces, become increasingly difficult. Confusion, disorientation, and difficulty with communication frequently arise. The loss of independence is a significant challenge, impacting self-esteem and creating a reliance on others.
Emotional and Psychological Impact
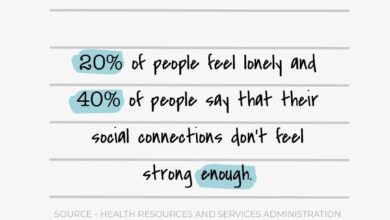
Alzheimer’s disease profoundly affects the emotional well-being of both the individual and their family. The individual experiences a progressive loss of identity as their cognitive abilities diminish. This can lead to feelings of frustration, anxiety, and depression. The family members are often burdened by the emotional strain of caregiving, which can encompass a spectrum of feelings, including stress, grief, and isolation.
Common Misconceptions about Alzheimer’s
Many misconceptions surround Alzheimer’s disease, often perpetuating inaccurate beliefs and hindering proper understanding. One common misconception is that memory loss is the sole symptom. In reality, Alzheimer’s affects various cognitive functions, impacting language, judgment, and reasoning. Another misconception is that it only affects older adults. While the majority of cases occur in later life, early-onset Alzheimer’s can affect individuals in their 30s, 40s, or 50s.
A key misunderstanding involves attributing normal age-related forgetfulness to Alzheimer’s; these are distinct phenomena.
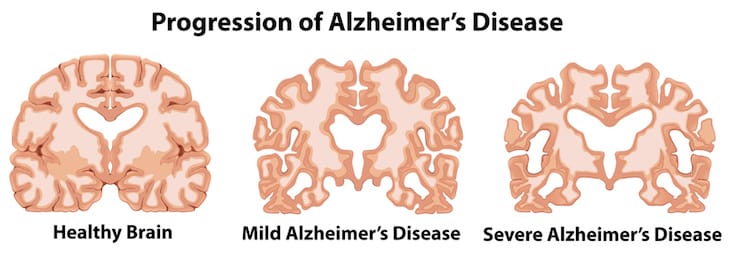
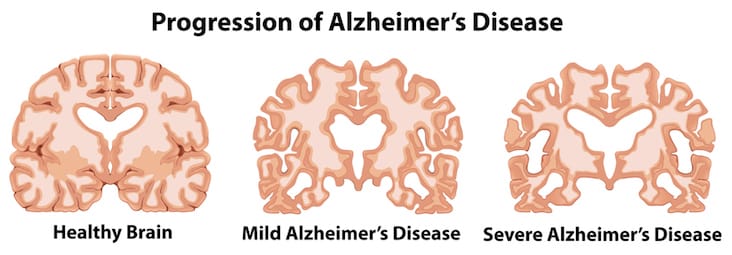
Stages of Alzheimer’s Disease
The progression of Alzheimer’s is often categorized into early, middle, and late stages, each presenting unique challenges and needs.
| Stage | Cognitive Function | Behavioral Changes | Specific Needs |
|---|---|---|---|
| Early Stage | Mild memory loss, difficulty with planning, and word-finding problems. Slight personality changes, such as increased irritability or anxiety. | Increased frustration and confusion, difficulty managing finances, and potential social withdrawal. | Support with daily tasks, medication management, and memory aids. Maintaining social connections and emotional support. |
| Middle Stage | Significant memory loss, disorientation, and difficulty with language. Changes in personality and behavior, such as aggression, agitation, and wandering. | Increased reliance on caregivers, difficulty with self-care, and potential behavioral issues. | Structured routines, safety measures to prevent wandering, and tailored communication strategies. Specialized caregiving support and respite care. |
| Late Stage | Severe memory loss, inability to communicate effectively, and complete dependence on others. Significant behavioral changes, including loss of motor skills, and potential physical decline. | Total reliance on caregivers for all aspects of daily life, increasing risk of infections, and vulnerability to injuries. | Specialized care facilities, palliative care, and comfort measures to manage pain and discomfort. Emotional support for caregivers. |
Communication and Connection
Connecting with someone living with Alzheimer’s can be profoundly rewarding, even when communication takes on new forms. It’s about recognizing that, despite cognitive changes, the person’s inherent worth and desire for connection remain. This requires patience, understanding, and a willingness to adapt communication styles. We’ll explore how to foster meaningful connections and navigate the evolving challenges of communication.Effective communication with individuals living with Alzheimer’s is not about simply transmitting information; it’s about creating a space where they feel seen, heard, and valued.
It requires recognizing that their communication methods might differ, and adjusting our own approaches to facilitate connection. This approach involves acknowledging the impact of the disease on their ability to communicate, while still maintaining a respectful and empathetic environment.
Clear and Respectful Communication
Clear and respectful communication is paramount. Avoid abrupt changes in conversation or using overly complex language. Speak slowly, clearly, and use simple, straightforward sentences. Maintain a calm and reassuring tone, focusing on empathy and understanding. Using visual aids, such as pictures or gestures, can also enhance communication and aid comprehension.
Strategies for Effective Communication
Several strategies can improve communication with individuals living with Alzheimer’s. Active listening is crucial, paying attention not just to words but also to non-verbal cues. Maintain eye contact (when appropriate), use gentle touch, and provide ample time for responses. Remembering past conversations and experiences can help maintain a sense of continuity and familiarity. Focus on feelings and emotions, rather than solely on factual information.
Learning about the 6 things people living with Alzheimer’s want you to know is incredibly important. It’s all about understanding their needs and creating a supportive environment. Thinking about fun toddler birthday party games can help you relate to the challenges of creating a comfortable and engaging experience for a child, which can mirror the need for patience and understanding when interacting with someone living with Alzheimer’s.
For more ideas on engaging toddler birthday party games, check out this helpful resource: toddler birthday party games. Ultimately, remembering these 6 crucial points is key to making a positive impact on those living with Alzheimer’s.
Emphasize the importance of maintaining eye contact and a calm demeanor.
Understanding Non-Verbal Cues
Recognizing and responding to non-verbal cues is vital. Changes in facial expressions, body language, or tone of voice can provide valuable insight into how the person is feeling. For instance, if someone appears agitated, a soothing presence and a change in the conversation topic might be more helpful than trying to resolve a complex issue. Being attentive to subtle changes in behavior can help in understanding underlying needs and emotions.
If a person seems frustrated, try to identify the cause and adjust the interaction accordingly.
Thinking about the 6 things people living with Alzheimer’s want you to know? It’s crucial to understand that cognitive decline isn’t always solely due to the disease itself; sometimes, underlying conditions like depression can significantly impact your ability to think clearly. Learning more about how depression can affect your mental sharpness can help you understand the complexities of Alzheimer’s.
For a deeper dive into the connection between depression and cognitive function, check out this insightful article on can depression affect your ability to think. Ultimately, remembering these 6 key points can empower you to be a more supportive and understanding friend or family member.
Building and Maintaining Meaningful Connections
Maintaining meaningful connections is essential. Focus on shared activities, such as listening to music, looking at photos, or engaging in familiar hobbies. These activities can evoke positive memories and emotions. Use reminiscence therapy to tap into past experiences and create shared moments of joy and connection. Encourage participation in social activities, ensuring the environment is supportive and familiar.
This can include joining support groups or activities that focus on shared interests.
Adapting Communication Styles
| Communication Style | Early Stage Alzheimer’s | Moderate Stage Alzheimer’s | Late Stage Alzheimer’s |
|---|---|---|---|
| Direct Questioning | Effective, but keep questions short and simple. | May require simpler, more direct questions. | Focus on nonverbal cues, avoid complex questions. |
| Complex Sentences | Avoid complex sentences. | Use short, simple sentences and phrases. | Focus on single words or phrases. |
| Nonverbal Communication | Important for understanding feelings and emotions. | Nonverbal cues become more important as verbal communication declines. | Nonverbal communication becomes crucial for interaction. |
| Humor | Appropriate, but keep it lighthearted. | Humor might be less effective, but shared memories might evoke laughter. | Focus on simple, familiar expressions of happiness or comfort. |
Maintaining Dignity and Independence
Respecting the dignity and autonomy of individuals living with Alzheimer’s is paramount. This involves acknowledging their inherent worth and recognizing their capacity for self-determination, even as cognitive abilities change. It’s about fostering a supportive environment that allows them to retain a sense of control and agency in their lives. This chapter explores practical strategies to maintain dignity and independence, crucial for the well-being and quality of life of those affected by the disease.Individuals living with Alzheimer’s often experience a progressive decline in cognitive function.
However, their inherent worth and desire for connection and participation remain. Maintaining their dignity and independence is a crucial aspect of compassionate care. This entails creating an environment that empowers them to participate in activities that are meaningful and enjoyable, while also respecting their changing abilities. Encouraging their autonomy in daily tasks fosters a sense of self-worth and promotes their well-being.
Respecting Autonomy and Dignity
Maintaining dignity involves treating individuals with Alzheimer’s with the same respect and consideration that we would extend to anyone else. This includes avoiding patronizing language or actions, and actively listening to their expressed needs and desires. Recognizing and valuing their past experiences, talents, and accomplishments can help foster a sense of self-worth. It’s about creating a supportive environment that allows for meaningful interactions and experiences.
Encouraging Independence in Daily Tasks
Encouraging independence in daily tasks is essential. Break down complex tasks into smaller, manageable steps. Provide clear and concise instructions. Offer visual cues or reminders. For example, instead of telling someone to “take a shower,” provide a visual schedule with pictures of the steps involved.
This promotes independence and reduces frustration. Use familiar routines and environments to minimize disorientation and promote a sense of security.
Promoting Purpose and Engagement
Promoting a sense of purpose and engagement in activities is vital. Activities should be tailored to the individual’s current cognitive abilities and interests. These activities could include hobbies they previously enjoyed, or new activities that spark interest. This might involve listening to music, engaging in light exercise, or simply spending time in nature. The key is to find activities that are enjoyable and stimulating, allowing them to maintain a sense of accomplishment and participation.
Practical Strategies for Maintaining Independence
| Stage of Alzheimer’s | Cognitive Abilities | Strategies for Maintaining Independence | Examples |
|---|---|---|---|
| Early Stage | Mild cognitive impairment, some memory loss. Generally independent in most daily tasks. | Maintain familiar routines, provide clear and concise instructions, use visual cues, offer choices where appropriate. | Use calendars with large print, label drawers and cupboards, create a visual schedule for daily activities. |
| Middle Stage | Significant memory loss, difficulty with complex tasks. Requires assistance with some daily tasks. | Simplify tasks, provide structure, maintain routines, encourage participation in familiar activities, use sensory stimulation. | Prepare simple meals, use adaptive utensils, create a safe and familiar environment, encourage participation in music therapy. |
| Late Stage | Severe cognitive impairment, loss of most cognitive abilities. Requires significant assistance with daily tasks. | Provide physical and emotional support, maintain a calm and predictable environment, engage in sensory stimulation, ensure comfort and hygiene. | Provide gentle touch, engage in calming activities, ensure proper nutrition and hydration, use touch and sound to communicate. |
Addressing Behavioral Changes: 6 Things People Living With Alzheimers Want You To Know
Navigating the emotional landscape of Alzheimer’s can be challenging, and behavioral changes are a frequent occurrence. These changes aren’t simply “bad behavior,” but often stem from the disease’s impact on the brain. Understanding the root causes is crucial to providing compassionate and effective care.Behavioral changes in individuals living with Alzheimer’s can manifest in various ways, from subtle shifts in mood to more pronounced and disruptive behaviors.
These changes are a complex interplay of cognitive decline, sensory perceptions, and the individual’s struggle to adapt to their changing reality. These shifts can also be triggered by environmental factors, physical discomfort, or unmet needs.
Possible Causes of Behavioral Changes
Alzheimer’s disease affects different parts of the brain at varying stages, disrupting communication pathways and impacting various cognitive functions. This can lead to a wide range of emotional and behavioral changes. Confusion, disorientation, and difficulty communicating can trigger frustration, anxiety, and agitation. Sensory overload, such as noisy environments or bright lights, can cause distress and result in challenging behaviors.
Physical discomfort, pain, or unmet needs, such as hunger, thirst, or a need for the bathroom, can also manifest as behavioral changes.
Managing Challenging Behaviors
Effective management of challenging behaviors necessitates a calm and empathetic approach. Focus on creating a supportive and predictable environment. Simple routines and visual cues can reduce confusion and anxiety. Speak clearly and calmly, using short, simple sentences. Maintain eye contact and use reassuring touch.
Avoid arguing or confronting the individual, as this often exacerbates the situation.
Strategies for Proactive Safety, 6 things people living with alzheimers want you to know
Safety concerns are paramount when addressing behavioral changes. Potential wandering, aggression, or impulsive actions need proactive attention. Install safety measures like locks on doors and windows, and consider a secure environment if wandering is a concern. Regular monitoring and supervision can help prevent accidents. In situations of potential harm, ensuring that the environment is safe and secure is crucial.
Understanding the Root Causes
Identifying the underlying reasons behind behavioral changes is crucial. Is the behavior a reaction to discomfort, confusion, or a need? Thorough communication with the individual’s healthcare team is essential. They can offer insights into potential triggers and recommend strategies to address the underlying causes. Recognizing and addressing these root causes can significantly reduce challenging behaviors and improve the overall well-being of the individual.
Examples of Addressing Safety Concerns
If an individual with Alzheimer’s is prone to wandering, installing motion-activated lights or alarms around the house can alert caregivers to their movements. Securing the home with alarms on doors and windows and implementing a system to track their whereabouts can prevent them from wandering off.
Seeking Support and Resources
Navigating the complexities of Alzheimer’s requires a robust support system. This isn’t just about the person living with the disease; it’s about the entire family. Finding the right resources and support networks can significantly ease the burden and improve the quality of life for everyone involved. Understanding the available assistance is key to managing the challenges effectively.The journey with Alzheimer’s is often challenging, but support is available to make it less arduous.
Recognizing the need for assistance and actively seeking it can empower individuals and families to cope with the various stages and symptoms. It’s important to remember that seeking support isn’t a sign of weakness, but a testament to resilience and a commitment to navigating this journey together.
Importance of Support for Individuals and Caregivers
Support systems are crucial for both the individual living with Alzheimer’s and their caregivers. The individual needs emotional support, understanding, and practical assistance, while caregivers need respite, education, and emotional support to cope with the demands of caregiving. This collaborative support fosters a healthier and more sustainable environment for everyone involved.
I’ve been reading up on the 6 things people living with Alzheimer’s want you to know, and it got me thinking about similar struggles in other health journeys. For example, navigating the complexities of metastatic breast cancer is incredibly tough, and finding supportive resources like metastatic breast cancer blogs can be invaluable. Ultimately, understanding and empathy are key, regardless of the specific health challenge, and those 6 things for people with Alzheimer’s remain important reminders to be compassionate and informed.
Available Resources
A multitude of resources are available to provide assistance and support. These resources range from local support groups and community services to professional counseling and educational programs. Seeking out these resources can significantly enhance the well-being of individuals and families.
- Local Support Groups: These groups provide a safe and supportive environment for individuals with Alzheimer’s and their caregivers to connect with others facing similar experiences. Sharing stories, exchanging advice, and learning from each other’s journeys fosters a sense of community and shared understanding.
- Community Services: Many communities offer valuable services like in-home care, respite care, and meal delivery programs. These services can provide much-needed assistance and support, allowing caregivers to take breaks and maintain their well-being.
- Professional Counseling: Counseling can provide valuable support for both the individual with Alzheimer’s and their caregivers. It offers a safe space for emotional processing, coping strategies, and guidance in navigating the challenges of the disease.
- Educational Programs: Educational programs can provide valuable information about Alzheimer’s disease, its progression, and available resources. These programs empower individuals and caregivers with knowledge and tools to manage the challenges effectively.
Self-Care for Caregivers
Caregivers often experience significant stress and emotional strain due to the demands of caregiving. Prioritizing self-care is essential for caregivers to maintain their well-being and effectively support the individual with Alzheimer’s. Caregivers need to make time for their own physical and mental health, including adequate rest, healthy meals, and engaging in activities they enjoy. This self-care allows caregivers to better handle the demands of caregiving, preventing burnout and promoting long-term well-being.
Support Group Resources
Finding the right support group can make a world of difference. Consider these resources to locate appropriate groups:
| Support Group Name | Location | Specialization | Contact Information |
|---|---|---|---|
| Alzheimer’s Association Support Group | Local Community Center | General support for Alzheimer’s disease | (123) 456-7890 |
| Caregiver Support Group (for dementia) | Senior Center | Specific support for caregivers of individuals with dementia | (987) 654-3210 |
| Memory Care Unit Support Group | Local Hospital | Support for families involved with memory care units | (555) 123-4567 |
| Specific Support Group for Stage 3 Alzheimer’s | Local Church Hall | Tailored support for individuals in stage 3 Alzheimer’s | (111) 222-3333 |
Enhancing Quality of Life
Focusing on quality of life for individuals living with Alzheimer’s is paramount. It’s not just about managing the disease; it’s about fostering a fulfilling and meaningful existence despite the challenges. This involves creating an environment that promotes comfort, engagement, and a sense of purpose. We can achieve this by understanding the individual’s preferences, abilities, and needs at each stage of the disease.This approach is crucial for maintaining a positive emotional state and preventing the isolation and discouragement that can accompany the progression of Alzheimer’s.
It involves respecting the individual’s dignity and promoting a sense of normalcy and belonging.
Importance of Maintaining Routine and Structure
Maintaining a consistent daily routine is vital for individuals with Alzheimer’s. A predictable schedule provides a sense of security and helps them feel more in control. This can involve familiar meal times, activities, and sleep patterns. Adapting routines to the individual’s abilities and limitations is key. For example, breaking down tasks into smaller, manageable steps can help with daily activities.
This can also prevent confusion and anxiety.
Tailoring Activities to Individual Needs
Activities should be tailored to the individual’s abilities and interests, regardless of the stage of Alzheimer’s. The goal is to stimulate engagement, promote joy, and foster a sense of accomplishment. It’s important to recognize that abilities may fluctuate throughout the day or even throughout the week.
Creating a Supportive and Engaging Environment
Creating a supportive and engaging environment involves several key factors. Visual cues, such as calendars and photos, can help with orientation and memory recall. A calming atmosphere, free from clutter and distractions, can be particularly helpful. Engaging the senses through music, aromas, or nature-inspired elements can create a comforting and stimulating experience.
Adapting Activities for Different Stages of Alzheimer’s
| Activity | Benefits | Adaptation for Early Stage | Adaptation for Middle Stage | Adaptation for Late Stage |
|---|---|---|---|---|
| Gentle Exercise | Improved physical health, cognitive function, and mood | Walking, chair exercises, stretching | Chair exercises, gentle stretching, seated yoga | Passive movement, gentle massage, sensory stimulation |
| Music Therapy | Stimulates memory, emotional expression, and social interaction | Listening to favorite music, singing along | Playing familiar instruments, singing along to familiar songs | Listening to soothing music, gentle touch to rhythm |
| Art Therapy | Provides a creative outlet, promotes emotional expression, and enhances well-being | Drawing, painting, sculpting | Creating collages, coloring books, simple crafts | Tactile stimulation with clay, textured objects, simple painting |
| Sensory Stimulation | Enhances awareness, promotes engagement, and reduces anxiety | Gentle touch, soft music, aromatherapy | Soft lighting, aromatherapy, nature sounds | Gentle touch, soothing music, soft lighting |
| Storytelling and Reminiscence | Stimulates memory, fosters emotional connection, and provides a sense of identity | Sharing personal stories, looking at old photos | Sharing family stories, reminiscing about past events | Using sensory objects to trigger memories, gentle reminders of familiar moments |
Closure
Ultimately, embracing empathy and understanding is key when supporting someone with Alzheimer’s. By acknowledging the specific challenges at each stage, communicating with clarity and respect, and providing the necessary support, we can make a tangible difference in the lives of those affected. This journey is about connection, compassion, and creating a supportive environment. Remember, you’re not alone.