Conditions women hard diagnose present a significant challenge in healthcare. This deep dive explores the multifaceted reasons behind these diagnostic difficulties, ranging from historical biases to biological variations and societal influences. We’ll examine how these factors impact the accuracy and timeliness of diagnoses for women, highlighting the crucial need for a more nuanced and patient-centered approach.
From the subtle differences in symptom presentation to the pervasive impact of implicit bias, this exploration delves into the complexities of diagnosing women. We’ll analyze common conditions where these difficulties are most pronounced, providing concrete examples to illustrate the challenges and opportunities for improvement.
Difficulties in Diagnosis for Women
The journey to accurate medical diagnoses can be significantly more challenging for women than for men, often due to systemic biases and a lack of understanding of unique physiological factors. This disparity in care stems from a complex interplay of historical, societal, and biological elements, leading to delayed or misdiagnosed conditions. This article explores the multifaceted nature of these challenges, examining specific examples to illustrate the potential for harm.The historical and societal factors that have contributed to diagnostic disparities for women are numerous and intertwined.
For instance, the medical field, in many instances, was historically developed and researched primarily using male bodies as the standard, leading to the exclusion or underrepresentation of women’s health concerns in research studies. This has resulted in diagnostic criteria often not tailored to women’s specific physiology, potentially causing misinterpretations of symptoms and delays in receiving appropriate care. Societal expectations and gender roles also play a significant part, as women may be less likely to voice concerns or be taken seriously by healthcare providers, thus contributing to a cycle of misdiagnosis.
Historical and Societal Factors Contributing to Diagnostic Challenges
Societal norms often dictate that women suppress pain and discomfort, potentially leading to delayed presentation of symptoms. This can also manifest in healthcare providers downplaying or dismissing women’s complaints compared to those of men, creating a significant barrier to accurate diagnosis. The lack of adequate research on women’s health has also contributed to a knowledge gap in understanding how conditions manifest differently in females, which in turn can affect the development of appropriate diagnostic tools and procedures.
Potential Biases in Diagnostic Criteria and Procedures
Diagnostic criteria and procedures themselves can contain inherent biases, often without explicit acknowledgement. For instance, established norms may not reflect the diverse range of physiological variations among women, or how specific conditions may present differently in women compared to men. This can lead to misinterpretations of symptoms and potentially inaccurate diagnoses. Furthermore, gender bias in research often leads to limited data on female physiology, hindering the development of more accurate diagnostic criteria.
Comparison of Diagnostic Processes for Heart Disease
| Characteristic | Men | Women |
|---|---|---|
| Typical Symptoms | Chest pain, shortness of breath, discomfort in the arms or jaw | Often atypical symptoms, such as shortness of breath, fatigue, nausea, back pain, or upper abdominal discomfort. Sometimes dismissed as non-cardiac. |
| Diagnostic Tests | Standard ECG, cardiac enzymes, angiography | Potentially delayed or inappropriate use of diagnostic tests, leading to delayed diagnosis. May be less likely to receive aggressive interventions compared to men with similar symptoms. |
| Treatment Approaches | Aggressive interventions such as angioplasty or stenting | Potentially less aggressive treatment approaches, potentially due to underestimation of severity of symptoms or lack of awareness of female-specific risks. |
This table highlights potential differences in the diagnostic process for heart disease in men and women. These differences can lead to significant disparities in care and outcomes, as early diagnosis and treatment are crucial for positive outcomes.
Typical Symptoms Reported by Women and Men for Various Conditions
| Condition | Typical Symptoms Reported by Women | Typical Symptoms Reported by Men |
|---|---|---|
| Depression | Fatigue, feelings of hopelessness, loss of interest in activities, changes in sleep patterns, and increased crying spells. May report physical symptoms like headaches or stomach problems. | Irritability, anger, loss of interest, difficulty concentrating, changes in sleep patterns, and feelings of worthlessness. More likely to report physical symptoms like muscle pain or headaches. |
| Anxiety | Muscle tension, rapid heartbeat, shortness of breath, sweating, and difficulty concentrating. Often report digestive issues or unexplained pain. | Irritability, restlessness, difficulty concentrating, muscle tension, and sleep problems. More likely to report physical symptoms like headaches or stomach problems. |
| (Other conditions) | (Detailed examples of other conditions and symptom differences could be added here) | (Detailed examples of other conditions and symptom differences could be added here) |
Significant differences in reported symptoms between genders can lead to misdiagnosis, especially if healthcare providers are not aware of these potential variations. It is important for both patients and healthcare professionals to recognize these potential differences to improve the accuracy and speed of diagnosis.
Underlying Biological Factors
The intricate dance of hormones and anatomy plays a crucial role in shaping the experience of illness in women. Understanding these biological factors is essential for improving diagnostic accuracy and patient care. Hormonal fluctuations, anatomical variations, and diverse physiological responses all contribute to a complex picture, often obscuring the presentation of symptoms.This complexity necessitates a nuanced approach to diagnosis, recognizing that a symptom experienced by a woman may have a different underlying cause compared to a man.
Recognizing the influence of these biological factors allows healthcare providers to approach each patient with a more holistic perspective, ultimately leading to more accurate and effective treatment.
Hormonal Fluctuations and Symptom Presentation
Hormonal fluctuations throughout a woman’s life, particularly during menstruation, pregnancy, and menopause, can significantly impact symptom presentation. These fluctuations can alter the sensitivity and expression of various physiological systems, leading to variations in pain perception, fatigue levels, and other symptoms. For instance, hormonal changes can affect the severity and frequency of migraines, making it difficult to pinpoint the root cause.
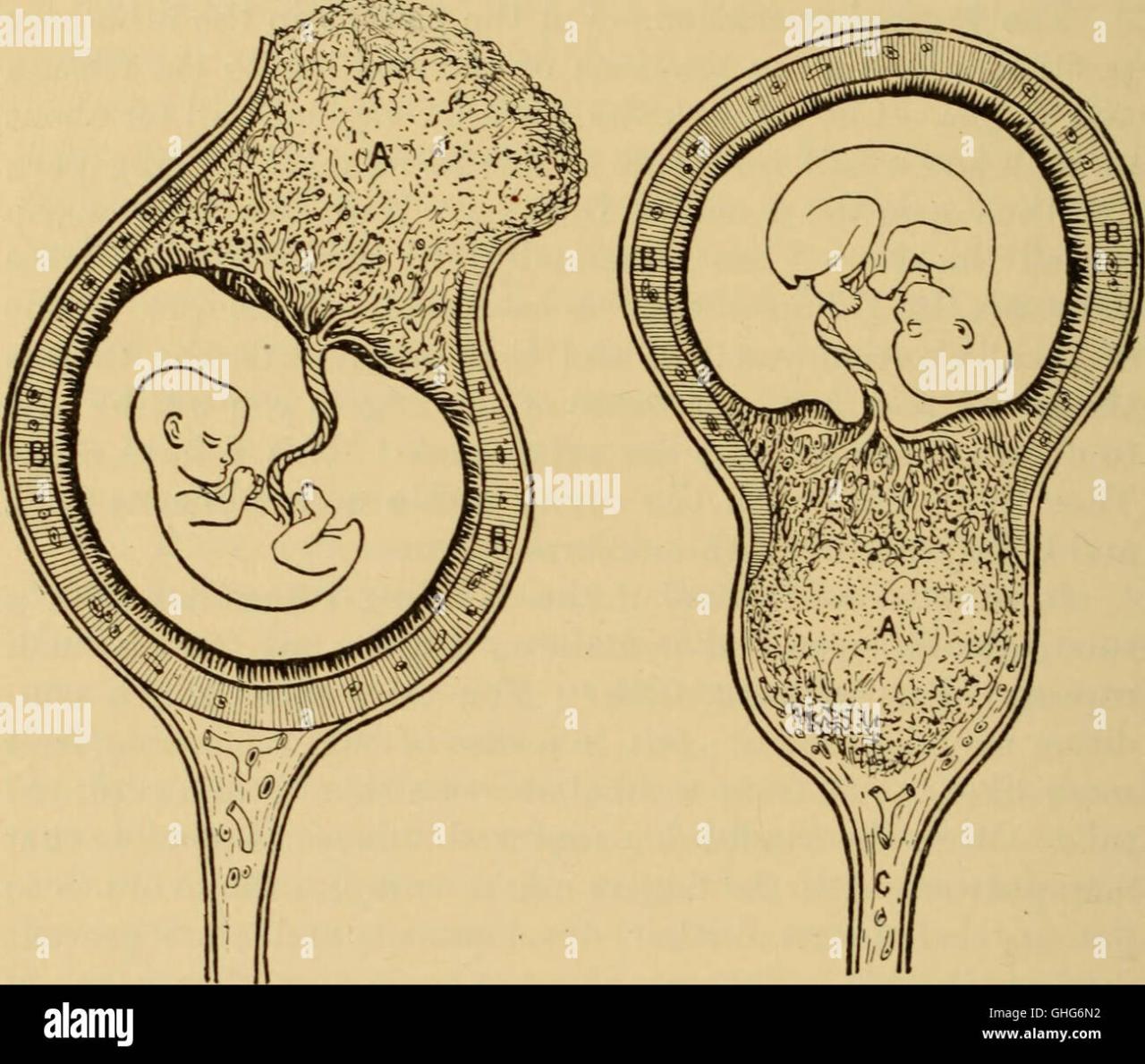
Anatomical Differences and Diagnostic Approaches
Anatomical differences between men and women can influence the presentation and interpretation of symptoms. For example, differences in the structure of the pelvis and reproductive organs can affect the location and intensity of pain. These variations can also impact the effectiveness of certain diagnostic procedures.
Specific Conditions Complicated by Biological Factors
Several conditions are particularly challenging to diagnose in women due to the interplay of biological factors.
- Endometriosis: Characterized by the presence of endometrial tissue outside the uterus, endometriosis can manifest with a wide range of symptoms, including pelvic pain, heavy bleeding, and infertility. The cyclical nature of hormonal fluctuations can exacerbate these symptoms, making it difficult to distinguish them from other conditions, such as ovarian cysts or pelvic inflammatory disease. Moreover, the location of endometrial implants can vary, influencing the type and intensity of pain experienced.
- Fibromyalgia: This chronic condition involves widespread musculoskeletal pain, fatigue, and sleep disturbances. The influence of hormonal fluctuations and the impact of stress on pain perception can make diagnosis challenging. Furthermore, the variability in symptom presentation from one woman to another, compounded by the absence of definitive diagnostic tests, contributes to diagnostic complexity.
Variations in Physiological Responses and Symptom Interpretation
Women may experience different physiological responses to illness compared to men. This variation can impact symptom interpretation. For example, the experience of pain can differ based on hormonal levels and other factors. Consequently, a symptom that might be easily recognized in a man could be masked or misinterpreted in a woman.
Impact of Reproductive Stages on Symptom Presentation
| Reproductive Stage | Common Condition | Symptom Presentation Variations |
|---|---|---|
| Menstruation | Migraines | Increased frequency and intensity during menstruation; overlap with premenstrual syndrome symptoms. |
| Pregnancy | Back pain | Increased load on the spine, hormonal changes affecting ligament laxity; symptoms can mimic other conditions. |
| Menopause | Joint pain | Hormonal changes affecting bone density and joint structure; symptoms can be confused with osteoarthritis. |
| Reproductive years | Chronic fatigue syndrome | Symptom presentation influenced by hormonal cycles; fatigue severity varies depending on the phase of the menstrual cycle. |
Social and Environmental Influences
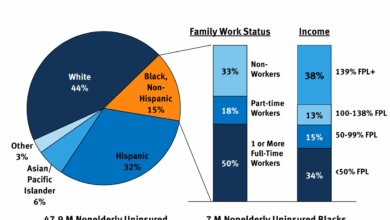
The journey to accurate diagnosis for women often encounters obstacles beyond the biological realm. Social and environmental factors significantly impact women’s access to healthcare, their willingness to report symptoms, and how those symptoms are interpreted by healthcare providers. Understanding these influences is crucial to improving diagnostic equity and ensuring women receive timely and appropriate care.Socioeconomic status and cultural norms play a vital role in shaping women’s healthcare experiences.
Limited access to resources, including transportation, childcare, and financial stability, can create barriers to preventative screenings, follow-up appointments, and adherence to treatment plans. These systemic inequities can lead to delayed or missed diagnoses, particularly for women from marginalized communities.
Socioeconomic Status and Healthcare Access
Different socioeconomic levels often result in varying levels of access to quality healthcare. Financial constraints can hinder women’s ability to afford necessary tests, specialists, or even routine check-ups. This disparity in access can lead to delayed diagnoses and poorer health outcomes.
Cultural Norms and Symptom Reporting
Cultural norms and expectations surrounding women’s health can influence symptom reporting and physician interpretation. In some cultures, certain symptoms are perceived as normal or are attributed to other factors, leading women to delay or avoid seeking medical attention. Furthermore, gender roles and societal expectations can impact women’s comfort level in discussing their symptoms with healthcare providers, potentially hindering the diagnostic process.
Implicit Bias in the Diagnostic Process, Conditions women hard diagnose
Implicit biases, often unconscious, can influence healthcare providers’ judgments and interpretations of women’s symptoms. These biases can result in differing diagnostic approaches or levels of attention given to women compared to men presenting with similar symptoms. This can lead to misdiagnosis or delayed diagnoses, particularly when the symptoms are less overtly “typical.”
Cultural Differences and Symptom Expression
Cultural backgrounds significantly impact how women experience and express symptoms. For example, some cultures may associate certain physical sensations with spiritual or emotional factors, leading women to seek help from traditional healers before consulting a physician. This can complicate the diagnostic process if cultural differences aren’t considered. Understanding these nuances is crucial for healthcare providers to provide culturally sensitive care and accurate diagnoses.
A patient’s understanding of their illness can differ from a healthcare professional’s, leading to miscommunication.
Table: Healthcare Access and Diagnostic Rates
| Socioeconomic Background | Healthcare Access (e.g., Regular Check-ups) | Diagnostic Rate (e.g., for common women’s health conditions) | Potential Factors |
|---|---|---|---|
| High Socioeconomic Status | High | High | Affordability, access to specialists, and awareness of preventative care |
| Low Socioeconomic Status | Low | Low | Limited financial resources, lack of transportation, and lower health literacy |
| Rural Communities | Low | Low | Geographical limitations, limited access to specialists, and lack of transportation |
Specific Condition Examples
Understanding the unique challenges women face in diagnosis requires a deep dive into specific conditions. Diagnostic hurdles often stem from variations in symptom presentation, masking of symptoms by other conditions, and a lack of awareness about gender-specific manifestations. This section will explore the diagnostic complexities surrounding autoimmune disorders, mental health issues, and gynecological problems, highlighting how existing criteria may not always reflect the diverse experiences of women.Existing diagnostic criteria for many conditions often fail to account for the complex interplay of biological, social, and environmental factors that influence a woman’s health.
This can lead to delayed diagnoses, inadequate treatment, and a diminished quality of life. A patient-centered approach, acknowledging the individuality of each woman’s experience, is crucial for more accurate and timely diagnoses.
Autoimmune Disorders
Autoimmune disorders, like lupus and rheumatoid arthritis, often present with a range of symptoms that can vary significantly between individuals. Women frequently experience symptoms that are less pronounced or different than those in men, leading to misdiagnosis or delayed diagnosis. For instance, fatigue, joint pain, and skin rashes are common, but the specific presentation and severity can differ considerably.
So many conditions are tough for women to get diagnosed, right? It’s frustrating when symptoms are dismissed or mislabeled. Luckily, there are innovative tools like a migraine app, which can help people better track and understand their symptoms, migraine app helps people with migraines. This could potentially help with diagnosis and treatment by providing valuable data.
But, even with these tools, there’s still a long way to go in accurately diagnosing conditions that disproportionately affect women.
The overlap of symptoms with other conditions, like depression or fibromyalgia, further complicates the diagnostic process.
It’s frustrating how many conditions women struggle to get diagnosed. Sometimes, a simple test can seem like the answer, but a concerning number of at-home genetic tests are producing false positives, like 40 percent of them, according to this recent study 40 percent at home genetic test results false positives. This highlights the complexity of accurate diagnosis and the need for thorough professional evaluation.
Ultimately, relying solely on these tests can lead to unnecessary worry and delay in getting the right care.
Mental Health Issues
Mental health issues, such as depression and anxiety, are often under-recognized and under-treated in women. Cultural expectations and societal pressures can influence how women express and experience these conditions. For example, women may internalize symptoms and attribute them to stress, while men may be more prone to outwardly displaying their distress. Additionally, the criteria used to diagnose these conditions may not adequately capture the range of experiences, particularly the unique impact of gender roles and societal expectations.
The perception of emotional vulnerability can also contribute to under-reporting.
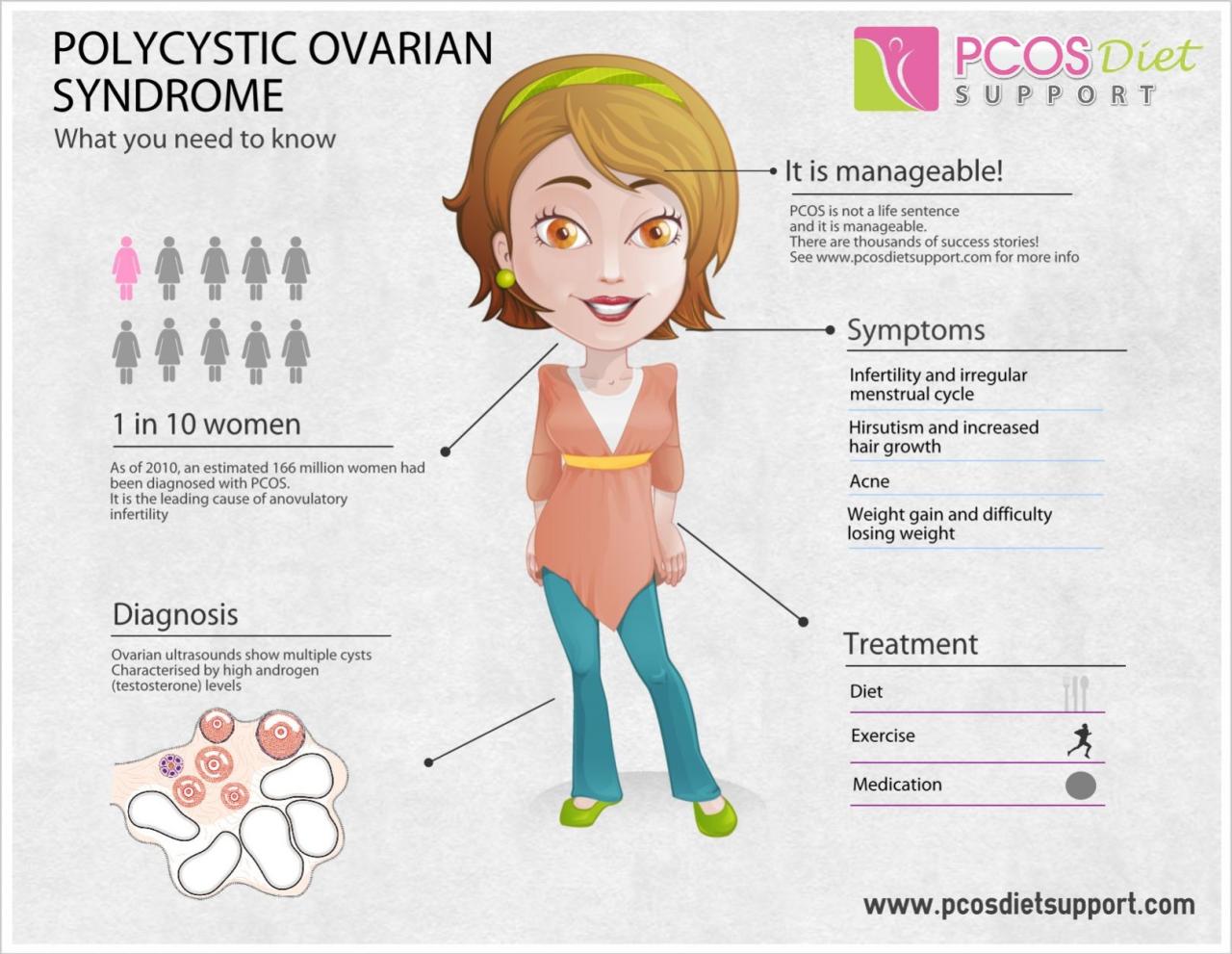
Gynecological Problems
Gynecological issues, such as endometriosis and polycystic ovary syndrome (PCOS), often present with non-specific symptoms. Pain, irregular periods, and fertility problems are common, but the intensity and presentation of these symptoms can vary greatly between women. The subjective nature of some symptoms, such as pelvic pain, further complicates diagnosis. The potential for overlap with other conditions, like irritable bowel syndrome or anxiety, adds to the diagnostic challenge.
Furthermore, societal stigma surrounding women’s health can contribute to reluctance to seek medical attention.
| Condition | Common Symptoms | Diagnostic Criteria |
|---|---|---|
| Lupus | Fatigue, joint pain, skin rashes, fever, headaches | Presence of specific autoantibodies, clinical evaluation, and exclusion of other conditions |
| Depression | Persistent sadness, loss of interest, changes in appetite or sleep, feelings of worthlessness | DSM-5 criteria for major depressive disorder, clinical evaluation, and exclusion of other conditions |
| Endometriosis | Pelvic pain, heavy or irregular periods, pain during sex, infertility | Diagnostic laparoscopy, evaluation of symptoms, and exclusion of other conditions |
| PCOS | Irregular periods, ovarian cysts, acne, excessive hair growth, infertility | Clinical evaluation, hormonal testing, and exclusion of other conditions |
Improving Diagnostic Accuracy
Improving diagnostic accuracy for women requires a multifaceted approach that addresses the unique challenges women face in healthcare. Existing biases and a lack of awareness of sex-specific differences in disease presentation often lead to delayed or misdiagnosis. This necessitates a shift towards more patient-centered care, incorporating diverse perspectives and utilizing evidence-based diagnostic tools tailored to the female body.
Strategies for Enhanced Diagnostic Accuracy
Diagnostic accuracy hinges on a combination of improved training, recognition of bias, and patient-centric approaches. By recognizing and addressing gender-based biases in diagnostic criteria and interpretation, healthcare providers can significantly reduce misdiagnosis rates. Furthermore, a more comprehensive understanding of the interplay between biological factors and social determinants of health can lead to more effective diagnostic processes.
Recognizing and Mitigating Biases in Diagnostic Processes
Gender bias in healthcare is a persistent issue. This bias can manifest in various ways, from underreporting of women’s symptoms to differing interpretations of symptoms based on gender stereotypes. For instance, pain experienced by women may be attributed to psychosomatic factors more readily than physical causes. Acknowledging these biases and actively working to mitigate them is crucial for accurate diagnoses.
Certain health conditions can be tough for women to pinpoint, often masking themselves in less obvious symptoms. This can be especially true when considering dietary changes. For example, a declining quality of diet in older adults can often manifest in subtle ways, making it harder to diagnose. Fortunately, there are actionable steps to address this, as outlined in this helpful guide on quality of diet for older adults has declined heres how to fix it.
Ultimately, understanding the factors contributing to these conditions, including diet, is crucial for effective diagnosis and treatment in women.
This involves creating awareness and implementing training programs for healthcare providers to recognize and address these implicit biases. Furthermore, using standardized diagnostic criteria that consider sex-specific factors and encouraging open communication between patients and providers can help.
Implementing Patient-Centered Care to Enhance Symptom Reporting and Interpretation
Patient-centered care emphasizes understanding and respecting individual experiences and preferences. Encouraging open and honest communication between patients and healthcare providers is essential. This includes creating a safe and supportive environment for women to discuss their symptoms without fear of judgment or dismissal. Active listening and validating the patient’s perspective are critical components. Providers should also actively solicit information about the patient’s social and environmental factors, recognizing that these can influence symptom presentation and overall health.
The Role of Diverse Healthcare Providers in Improving Outcomes
A diverse healthcare workforce is crucial for improving diagnostic accuracy. This diversity brings a range of perspectives and experiences, allowing for a more nuanced understanding of the complex interplay of biological, social, and environmental factors affecting women’s health. Healthcare teams that include women, people of color, and individuals from diverse backgrounds can better address the specific needs and experiences of diverse patient populations.
This broader perspective helps to identify and avoid potential biases.
Comparison of Diagnostic Methods for Women and Men
| Condition | Diagnostic Method (Women) | Diagnostic Method (Men) | Efficacy Comparison |
|---|---|---|---|
| Breast Cancer | Mammography, ultrasound, MRI | Mammography, ultrasound, MRI | Mammography is a widely used and effective screening tool for both, but specific protocols might be adjusted to accommodate the breast density of women. |
| Heart Disease | Electrocardiogram (ECG), cardiac stress test, cardiac CT scan | Electrocardiogram (ECG), cardiac stress test, cardiac CT scan | While the diagnostic methods are similar, women often present with atypical symptoms, making early detection challenging. |
| Depression | Patient interview, symptom questionnaires, blood tests | Patient interview, symptom questionnaires, blood tests | Symptoms may present differently, and societal expectations can influence reporting. Recognizing this is key to accurate diagnosis. |
This table highlights the need for adaptable and personalized approaches to diagnosis, acknowledging the potential variations in presentation across genders.
Case Studies and Illustrations: Conditions Women Hard Diagnose
Navigating the labyrinth of medical diagnosis, especially for women, can be a frustrating and often disheartening journey. The challenges are multifaceted, encompassing biological predispositions, societal biases, and the inherent complexity of the human body. This section delves into real-world scenarios, highlighting the difficulties in accurately diagnosing women with various conditions.Understanding the diagnostic odyssey of a woman experiencing symptoms can shed light on the systemic issues that contribute to delayed or misdiagnosis.
By examining case studies, we can better grasp the interplay of biological, social, and environmental factors that impact the diagnostic process.
Hypothetical Case Study: A Woman with Persistent Fatigue
A 35-year-old woman, Sarah, presents with persistent fatigue, headaches, and muscle aches for the past six months. She reports feeling significantly less productive at work and struggles with daily tasks. Her primary care physician attributes her symptoms to stress and recommends lifestyle changes. Sarah, however, feels this is insufficient. She seeks a second opinion.
This illustrates the common pattern of initial dismissals of women’s health concerns.
Cultural and Social Influences on Diagnosis
Cultural and social factors significantly influence how symptoms are perceived and interpreted, impacting the diagnostic process. For example, a woman from a culture where mental health issues are stigmatized might be hesitant to seek help, leading to a delayed diagnosis. Or, a woman experiencing physical symptoms might be discouraged from seeking medical attention if her symptoms are dismissed as “normal” for her gender.
Challenges in Establishing a Proper Diagnosis
Establishing a precise diagnosis can be particularly challenging for women due to several factors. Overlap in symptoms between various conditions can mask the underlying cause, requiring meticulous investigation. Furthermore, the physiological differences between men and women can lead to different responses to similar conditions. Consider the different hormonal fluctuations that women experience throughout their lives.
Fictitious Patient Scenario: A Complex Case
Consider Amelia, a 42-year-old woman experiencing a constellation of symptoms including chest pain, shortness of breath, and palpitations. Her primary care physician initially attributes her symptoms to anxiety. Amelia, however, feels this explanation doesn’t adequately address the severity of her discomfort. She seeks a second opinion, undergoing various tests, including cardiac evaluations and blood work. The tests yield inconsistent results, making it difficult to pinpoint the precise cause.
This highlights the complexity of establishing a proper diagnosis when dealing with a complex case involving multiple potential contributing factors. This also illustrates how the interplay of factors like anxiety and underlying medical conditions can confound the diagnostic process, often leading to misdiagnosis. Amelia’s situation underscores the need for a thorough and comprehensive approach to diagnosis, especially when dealing with women’s health concerns.
Ultimate Conclusion
In conclusion, diagnosing conditions in women requires a multifaceted understanding that goes beyond the traditional diagnostic framework. By acknowledging the historical, biological, and social factors that contribute to diagnostic disparities, we can begin to develop more effective strategies for improving accuracy and empathy in healthcare. Ultimately, a patient-centered approach, combined with awareness of these complexities, will lead to more accurate and timely diagnoses for women, ensuring they receive the appropriate care they deserve.