Primary and secondary emphysema, two forms of a debilitating lung disease, are often confused. This exploration delves into the intricacies of each, from their underlying causes to their distinct symptoms and treatments. Understanding the differences between these two types is crucial for effective diagnosis and management. We’ll dissect the pathological features, explore the genetic and environmental triggers, and examine how these factors influence disease progression.
Get ready to unravel the complexities of these lung conditions.
Primary emphysema, often stemming from genetic mutations, can manifest earlier in life, while secondary emphysema is frequently linked to environmental factors like smoking. This difference is reflected in the various symptoms and treatment approaches. This in-depth look will guide you through the complexities of both types, providing a clearer understanding of the nuances of each form.
Introduction to Emphysema
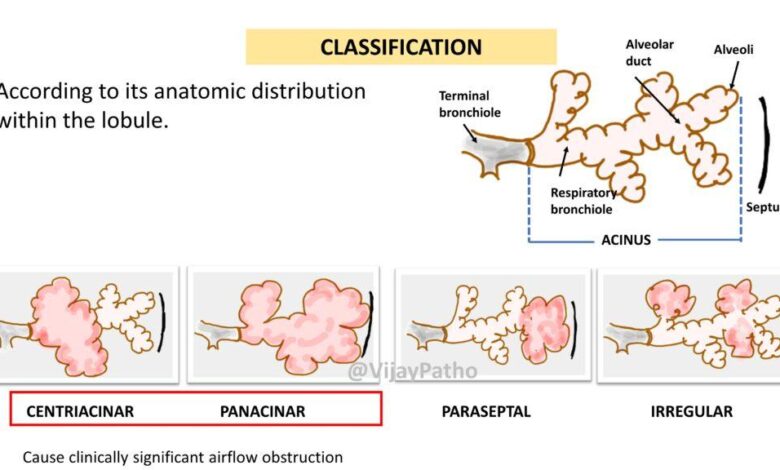
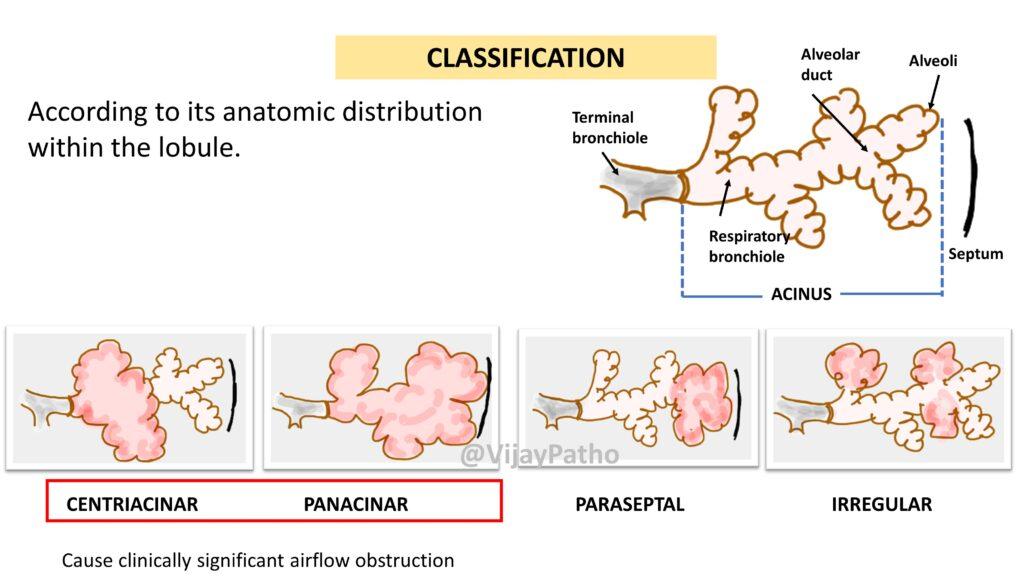
Emphysema is a chronic lung disease characterized by the destruction of the alveoli, the tiny air sacs in the lungs responsible for gas exchange. This destruction leads to a progressive loss of lung function, making it increasingly difficult to breathe. Crucially, emphysema isn’t a single entity; it’s categorized into primary and secondary forms, each with distinct causes and characteristics.
Primary emphysema stems from genetic predispositions, while secondary emphysema arises from environmental factors, most notably smoking. Understanding these distinctions is vital for diagnosis and treatment.The pathological hallmark of emphysema is the enlargement and destruction of the alveoli, accompanied by the loss of their elastic recoil. This loss of elasticity impairs the lungs’ ability to expel air effectively, leading to air trapping and overinflation of the lungs.
Primary and secondary emphysema differ in the underlying mechanisms driving this alveolar damage, influencing the disease progression and associated symptoms. For example, primary emphysema often manifests at a younger age compared to secondary emphysema, which tends to be associated with long-term exposure to environmental irritants.
Key Pathological Features of Emphysema
The key pathological features that differentiate primary and secondary emphysema primarily lie in the root causes. Primary emphysema, arising from genetic defects, often shows a diffuse pattern of alveolar damage. This contrasts with secondary emphysema, which frequently displays a more focal pattern of damage concentrated in specific areas of the lung. The severity and progression of these pathological changes can vary significantly between individuals, influencing the overall clinical presentation.
Underlying Causes of Emphysema
Understanding the causes of emphysema is essential for prevention and treatment. Both primary and secondary emphysema have diverse causes, ranging from genetic predispositions to environmental triggers.
- Primary Emphysema: This form of emphysema is predominantly linked to genetic mutations, often affecting genes responsible for elastin and collagen production. Examples of such genetic conditions include α1-antitrypsin deficiency, which impairs the body’s ability to protect the lungs from damaging enzymes. This genetic predisposition makes individuals more susceptible to the development of emphysema, often presenting at a younger age than secondary emphysema.
- Secondary Emphysema: This form is largely driven by environmental factors. Prolonged exposure to air pollutants, particularly cigarette smoke, is the most significant environmental risk factor. Other factors include exposure to occupational dusts and fumes, and recurrent respiratory infections. These environmental irritants trigger an inflammatory response in the lungs, ultimately leading to alveolar damage and emphysema.
Common Symptoms of Emphysema
The symptoms of emphysema, irrespective of the type, typically emerge gradually, progressively worsening over time.
- Shortness of breath, especially during physical activity
- Chronic cough, often productive of sputum
- Wheezing, a whistling sound during breathing
- Chest tightness
- Frequent respiratory infections
Comparison of Primary and Secondary Emphysema
The table below highlights the key distinctions between primary and secondary emphysema:
| Feature | Primary Emphysema | Secondary Emphysema |
|---|---|---|
| Cause | Genetic mutations (e.g., α1-antitrypsin deficiency) | Environmental factors (e.g., smoking, air pollution) |
| Symptoms | Similar to secondary, but often onset earlier in life | Often exacerbated by smoking or other environmental factors |
| Treatment | Similar to secondary, but with a focus on managing the genetic component | Similar to secondary, but with a focus on eliminating the environmental trigger |
Pathophysiology of Primary Emphysema
Primary emphysema, a devastating lung disease, arises from inherited genetic defects that disrupt the delicate balance of the lung’s structure and function. These mutations lead to a cascade of events ultimately resulting in the progressive destruction of the alveoli, the tiny air sacs responsible for gas exchange. Understanding the pathophysiology is crucial for developing targeted therapies and improving patient outcomes.
Genetic Mutations in Primary Emphysema
Mutations in specific genes are responsible for primary emphysema. These genetic defects often affect proteins crucial for lung structure and function. Commonly affected genes include α1-antitrypsin (AAT) and other elastin-associated genes. These mutations lead to dysfunctional proteins, which are unable to effectively carry out their intended roles, initiating the destructive cascade.
Mechanisms of Alveolar Damage
The dysfunctional proteins, stemming from genetic mutations, disrupt the normal processes that maintain the integrity of the alveoli. This disruption can manifest in several ways. For example, insufficient α1-antitrypsin leads to an imbalance in the protease-antiprotease system. Proteases, enzymes that break down proteins, are not effectively inhibited, leading to the excessive breakdown of elastin, a crucial component of the alveolar walls.
This excessive breakdown results in the loss of elasticity and the gradual destruction of the alveolar structure.
The Inflammatory Response in Primary Emphysema
The presence of dysfunctional proteins and the breakdown of elastin trigger a robust inflammatory response within the lungs. Inflammation, while a natural defense mechanism, can become detrimental in primary emphysema. In this context, the inflammatory cascade is characterized by the recruitment of immune cells, like neutrophils and macrophages, to the affected areas. These cells release various inflammatory mediators, exacerbating the damage to the lung tissue and contributing to the progressive loss of alveolar function.
Primary and secondary emphysema, both impacting lung function, often stem from underlying conditions. While I’m not a doctor, I’ve been researching ways to improve overall health, and a recent article I came across about whether or not can sparkling water cause weight gain sparked my curiosity about lifestyle choices and their potential influence on respiratory health.
Regardless, understanding these types of emphysema is crucial for proactive health management.
Role of Elastin and its Degradation
Elastin, a crucial protein component of the lung’s connective tissue, provides the elasticity needed for the alveoli to expand and contract during breathing. In primary emphysema, the degradation of elastin, accelerated by the uncontrolled protease activity, leads to the loss of this crucial property. This loss of elasticity, along with the destruction of the alveolar walls, results in the characteristic air trapping and hyperinflation of the lungs observed in the disease.
Flowchart of Primary Emphysema Progression
| Stage | Event |
|---|---|
| 1. Genetic Mutation | Inherited mutations in genes like α1-antitrypsin (AAT) or other elastin-associated genes occur. |
| 2. Dysfunctional Protein Production | The mutations lead to the production of dysfunctional proteins, which fail to perform their normal roles. |
| 3. Protease-Antiprotease Imbalance | The lack of functional α1-antitrypsin, a protease inhibitor, allows proteases to degrade elastin without proper control. |
| 4. Elastin Degradation | Excessive elastin breakdown occurs, weakening the alveolar walls. |
| 5. Alveolar Damage | The alveolar walls lose elasticity and integrity, leading to their destruction. |
| 6. Inflammation and Fibrosis | The inflammatory response and fibrosis further contribute to the loss of lung function. |
| 7. Air Trapping and Hyperinflation | Air becomes trapped in the damaged alveoli, causing the lungs to hyperinflate. |
| 8. Emphysema | Progressive loss of lung function culminates in the clinical diagnosis of emphysema. |
Pathophysiology of Secondary Emphysema
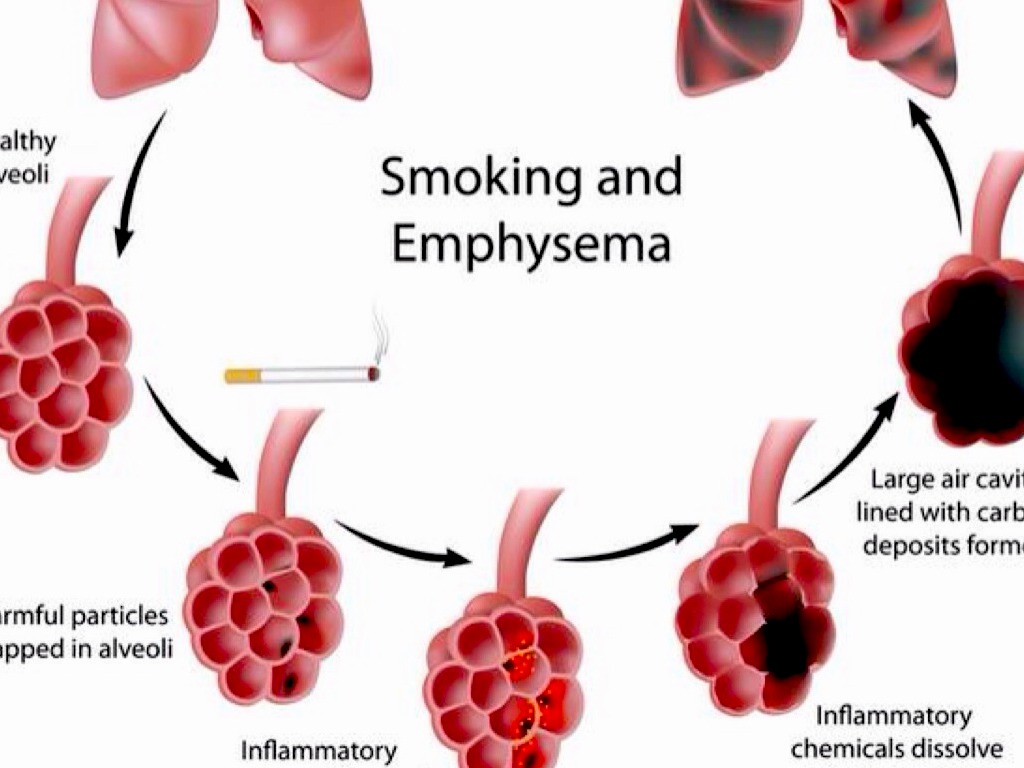
Secondary emphysema, a debilitating lung condition, arises from a complex interplay of environmental factors and the body’s response to them. Unlike primary emphysema, which has a genetic basis, secondary emphysema is almost always linked to long-term exposure to harmful substances and irritants. This chronic exposure triggers a cascade of detrimental events within the lungs, ultimately leading to the characteristic damage and airflow limitation of emphysema.Chronic inflammation, a hallmark of secondary emphysema, is intimately connected to environmental factors like smoking and air pollution.
This persistent inflammatory response weakens the lung’s structural integrity, contributing to the breakdown of alveolar walls. Oxidative stress, a consequence of this inflammation, further exacerbates the damage, creating a vicious cycle that progressively deteriorates lung function.
Chronic Inflammation in Secondary Emphysema
Chronic inflammation plays a central role in the development and progression of secondary emphysema. This persistent inflammatory response, often driven by inhaled irritants, activates various immune cells, such as neutrophils and macrophages. These cells release inflammatory mediators, including cytokines and reactive oxygen species (ROS). This inflammatory cascade leads to the recruitment of more inflammatory cells, creating a self-perpetuating cycle of lung damage.
Smoking is a prime example, as the toxins in cigarette smoke activate inflammatory pathways, resulting in chronic bronchitis and, ultimately, emphysema.
Oxidative Stress and Lung Tissue Damage
Oxidative stress, characterized by an imbalance between reactive oxygen species (ROS) production and antioxidant defenses, is a key contributor to the tissue damage seen in secondary emphysema. ROS, generated by inflammatory cells and environmental pollutants, damage cellular components, including lipids, proteins, and DNA. This damage contributes to the destruction of elastin and collagen fibers, the crucial components of lung tissue structure.
For instance, exposure to air pollutants can increase ROS production, leading to oxidative stress and consequent lung damage.
Primary and secondary emphysema, while distinct in their causes, both lead to the same unfortunate lung damage. But beyond the physical toll, it’s important to consider the wider societal issues that impact health outcomes, like access to mental healthcare is harder for black Americans, here’s why. These systemic barriers can affect individuals’ ability to manage chronic conditions like emphysema, creating a complex interplay between physical and mental well-being.
Ultimately, addressing the root causes of these disparities is crucial to improving the overall health and quality of life for everyone affected by primary and secondary emphysema.
Protease-Antiprotease Imbalance
The balance between proteases and antiproteases is crucial for maintaining lung tissue integrity. In secondary emphysema, this delicate equilibrium is disrupted, leading to an excess of proteases, enzymes that break down proteins, and a deficiency of antiproteases, which counteract these proteolytic actions. This imbalance is often associated with smoking, which leads to increased production of neutrophil elastase, a potent protease that degrades elastin fibers.
Consequently, the destruction of elastin fibers in the alveoli causes the characteristic emphysematous changes.
“The imbalance between proteases and antiproteases is a critical factor in the pathogenesis of emphysema.”
Impact of Inhaled Irritants
Inhaled irritants, such as cigarette smoke, air pollutants, and industrial dusts, are major contributors to the development of secondary emphysema. These irritants trigger an inflammatory response in the lungs, which leads to the release of proteases and ROS. Repeated exposure to these irritants over time progressively damages lung tissue, leading to the characteristic emphysematous changes. For instance, long-term exposure to silica dust in miners can induce a significant inflammatory response and protease-antiprotease imbalance, eventually leading to emphysema.
Environmental Factors Contributing to Secondary Emphysema
| Environmental Factor | Mechanism of Action |
|---|---|
| Smoking | Induces inflammation, increases protease production, and impairs antioxidant defenses. |
| Air pollution | Increases ROS production, damages lung tissue, and exacerbates inflammation. |
| Occupational exposure (e.g., silica dust) | Induces a strong inflammatory response, leading to protease-antiprotease imbalance and lung damage. |
| Alpha-1 antitrypsin deficiency | Reduced levels of antiproteases increase susceptibility to emphysema, especially when combined with environmental factors. |
| Infections (e.g., chronic bronchitis) | Repeated infections contribute to chronic inflammation and lung damage. |
Diagnosis and Treatment: Primary And Secondary Emphysema
Navigating the complexities of emphysema, whether primary or secondary, hinges on accurate diagnosis and effective treatment. This crucial stage involves a multifaceted approach, encompassing various diagnostic methods, tailored treatment plans, and the vital role of pulmonary rehabilitation. Understanding the nuances of each type is essential for optimizing patient outcomes and mitigating potential complications.
Diagnostic Methods Comparison
Accurate diagnosis of emphysema relies on a combination of clinical evaluation, imaging studies, and pulmonary function tests. For both primary and secondary emphysema, a thorough medical history and physical examination are paramount. Symptoms, such as shortness of breath, chronic cough, and wheezing, along with a detailed family history, help clinicians narrow down the possibilities. Spirometry, a common pulmonary function test, assesses airflow limitations and is crucial for confirming the presence of airflow obstruction, a hallmark of emphysema.
Chest X-rays and CT scans are valuable imaging tools to visualize the lungs, providing details about lung structure and the extent of air trapping. While chest X-rays might show hyperinflation in advanced cases, high-resolution CT scans are often more sensitive in detecting subtle emphysematous changes. In some cases, arterial blood gas analysis might be necessary to evaluate the oxygen and carbon dioxide levels in the blood.
Differentiating between primary and secondary emphysema often requires a thorough investigation into potential risk factors, such as a family history of alpha-1 antitrypsin deficiency in primary emphysema or a detailed medical history revealing environmental exposures or underlying lung diseases in secondary cases.
Treatment Approaches
Effective management of emphysema focuses on symptom relief and slowing disease progression. Pharmacological therapies are often used to manage symptoms and improve lung function. Bronchodilators, both short-acting and long-acting, help relax the airways, easing breathing. Inhaled corticosteroids can reduce airway inflammation, particularly beneficial in secondary cases where inflammation plays a role. Oxygen therapy might be necessary for patients with low blood oxygen levels.
In advanced cases, surgical interventions, such as lung volume reduction surgery (LVRS) or lung transplantation, are considered. LVRS aims to improve breathing by reducing the volume of diseased lung tissue, while lung transplantation offers a chance at a better quality of life for individuals with severe emphysema.
Pulmonary Rehabilitation
Pulmonary rehabilitation programs are crucial for improving the quality of life and managing the challenges of emphysema. These programs offer a structured approach to enhance respiratory function, exercise capacity, and overall well-being. Educational components address disease management, medication adherence, and lifestyle modifications, empowering patients to actively participate in their care. Exercise training tailored to individual needs helps improve lung function, endurance, and strength, ultimately reducing symptoms and improving quality of life.
Nutritional counseling can help patients maintain a healthy weight and support overall lung health. Psychological support and education on coping mechanisms are important components for managing the emotional and psychological impacts of the disease.
Primary and secondary emphysema are conditions that affect the lungs, often causing breathing difficulties. While exploring these respiratory issues, it’s fascinating to consider how anxiety and fear can manifest in other areas of health, like with celiac disease, impacting a person’s relationship with food as explored in this helpful resource about celiac disease anxiety fear of food.
Ultimately, understanding the multifaceted nature of health challenges, from lung conditions to digestive concerns, is crucial for comprehensive well-being. This deeper understanding can be a powerful tool for better management of primary and secondary emphysema.
Potential Complications
Complications associated with emphysema can significantly impact patients’ health and well-being. Respiratory failure, a serious complication, can necessitate supplemental oxygen or mechanical ventilation. Pneumonia and other infections are more common in individuals with compromised lung function. Patients with severe emphysema might experience pneumothorax, a condition where air leaks into the space between the lungs and the chest wall.
Cor pulmonale, a condition where the right side of the heart enlarges due to increased pressure in the pulmonary arteries, is a significant concern in advanced emphysema. Depression and anxiety can also occur due to the chronic nature of the disease and its impact on daily activities.
Common Diagnostic Tests
| Diagnostic Test | Primary Emphysema | Secondary Emphysema |
|---|---|---|
| Medical History & Physical Exam | Essential for identifying family history of alpha-1 antitrypsin deficiency | Crucial for identifying potential environmental exposures, underlying lung diseases, or smoking history |
| Spirometry | Evaluates airflow limitation, confirms obstruction | Evaluates airflow limitation, confirms obstruction |
| Chest X-ray | May show hyperinflation in advanced cases | May show hyperinflation in advanced cases |
| High-Resolution CT Scan | Identifies subtle emphysematous changes | Identifies subtle emphysematous changes |
| Arterial Blood Gas Analysis | Assesses oxygen and carbon dioxide levels | Assesses oxygen and carbon dioxide levels |
Management Strategies and Prevention
Emphysema, a progressive lung disease, significantly impacts a person’s quality of life. Effective management and proactive prevention strategies are crucial for slowing disease progression and improving outcomes. This section will delve into lifestyle modifications, the vital role of smoking cessation, preventative measures for both primary and secondary emphysema, and the significance of early detection and management. It will also Artikel available support resources.Understanding the modifiable risk factors and implementing appropriate strategies can significantly reduce the risk of developing or worsening emphysema.
Early intervention and adherence to management plans are key to improving long-term health and well-being.
Lifestyle Modifications to Reduce Secondary Emphysema Risk
Modifying certain lifestyle choices can substantially lower the risk of developing secondary emphysema, particularly for those exposed to environmental irritants or with pre-existing lung conditions. Avoiding further exposure to harmful substances and maintaining a healthy lifestyle are paramount.
- Avoiding Environmental Irritants: Reducing exposure to air pollutants, dust, fumes, and other environmental irritants can help mitigate the progression of secondary emphysema. This includes minimizing time spent in smoky environments and taking precautions when working with potentially harmful substances.
- Maintaining a Healthy Diet: A balanced diet rich in fruits, vegetables, and whole grains provides essential nutrients that support overall health and lung function. This can contribute to a stronger immune system and potentially better lung health.
- Regular Exercise: Physical activity improves cardiovascular health and strengthens the respiratory system, potentially slowing the progression of the disease. Regular exercise is crucial for maintaining overall well-being and supporting lung function.
The Role of Smoking Cessation in Managing Secondary Emphysema
Smoking is the leading cause of secondary emphysema. Quitting smoking is paramount in managing and preventing further progression of the disease. Nicotine replacement therapies, counseling, and support groups can greatly enhance the success of quitting.
- Immediate Benefits of Cessation: Stopping smoking immediately reduces exposure to harmful chemicals, leading to a noticeable improvement in lung function and a reduction in inflammation.
- Long-Term Effects of Cessation: Long-term smoking cessation reduces the risk of exacerbations and further lung damage, improving overall quality of life and reducing the need for intensive medical interventions.
- Support for Smoking Cessation: Nicotine replacement therapy, counseling, and support groups are available to assist individuals in quitting smoking. These resources provide guidance and encouragement, increasing the chances of success.
Preventive Strategies for Primary and Secondary Emphysema
Preventive measures for both primary and secondary emphysema focus on reducing exposure to risk factors and promoting overall lung health. Early detection and prompt management are critical in preventing disease progression.
- Avoiding Exposure to Risk Factors: Recognizing and avoiding known risk factors such as smoking, exposure to pollutants, and certain infections can help prevent both primary and secondary emphysema. This proactive approach is crucial for maintaining lung health.
- Promoting Healthy Lung Function: Maintaining good lung function through a healthy diet, regular exercise, and avoiding irritants supports overall respiratory health, potentially reducing the risk of emphysema development or progression.
Importance of Early Detection and Management
Early detection and management of emphysema, regardless of its type, are vital for slowing the progression of the disease and improving the patient’s quality of life.
- Prompt Diagnosis: Early diagnosis allows for timely intervention and personalized treatment plans, which can significantly impact the course of the disease. Regular check-ups and prompt medical attention are critical for early detection.
- Proactive Treatment: Early management strategies can help slow the decline in lung function, improve symptoms, and prevent complications. Working closely with healthcare providers is essential for effective management.
Support Groups and Resources for Patients
Support groups and resources are crucial for individuals living with emphysema. These provide emotional support, practical advice, and a sense of community.
- Patient Advocacy Groups: Numerous patient advocacy groups offer valuable information, support, and resources to individuals affected by emphysema.
- Online Communities: Online forums and communities provide a platform for patients to connect, share experiences, and find support from others facing similar challenges.
- Healthcare Professionals: Healthcare professionals can provide guidance, support, and access to additional resources.
Emerging Research and Future Directions
The fight against emphysema, both primary and secondary, is a multifaceted endeavor. While current treatments focus on symptom management and slowing disease progression, ongoing research promises innovative approaches to potentially revolutionize how we approach this debilitating lung condition. Understanding the complexities of the disease’s underlying mechanisms, along with identifying personalized treatment strategies, are key to unlocking a brighter future for those affected.Recent advancements in our understanding of the immune response, genetic predispositions, and the intricate interplay of environmental factors are paving the way for targeted therapies.
These advancements are not just theoretical; they are already translating into promising clinical trials, with the potential to alter the trajectory of emphysema for countless individuals.
Current Research Areas
Research into emphysema is tackling several key areas simultaneously. These investigations encompass diverse aspects, from the genetic underpinnings to the potential of novel therapies. The exploration of specific genetic mutations linked to primary emphysema is yielding crucial insights. Furthermore, research is actively investigating the role of the microbiome in both disease development and progression.
Potential Future Treatment Strategies and Therapies
Future treatment strategies will likely focus on targeted therapies. These could include gene therapies aimed at correcting genetic defects, immunomodulatory drugs to mitigate inflammation, and even cell-based therapies to restore lung function. Furthermore, novel drug delivery systems could improve the efficacy of existing treatments, enabling more precise targeting of affected areas in the lung. One example is the development of inhalable drugs that can specifically deliver therapeutic agents to the airways.
Impact of Personalized Medicine
Personalized medicine is poised to transform the management of emphysema. By analyzing an individual’s genetic profile, environmental exposures, and specific disease characteristics, clinicians can tailor treatment plans. This approach will enable more effective interventions, potentially leading to improved outcomes and reduced side effects. For example, individuals with specific genetic predispositions to primary emphysema could receive targeted therapies from the outset, potentially delaying or preventing disease progression.
Overview of Ongoing Clinical Trials
Numerous clinical trials are currently underway, exploring the efficacy of various treatment strategies. These trials are investigating novel therapies and evaluating the long-term effects of existing treatments. For instance, several trials are evaluating the effectiveness of specific anti-inflammatory drugs in reducing the progression of emphysema in patients with secondary emphysema associated with smoking.
Visual Representation of Research Areas
A comprehensive visual representation of the current research areas could be a mind map, showing interconnected nodes for genetic factors, environmental triggers, immune response pathways, and potential therapies. Each node would be linked to relevant research studies and clinical trials. Such a visual would highlight the interconnectedness of various research avenues, emphasizing the collaborative nature of the field.
Imagine a large, central node representing “Emphysema Research.” Radiating outward from this node would be smaller nodes representing “Genetic Factors,” “Environmental Factors,” “Immune Response,” “Therapeutic Approaches,” and “Personalized Medicine.” Arrows connecting these nodes would illustrate the relationships between them.
Last Word
In conclusion, both primary and secondary emphysema present unique challenges in diagnosis and treatment. Recognizing the genetic predisposition in primary cases and the environmental triggers in secondary cases is crucial. Understanding the underlying pathophysiology, from genetic mutations to chronic inflammation, provides valuable insights into managing the disease. The importance of early detection, lifestyle modifications, and pulmonary rehabilitation cannot be overstated in improving patient outcomes and quality of life.
Let’s strive for a better future for those affected by these forms of emphysema.
