Pain relief during labor is a crucial aspect of the birthing experience. This comprehensive guide explores the various methods available, from natural techniques to pharmacological interventions, to help women navigate the challenges of labor pain. We’ll delve into the different types of pain, the physiological mechanisms behind them, and the different stages of labor where pain perception may vary.
Understanding the options available for pain relief can empower expectant mothers to make informed decisions about their birthing plans, promoting a positive and comfortable experience. This exploration will cover everything from relaxation techniques and breathing exercises to medication choices and combined approaches, including specific considerations for Cesarean deliveries.
Overview of Labor Pain Relief

Labor is a transformative experience, marked by a unique array of physical and emotional sensations. Understanding the nature of labor pain is crucial for both women experiencing it and the healthcare providers supporting them. This involves recognizing the different types of pain, the physiological mechanisms behind it, and how pain perception evolves throughout the various stages of labor. This understanding is essential for choosing the most appropriate pain relief strategies.The pain of labor arises from a complex interplay of factors.
Uterine contractions, stretching of the cervix and vagina, pressure on surrounding tissues, and the psychological stress of the experience all contribute to the overall discomfort. This multifaceted nature of labor pain underscores the importance of individualized approaches to pain management.
Types of Labor Pain
Labor pain is not a uniform experience. Women describe a wide range of sensations, from sharp, stabbing pains to dull, aching cramps. The intensity and character of pain can vary significantly between individuals and even within the same labor. Common pain descriptors include: sharp, cramping, aching, pressure, burning, and throbbing.
Finding pain relief during labor can be tough, but some strategies might surprise you. While focusing on natural remedies, exploring options like incorporating leafy greens into your diet might offer unexpected benefits, potentially impacting overall health, as seen in research on leafy greens multiple sclerosis treatment leafy greens multiple sclerosis treatment. Ultimately, though, the most effective approach for pain relief during labor is often a personalized one, considering individual needs and preferences.
Physiological Mechanisms of Labor Pain
The physiological mechanisms behind labor pain are intricate. Uterine contractions are initiated by hormonal signals, primarily oxytocin. These contractions cause mechanical stress on the cervix, vagina, and surrounding tissues. Furthermore, the stretching of these tissues generates nerve impulses that transmit pain signals to the brain. The intensity of these contractions and the resulting pain are directly influenced by factors such as the strength of uterine contractions, the rate of cervical dilation, and the position of the baby.
Stages of Labor and Pain Perception
The experience of labor pain evolves across the three stages. In the first stage, contractions are typically irregular and mild, initially leading to mild discomfort. As labor progresses, contractions become more frequent, stronger, and longer, resulting in more intense pain. In the second stage, the focus shifts to pushing, which often involves a combination of intense pressure and bearing-down sensations.
In the third stage, pain is usually less intense as the focus shifts to the delivery of the placenta.
Comparison of Pain Relief Methods
| Method | Mechanism | Effectiveness | Potential Side Effects |
|---|---|---|---|
| Epidural Anesthesia | Blocks nerve signals in the lower spine, reducing pain signals to the brain. | Generally highly effective in relieving pain, especially in the second stage. | Potential for hypotension (low blood pressure), nausea, itching, urinary retention, and, in rare cases, headache. |
| Spinal Anesthesia | Provides rapid pain relief by injecting anesthetic directly into the spinal fluid. | Highly effective for short-term pain relief, often used for cesarean sections. | Potential for similar side effects to epidural anesthesia, including headache and hypotension. |
| Nitrous Oxide | Provides a mild analgesic effect, reducing pain perception by altering brain function. | Generally effective for managing pain during contractions. | Potential for dizziness, nausea, or disorientation. It’s not a complete pain reliever. |
| Pain Medications (e.g., opioids) | Bind to opioid receptors in the brain, reducing pain perception. | Can be effective for managing pain, especially in the first and second stages. | Potential for respiratory depression, nausea, vomiting, and constipation. Also, dependence potential with prolonged use. |
Non-Pharmacological Pain Relief Techniques: Pain Relief During Labor
Navigating labor can be overwhelming, but knowing effective non-pharmacological methods can significantly ease the experience. These techniques empower birthing individuals to actively participate in managing their pain, fostering a sense of control and well-being. They often complement and enhance the effectiveness of other pain relief options, and are particularly valuable for those who prefer to avoid medication.
Relaxation Techniques for Managing Labor Pain
Relaxation techniques are crucial for labor pain management. They help to reduce muscle tension, slow the heart rate, and promote a sense of calm. Progressive muscle relaxation, guided imagery, and deep breathing are examples of powerful tools. These techniques help to divert attention from the discomfort of labor contractions and promote a sense of inner peace. Practicing these techniques before labor begins can make a significant difference during the birthing process.
Breathing Exercises and Their Impact on Pain Perception
Effective breathing techniques can significantly alter pain perception during labor. Controlled breathing exercises, such as the patterned breathing technique, can help to slow the heart rate, reduce anxiety, and promote relaxation. By focusing on the breath, individuals can redirect their attention away from the pain and toward a more positive experience. This conscious control over breathing can create a sense of calm and empowerment.
Different types of breathing techniques can be adapted to suit individual needs and preferences.
The Role of Massage and Touch in Labor Pain Relief
Massage and touch play a significant role in pain relief during labor. The release of endorphins, natural pain relievers, is often triggered by physical touch. Massage can help to alleviate muscle tension and promote relaxation, reducing discomfort and creating a sense of well-being. Warm compresses, back rubs, and gentle touch can also provide comfort. A supportive partner or doula can be instrumental in providing this form of pain relief.
Hydrotherapy and its Effectiveness in Pain Management
Hydrotherapy, or water therapy, offers a soothing and effective approach to labor pain relief. The buoyancy and warmth of water can reduce muscle tension and ease the pressure on joints. A warm bath or shower can significantly reduce pain perception during labor. This technique can be particularly effective in managing lower back pain. The sensory experience of being immersed in water can promote a sense of calm and well-being.
Non-Pharmacological Methods for Labor Pain Relief
| Method | Advantages | Disadvantages | Application |
|---|---|---|---|
| Relaxation Techniques | Reduces muscle tension, promotes calmness, and redirects focus | Requires practice and focus, may not be effective for everyone | Throughout labor, can be used in conjunction with other methods |
| Breathing Exercises | Helps regulate the heart rate, reduces anxiety, and alters pain perception | Requires conscious effort and practice, may not be suitable for all individuals | During contractions, can be adapted to different intensities |
| Massage and Touch | Releases endorphins, alleviates muscle tension, and promotes relaxation | Requires a supportive partner or professional, may not be effective for everyone | Can be applied throughout labor, particularly to tense muscles |
| Hydrotherapy | Reduces muscle tension, eases pressure on joints, and provides comfort | May not be suitable for all individuals or locations, may require special equipment | Can be used in various stages, especially during active labor |
Flow Chart for Non-Pharmacological Techniques
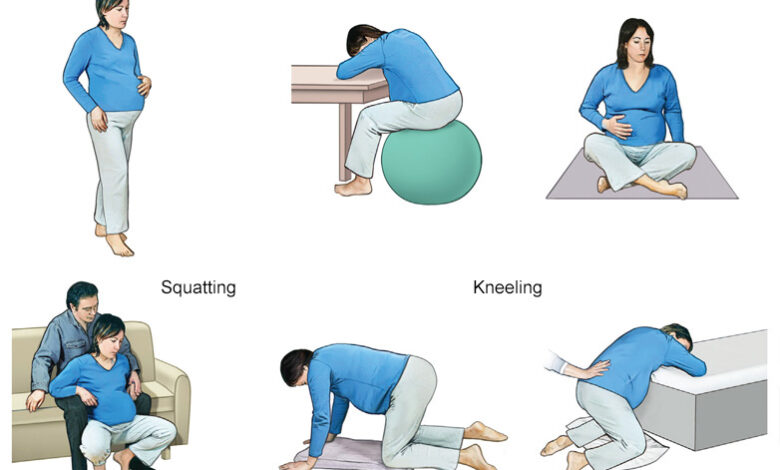
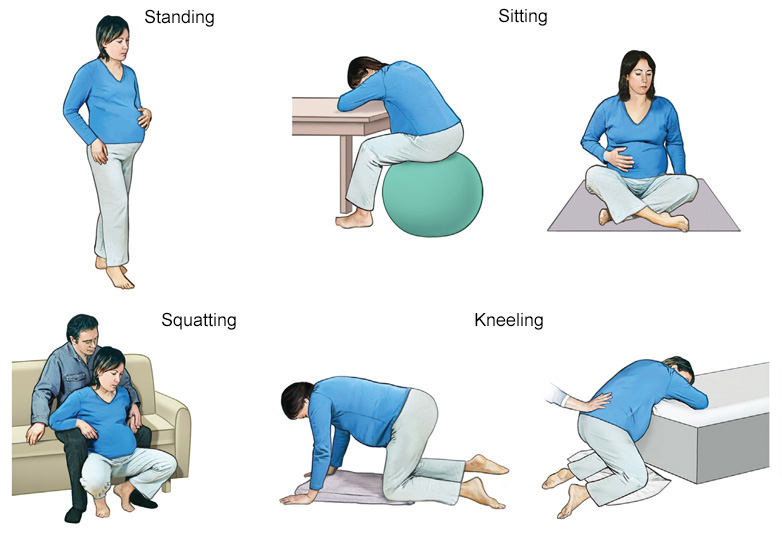
(A visual flow chart would be best for this, but cannot be created here.)A suggested sequence of non-pharmacological techniques could begin with relaxation techniques and breathing exercises. During contractions, hydrotherapy, massage, and touch could be integrated. The choice of techniques should be individualized, considering the birthing person’s preferences and needs. A birthing partner or doula can guide the birthing person through the process.
Pharmacological Pain Relief Options
Easing labor pain is a crucial aspect of childbirth, and various pharmacological options are available to help manage discomfort. These medications work in different ways, impacting the body’s perception of pain. Understanding the benefits, risks, and considerations surrounding these options empowers both expecting mothers and healthcare providers to make informed decisions.
Types of Analgesics Used for Labor Pain Relief
Different types of analgesics target different aspects of the pain experience. Some work by blocking pain signals in the nervous system, while others reduce the intensity of pain perception. The choice of medication often depends on the stage of labor, the woman’s medical history, and individual preferences.
Mechanism of Action of Each Type of Medication, Pain relief during labor
Analgesics work through various mechanisms, altering the body’s response to pain. Opioids, for instance, bind to opioid receptors in the brain and spinal cord, decreasing pain signals. Local anesthetics work by blocking nerve impulses, providing temporary numbness in a specific area. Epidurals, a type of regional anesthetic, numb the lower part of the body by injecting medication into the epidural space.
Potential Side Effects and Contraindications of Each Medication
Each medication carries potential side effects and contraindications. Opioids, while effective, can cause respiratory depression in the mother and newborn. Local anesthetics, like those used for pudendal blocks, can lead to temporary numbness or tingling in the treated area. Epidurals can cause headaches, itching, and urinary retention. Contraindications include certain medical conditions and allergies.
Careful consideration of individual circumstances is vital to mitigate potential risks.
Examples of Common Pain Medications Used During Labor
Common pain medications used during labor include various opioids like fentanyl and morphine. Regional anesthetics, including epidurals and spinal blocks, are also frequently employed. Local anesthetics, like those used for pudendal blocks, are another option. The specific choice often depends on the circumstances and preferences of the birthing person.
Comparison of Pharmacological Pain Relief Methods
| Medication | Mechanism | Side Effects | Contraindications |
|---|---|---|---|
| Opioids (e.g., fentanyl, morphine) | Bind to opioid receptors, reducing pain signals. | Respiratory depression (mother and newborn), nausea, vomiting, itching, constipation. | Pre-existing respiratory conditions, certain allergies. |
| Epidural Anesthetics | Inject medication into the epidural space to numb the lower body. | Headaches, itching, urinary retention, hypotension, fever. | Coagulation disorders, infection at the injection site, certain neurological conditions. |
| Spinal Anesthetics | Inject medication into the spinal fluid to numb the lower body. | Similar to epidurals, but with a quicker onset and shorter duration. | Similar to epidurals, but with potential for higher risk of hypotension. |
| Local Anesthetics (e.g., pudendal block) | Block nerve impulses in a specific area. | Numbness, tingling, temporary discomfort at the injection site. | Hypersensitivity to local anesthetics, bleeding disorders. |
Factors Influencing the Choice of Pharmacological Pain Relief Method
Several factors influence the selection of a pain relief method during labor. These include the stage of labor, the woman’s medical history, any allergies or pre-existing conditions, her preferences, and the healthcare provider’s assessment. The overall goal is to provide effective pain relief while minimizing potential risks.
Combined Approaches to Pain Management
Labor pain can be overwhelming, but it doesn’t have to be unbearable. Understanding the various options and how they can be combined effectively can empower expecting parents to make informed choices about their pain relief during labor. This approach recognizes the individuality of each woman’s experience and allows for a customized strategy.Effective pain management during labor often involves a multifaceted strategy.
This means combining non-pharmacological techniques with pharmacological options, or even utilizing a combination of different pharmacological approaches. The goal is to achieve the best possible balance between pain relief and overall well-being. A collaborative effort between the expectant parent, their support system, and healthcare providers is crucial to achieving optimal outcomes.
Optimizing Pain Relief Through Combined Strategies
Combining non-pharmacological and pharmacological methods can significantly enhance pain relief during labor. For example, using relaxation techniques alongside epidural analgesia can reduce the required dosage of medication, minimizing potential side effects. This synergy can provide more comfortable and manageable labor experiences. By combining different strategies, expectant parents can tailor their pain relief plan to their specific needs and preferences.
The Role of Support Persons
Labor support persons play a vital role in managing pain during labor. Their presence provides emotional support, encouragement, and practical assistance. This support system can also help the expectant parent stay focused on non-pharmacological techniques such as breathing exercises, massage, or movement. Their understanding of the expectant parent’s preferences and comfort levels is essential. Support persons can act as advocates, ensuring the expectant parent’s voice is heard and their needs are met.
Individual Preferences and Circumstances
Individual preferences and circumstances significantly influence the choice of pain relief strategies. Factors such as cultural background, previous experiences with pain, and personal beliefs all play a role in the expectant parent’s decisions. For instance, some expectant parents might prefer a more natural approach, relying heavily on non-pharmacological techniques, while others might prioritize immediate and significant pain relief through pharmacological interventions.
Finding effective pain relief during labor can be tough, and it’s important to explore all options. While some dietary choices can impact overall health, like those linked to an increased risk of heart disease, the diets associated with increased risk of heart disease , it’s crucial to remember that pain management during labor is a very personal journey.
Different methods work for different people, and ultimately, the goal is to find what feels best for you and your body.
A healthcare provider should carefully assess the expectant parent’s unique needs and preferences to create a personalized plan.
Cultural Factors
Cultural factors can significantly influence pain relief preferences during labor. Some cultures prioritize natural pain management methods, while others might have different expectations regarding the use of medication. It is essential for healthcare providers to be sensitive to these cultural nuances and respect the expectant parent’s choices, offering culturally appropriate support and pain relief options. Understanding and respecting cultural norms can enhance the effectiveness of pain management strategies.
Patient Testimonials
“I was hesitant about using medication, but combining the breathing techniques with the epidural was the perfect balance. I felt empowered and in control of my labor experience.”
Sarah M.
“The support from my doula was incredible. She guided me through different relaxation techniques and helped me stay focused during the contractions, making the experience so much more manageable.”
Emily S.
“My cultural background emphasizes natural remedies. The combination of acupressure, warm compresses, and aromatherapy helped me manage the pain without medication. It was a beautiful experience.”
Maria A.
Pain Relief During Cesarean Delivery
Navigating the experience of a cesarean delivery involves careful consideration of pain management strategies. Understanding the available options, their potential benefits and risks, and how they compare to vaginal delivery pain management is crucial for both the expecting mother and the medical team. This section will delve into the specifics of pain relief during a cesarean section, highlighting the types of anesthesia used, and the potential risks and benefits of each.Cesarean deliveries, while often necessary for the health of mother and baby, involve surgical incisions that require significant pain management.
The methods employed during a cesarean aim to minimize discomfort and promote a smoother recovery process. The choice of pain relief often depends on various factors, including the specific circumstances of the delivery, the patient’s preferences, and the expertise of the medical team.
Pain Management Strategies During Cesarean Delivery
Effective pain management during a cesarean section is crucial for patient comfort and well-being. This is accomplished through a variety of strategies, ranging from regional anesthesia to general anesthesia.
Types of Anesthesia Used
A variety of anesthetic techniques are utilized during cesarean deliveries, each with its own advantages and disadvantages. Regional anesthesia, which numbs a specific area of the body, is a common choice. This often involves spinal or epidural anesthesia. General anesthesia, which renders the patient unconscious, is also an option, but it carries potential risks to both the mother and the baby.
Comparison of Cesarean and Vaginal Delivery Pain Management
Cesarean delivery pain management differs from vaginal delivery pain management due to the surgical nature of the procedure. While vaginal delivery pain relief often focuses on techniques to manage contractions, cesarean delivery requires pain relief for the surgical incision. Vaginal delivery often involves non-pharmacological techniques and perhaps regional analgesia, whereas cesarean deliveries often necessitate more substantial forms of pain control, including regional or general anesthesia.
Potential Risks and Benefits of Different Pain Relief Options
Each anesthetic method carries its own set of potential risks and benefits. Regional anesthesia, while offering a faster recovery, can potentially lead to complications like headache or nerve damage. General anesthesia, while providing complete pain relief, carries the risk of complications for both the mother and the baby, including potential respiratory depression or problems during the recovery period.
Specific Pain Relief Methods for Cesarean Delivery
| Method | Administration | Duration of Action | Potential Side Effects |
|---|---|---|---|
| Spinal Anesthesia | Injection into the spinal canal | Typically 1-2 hours | Headache, nausea, vomiting, hypotension (low blood pressure), and potential spinal or nerve injury |
| Epidural Anesthesia | Injection into the epidural space | Variable, depending on the level of blockade | Headache, nausea, vomiting, hypotension, pruritus (itching), and potential nerve damage |
| General Anesthesia | Inhalation or intravenous administration | Variable, depending on the duration of the procedure | Respiratory depression, aspiration, nausea, vomiting, and potential complications for the mother and the baby, including prolonged recovery time |
Surgical Site and Placement of Pain Relief Methods
During a cesarean section, the incision is typically made in the lower abdomen, often along the midline. The placement of pain relief methods depends on the type of anesthesia chosen. For example, with spinal anesthesia, the needle is inserted into the subarachnoid space within the spinal canal, blocking pain signals from the lower part of the body. With epidural anesthesia, the catheter is inserted into the epidural space, a space outside the dura mater, allowing for continuous pain relief.
The location of the catheter placement will be dependent on the desired level of pain relief, and will be determined by the anesthesiologist.
Finding pain relief during labor can be tough, but imagine a world where natural methods like hypnobirthing or aromatherapy could ease those contractions. Just as talking to babies in baby talk can significantly speed up their language development, having a conversation in baby talk can speed up infants language development , exploring different relaxation techniques might help manage discomfort during labor.
Ultimately, focusing on positive coping strategies during this special time can make a world of difference in the birthing experience.
Pain Relief and Maternal Wellbeing
Labor is a transformative experience, fraught with intense physical and emotional challenges. Effective pain management during this period is not just about alleviating discomfort; it’s intrinsically linked to the mother’s overall well-being, impacting her ability to cope, bond with her newborn, and even her postpartum recovery. Understanding this connection is crucial for providing comprehensive and supportive care.A woman’s experience of labor is profoundly personal, but a shared understanding of the importance of pain relief on maternal well-being is vital.
The physical and emotional toll of intense pain can significantly hinder a woman’s ability to navigate the birthing process. Adequate pain relief can foster a sense of control and empowerment, allowing her to engage more fully with the experience and build a stronger connection with her baby.
The Connection Between Pain Relief and Coping Mechanisms
Effective pain management significantly enhances a laboring woman’s ability to cope with the physical demands of labor. When pain is effectively controlled, women report feeling more capable, less overwhelmed, and better equipped to manage contractions and other physical discomforts. This increased sense of control translates into better emotional regulation, reducing anxiety and fear, and promoting a more positive labor experience.
For example, a woman who feels adequately supported and pain-managed may be more likely to engage in relaxation techniques or other coping strategies, further facilitating her labor progression.
Impact on Breastfeeding and Bonding
The physical and emotional state of the mother during labor directly affects her ability to establish breastfeeding and bond with her newborn. Postpartum pain, fatigue, and emotional distress can negatively impact the mother’s capacity to engage in the immediate postpartum care and bonding with her baby. Adequate pain relief can facilitate a smoother transition to the postpartum period, enabling mothers to focus on their newborns and establish a positive nursing relationship.
For example, a mother experiencing minimal pain may be able to attend to her newborn’s needs more effectively, fostering early bonding and a stronger connection.
Psychological Effects of Inadequate Pain Relief
Inadequate pain relief during labor can have a range of psychological consequences, potentially impacting the mother’s postpartum mental health. The experience of intense and uncontrolled pain can lead to feelings of helplessness, anxiety, and even post-traumatic stress. This can manifest in difficulties coping with the postpartum period, impacting her ability to bond with her baby and manage the challenges of motherhood.
A mother experiencing prolonged and severe pain may feel isolated, distressed, and unable to effectively engage in positive interactions with her infant.
Potential Impacts of Pain Relief on Maternal Wellbeing
| Aspect | Positive Impacts | Negative Impacts | Considerations |
|---|---|---|---|
| Physical Well-being | Reduced pain and discomfort, improved ability to cope with contractions, decreased risk of complications | Potential for side effects from medication, increased risk of certain complications if medication is not used appropriately. | Individual responses to pain relief vary; careful monitoring and individualized approaches are crucial. |
| Emotional Well-being | Reduced anxiety and fear, increased sense of control, improved mood, and increased confidence | Potential for side effects of medication impacting mood or cognitive function, potential for fear of the unknown regarding the effects of pain relief. | Prioritize the mother’s emotional needs and support throughout the labor process. |
| Mother-Infant Bonding | Increased ability to attend to newborn needs, enhanced opportunities for skin-to-skin contact and early bonding | Potential for medication impacting the newborn, potential for decreased engagement due to pain. | Ensure mothers are informed about potential side effects and that appropriate precautions are taken for the newborn. |
| Postpartum Recovery | Reduced physical and emotional stress, improved ability to care for the newborn | Potential for long-term side effects from medication, potential for prolonged recovery if pain is not managed appropriately. | Address potential concerns and provide ongoing support to aid in the transition. |
Importance of Emotional Support
Emotional support plays a pivotal role in helping mothers cope with pain during labor. A supportive environment, provided by healthcare providers, partners, and family members, can significantly reduce the mother’s anxiety and stress. This support can take various forms, including encouragement, reassurance, and simply being present during challenging moments. A supportive partner can provide comfort and encouragement, offering distraction techniques and a sense of companionship.
Conclusive Thoughts
In conclusion, managing pain during labor is a multifaceted process that requires a personalized approach. From natural methods to pharmacological options, and the potential integration of both, this guide provides a holistic overview. Ultimately, the best pain relief strategy is the one that aligns with the individual needs, preferences, and circumstances of the birthing person. This knowledge empowers women to make informed decisions and experience labor with increased comfort and confidence.
