Preventive artery repair recommended after heart attacks is a crucial procedure for patients aiming to prevent future heart issues. This innovative approach offers a targeted solution for those who’ve experienced a myocardial infarction (MI). The procedure involves repairing damaged arteries to enhance blood flow, reducing the risk of another heart attack. Different techniques exist, each with its own advantages and disadvantages, and understanding these options is key to making informed decisions.
This detailed look into the process explores patient selection criteria, surgical techniques, post-operative care, potential risks, and long-term outcomes, ultimately empowering individuals to understand the nuances of this life-saving intervention.
The rationale behind preventive artery repair (PAR) after a heart attack centers around the concept of preventing future cardiac events. By addressing the damaged arteries, PAR aims to improve blood flow, reducing the risk of another heart attack and enhancing overall cardiovascular health. This proactive approach is designed to significantly improve patient outcomes and quality of life. The process involves careful patient evaluation and personalized surgical approaches, ensuring the best possible outcome for each individual.
Introduction to Preventive Artery Repair
Preventive artery repair (PAR) is a crucial intervention for individuals who have experienced a heart attack (myocardial infarction, or MI). It focuses on proactively addressing the underlying arterial damage that contributed to the initial event, thereby reducing the risk of future heart attacks and related complications. The goal of PAR is to prevent future damage by improving blood flow and strengthening the affected arteries.The rationale for performing PAR after an MI stems from the understanding that the initial heart attack often results from a compromised artery, typically blocked by atherosclerotic plaque.
This plaque buildup, if left unaddressed, can continue to grow and potentially cause another heart attack. PAR aims to mitigate this risk by either restoring blood flow to the affected area or by reinforcing the artery wall, preventing further blockages.
So, preventive artery repair is often recommended after a heart attack to help prevent future issues. But beyond the medical procedures, a crucial component to overall heart health is plant-based nutrition fueling workouts. Plant based nutrition fueling workouts can significantly contribute to a healthier heart and recovery, ultimately supporting the effectiveness of the preventive artery repair.
Maintaining a strong heart health strategy, combining medical interventions with a healthy lifestyle, is key.
Different Types of PAR Procedures
Various procedures fall under the umbrella of PAR, each with its own advantages and disadvantages. These techniques are tailored to the specific needs of each patient, considering the extent of arterial damage and overall health.
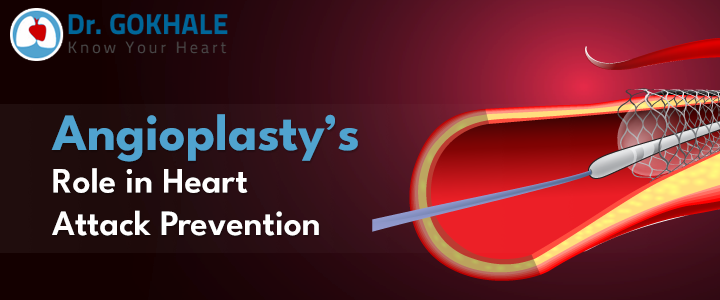
- Angioplasty with Stenting: This common procedure involves inserting a balloon catheter into the affected artery to widen the narrowed or blocked section. A small metal mesh tube (stent) is then placed within the artery to keep it open. The advantage is the immediate restoration of blood flow. A disadvantage is the possibility of complications like stent thrombosis (blood clot formation within the stent) or restenosis (re-narrowing of the artery).
- Artery Bypass Grafting: In this procedure, a healthy blood vessel (either from the patient’s own body or a donor) is used to create a detour around the blocked portion of the artery. This improves blood flow to the heart muscle. Advantages include addressing severe blockages and improving long-term blood flow. Potential disadvantages include the need for a larger incision and a longer recovery period compared to angioplasty.
- Atherectomy: This procedure removes plaque buildup from the artery walls using a specialized device. It’s often employed in conjunction with angioplasty. The benefit is removing the plaque directly, but it may not be suitable for all cases of severe blockage.
Historical Context of PAR Development
The development of PAR procedures reflects a continuous evolution in cardiovascular care. Early attempts focused on treating acute heart attacks, but the understanding of the underlying causes and long-term implications of atherosclerosis led to the development of preventive strategies. This historical context demonstrates the shift from crisis management to proactive interventions, leading to improved patient outcomes.
Types of PAR Procedures: A Comparative Overview
| Procedure | Mechanism of Action | Typical Recovery Time |
|---|---|---|
| Angioplasty with Stenting | Widens blocked artery, inserts stent to maintain patency. | Generally, a few days to a couple of weeks. Full recovery can take several months. |
| Artery Bypass Grafting | Creates a new pathway for blood flow around the blockage using a graft vessel. | Typically a longer recovery period, ranging from several weeks to several months. Full recovery can take several months to a year, depending on the patient’s overall health and the complexity of the procedure. |
| Atherectomy | Removes plaque buildup from the artery walls. | Recovery time is generally shorter than bypass surgery but longer than angioplasty, typically several days to a few weeks. |
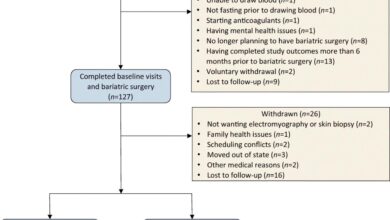
Patient Selection Criteria: Preventive Artery Repair Recommended After Heart Attacks
Choosing the right patients for Preventive Artery Repair (PAR) after a heart attack is crucial for maximizing benefits and minimizing risks. A careful evaluation process considers various factors, including the patient’s overall health, the extent of coronary artery damage, and their individual risk profile. This personalized approach ensures that PAR is offered only to those who stand to gain the most from the procedure.The decision to recommend PAR is multifaceted, taking into account a range of risk factors and their interplay.
A thorough pre-operative assessment is essential for identifying those who are most likely to benefit from the procedure while mitigating potential complications. This process also involves detailed diagnostic testing to evaluate the patient’s suitability.
Specific Patient Populations Benefiting from PAR
Patients who have experienced a heart attack and exhibit significant stenosis (narrowing) in a crucial artery, often accompanied by impaired blood flow, are prime candidates for PAR. This is particularly true for those with a high likelihood of future heart events or those who have already experienced recurrent episodes. Individuals with a history of unstable angina, a condition marked by chest pain that fluctuates, are also strong candidates if the underlying cause is amenable to repair.
Risk Factors Influencing PAR Recommendation
Various risk factors influence the decision-making process regarding PAR. These include age, smoking history, blood pressure, blood sugar levels, cholesterol levels, and the presence of other co-morbidities like diabetes or kidney disease. A detailed medical history and physical examination help in evaluating the overall risk profile. The severity and location of the artery blockage are also critical factors, as these influence the procedure’s potential effectiveness and safety.
Importance of Pre-operative Assessment
Thorough pre-operative assessment is vital to identify potential complications and adjust the treatment plan accordingly. This involves a comprehensive evaluation of the patient’s medical history, current medications, and any underlying conditions. A thorough physical examination, including blood pressure, heart rate, and other vital signs, is performed. This assessment aims to identify any factors that could increase the risk of complications during or after the procedure.
A detailed discussion with the patient about the risks and benefits of PAR is also a critical part of the pre-operative assessment.
Diagnostic Tests and Procedures
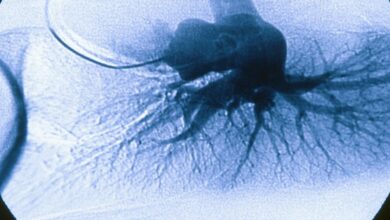
Several diagnostic tests and procedures are employed to assess a patient’s suitability for PAR. These include cardiac catheterization, which involves inserting a thin tube into the heart to visualize the coronary arteries and assess the extent of blockage. Coronary angiography provides detailed images of the coronary arteries, allowing clinicians to identify the specific location and severity of any blockages.
Electrocardiograms (ECGs) and stress tests are also used to evaluate the heart’s response to exertion. These tests help in assessing the patient’s overall cardiovascular health and the potential risks associated with the procedure.
Summary of Key Criteria for Patient Selection
| Criterion | Description | Example |
|---|---|---|
| Age | Patients of all ages can be considered, but younger patients with significant stenosis may benefit more from PAR. | A 55-year-old with severe blockage in the left anterior descending artery might be a good candidate. |
| Medical History | History of heart attacks, angina, diabetes, hypertension, and other cardiovascular conditions. | A patient with a history of multiple heart attacks and high blood pressure may be a higher risk candidate for PAR. |
| Anatomical Considerations | Location and severity of coronary artery stenosis. | A blockage in a major artery like the left main coronary artery may require PAR. |
Surgical Techniques and Procedures
Preventive Artery Repair (PAR) encompasses a spectrum of surgical techniques tailored to address the specific needs of each patient. The choice of approach hinges on the location and extent of the diseased artery, the patient’s overall health, and the surgeon’s expertise. Minimally invasive techniques are increasingly popular due to their reduced recovery time and lower risk of complications.
Surgical Steps in Different PAR Procedures
The precise surgical steps vary depending on the specific PAR procedure, but generally involve these key stages: initial assessment of the affected artery, careful dissection to isolate the diseased segment, and replacement or repair of the damaged artery. Crucial steps include meticulous hemostasis (controlling bleeding) to minimize blood loss and careful handling of the surrounding tissues to avoid damage to critical structures.
The restoration of normal blood flow is paramount, achieved by precise anastomosis (joining) of the healthy artery segments.
Surgical Approaches for PAR
Several surgical approaches are used in PAR, each with its own advantages and disadvantages. Open surgery involves a larger incision, providing direct access to the targeted artery. Minimally invasive techniques, such as endovascular approaches, use smaller incisions and specialized catheters, often reducing patient recovery time and discomfort. Robotic surgery, another advancement, employs robotic arms to perform precise procedures with enhanced visualization, further minimizing invasiveness.
Instruments and Technologies in PAR
A wide array of instruments and technologies are employed in PAR. Surgical microscopes, ultrasonic devices, and specialized imaging techniques, such as intraoperative angiography, facilitate precise identification and assessment of the diseased artery. Surgical staplers, sutures, and vascular grafts are used for repairing or replacing the affected artery segment. The advent of advanced materials, like biocompatible grafts, has expanded the range of repair options, contributing to improved outcomes.
Minimizing Surgical Trauma and Complications
Minimizing surgical trauma and complications is a core focus in PAR. Surgeons employ meticulous surgical techniques, precise instrument handling, and careful monitoring of vital signs throughout the procedure. The use of advanced imaging tools ensures accurate identification of the target vessel, thereby minimizing the risk of unintended damage to surrounding tissues. Careful hemostasis, precise suture placement, and the selection of appropriate graft materials all contribute to reducing the likelihood of post-operative complications.
Closing the Incision and Post-Operative Care
Closure of the incision involves precise suturing techniques to minimize scarring and ensure proper healing. Post-operative care is crucial, encompassing pain management, medication administration, and close monitoring of vital signs. Patients are typically advised to avoid strenuous activity and adhere to prescribed medication schedules to promote recovery. Follow-up appointments are essential to monitor healing and address any potential complications.
Comparison of Open and Minimally Invasive PAR Techniques
| Characteristic | Open PAR | Minimally Invasive PAR |
|---|---|---|
| Incision Size | Larger | Smaller |
| Recovery Time | Longer | Shorter |
| Hospital Stay | Potentially longer | Potentially shorter |
| Potential Risks | Increased risk of infection, bleeding, and nerve damage | Lower risk of infection, bleeding, and nerve damage |
| Advantages | Direct access to the targeted artery, better visualization | Reduced scarring, less pain, faster recovery |
This table provides a general comparison. Specific risks and benefits depend on individual patient factors and the complexity of the procedure. For example, complex cases may require open surgery despite the longer recovery time.
Post-operative Care and Recovery
The journey after a preventive artery repair (PAR) surgery is crucial for a successful recovery. Post-operative care focuses on managing pain, preventing complications, and supporting the body’s healing process. This phase emphasizes patient education and active participation in the recovery plan. The key is to address potential issues promptly and foster a supportive environment for healing.
Expected Post-operative Course and Recovery Timeline
The recovery period following PAR surgery varies depending on individual factors such as overall health, the extent of the procedure, and any complications. Typically, patients spend one to three days in the hospital. Discharge planning begins well in advance, ensuring a smooth transition to home care. Early ambulation and physical activity, as tolerated, are encouraged to promote circulation and prevent blood clots.
A gradual return to normal activities is expected, with a focus on avoiding strenuous exertion for several weeks post-surgery. Patients are advised to follow their doctor’s instructions meticulously to minimize the risk of complications and accelerate the healing process.
Post-operative Medication Management
Medication management is a critical aspect of post-operative care. Patients are prescribed medications to manage pain, prevent blood clots, and control any underlying health conditions. These medications may include anticoagulants (to prevent blood clots), pain relievers, and potentially blood pressure or cholesterol medications. Adherence to the prescribed medication regimen is essential to achieve optimal results and minimize the risk of complications.
Patients should carefully note the dosage, frequency, and potential side effects of each medication. Close communication with the healthcare team is crucial for any concerns regarding medication.
Following a heart attack, preventive artery repair is often recommended. This crucial step helps to reduce the risk of future heart issues. It’s important to look at the bigger picture of overall well-being, like the initiatives in Howaa City to promote health, as detailed in howaa city gets healthy. Ultimately, these preventative measures, including artery repair, are key to maintaining a healthy heart and a good quality of life.
Monitoring Vital Signs and Potential Complications
Post-surgery, regular monitoring of vital signs such as blood pressure, heart rate, and temperature is crucial. This allows healthcare providers to detect any early signs of complications, such as infection, bleeding, or blood clots. Patients should report any unusual symptoms, including excessive pain, swelling, or changes in breathing, immediately to their healthcare team. Proactive monitoring helps ensure a smooth and complication-free recovery.
Close monitoring is especially important during the first few weeks after surgery.
Rehabilitation Process and Role of Physical Therapy
Physical therapy plays a significant role in the rehabilitation process after PAR. A tailored physical therapy program is often implemented to help patients regain strength and mobility, improve cardiovascular function, and prevent stiffness. Exercises and stretches are gradually introduced to restore normal function and promote healing. The therapy sessions will guide patients in performing safe and effective exercises that enhance their recovery.
Physical therapy sessions can also address any lingering pain or discomfort.
Typical Post-operative Monitoring Schedule and Potential Complications
| Day | Monitoring Focus | Potential Complications |
|---|---|---|
| Days 1-3 (Hospital) | Vital signs (BP, HR, Temp), pain levels, wound healing, intake/output | Bleeding, infection, blood clots, pain management issues, difficulty breathing |
| Days 4-7 (Home) | Vital signs (at home monitoring), medication adherence, wound care, activity levels | Persistent pain, swelling, fever, shortness of breath, signs of infection, difficulty swallowing |
| Weeks 1-4 | Follow-up appointments, physical therapy, gradual return to activities | Ongoing pain, slow healing, blood clots, recurrence of heart attack symptoms |
| Weeks 4+ | Regular check-ups, lifestyle modifications, maintenance medications | Long-term complications, such as persistent chest pain, fatigue, or limited mobility |
Regular follow-up appointments are critical for long-term success and to address any unforeseen issues.
Potential Complications and Risks
Preventive Artery Repair (PAR) is a complex procedure with potential risks, just like any surgical intervention. Understanding these complications is crucial for informed decision-making. While PAR aims to significantly reduce the risk of future heart attacks, it’s essential to acknowledge that no procedure is without potential downsides. Careful consideration of the potential benefits and risks, alongside the patient’s individual health profile, is vital for determining the best course of action.
Potential Surgical Complications
Surgical procedures, by their very nature, carry the risk of complications. These can range from minor issues to more serious problems requiring additional interventions. In the context of PAR, potential complications include bleeding, infection, and damage to surrounding tissues or nerves. The extent of these complications varies significantly depending on factors like the patient’s overall health, the skill of the surgical team, and the specific nature of the procedure.
Thorough preoperative assessments and meticulous surgical techniques are crucial for mitigating these risks.
Long-Term Risks and Benefits
While PAR aims to prevent future heart attacks, long-term complications and benefits need careful consideration. Potential long-term complications might include the need for additional procedures, persistent pain, or limitations in physical activity. The benefits, on the other hand, encompass a reduced risk of future cardiac events and an improved quality of life. The long-term impact of PAR is highly individualized, and careful patient selection and ongoing monitoring are essential.
While preventive artery repair is often recommended after a heart attack, lifestyle changes are crucial for long-term heart health. Cutting out 200 calories a day and exercising regularly, as detailed in this great article , can significantly reduce your risk of future heart issues. These preventative measures, combined with any necessary medical procedures, are key to maintaining a healthy heart and avoiding another attack.
For example, a patient with a history of extensive cardiovascular disease might experience more pronounced long-term effects compared to a younger patient with a less severe history.
Comparison with Alternative Treatments
Alternative treatments for preventing future heart attacks include lifestyle modifications, medication, and other interventional procedures. Each approach has its own set of risks and benefits. For instance, medication may not address the underlying structural issues that PAR addresses directly. A thorough discussion between the patient and their healthcare provider is critical to assess the most appropriate approach given the specific circumstances.
Comparing PAR to other treatments helps determine the optimal approach for each individual.
Minimizing Complications and Risks
Several strategies are employed to minimize the risks associated with PAR. These strategies encompass meticulous surgical technique, appropriate patient selection, and meticulous post-operative care. Experienced surgeons, advanced surgical equipment, and well-equipped post-operative care units contribute significantly to mitigating complications. For instance, employing minimally invasive techniques can reduce the extent of tissue trauma and potential complications.
Potential Complications Summary, Preventive artery repair recommended after heart attacks
| Potential Complication | Frequency (Approximate) | Management Strategies |
|---|---|---|
| Bleeding | Moderate | Blood transfusions, pressure dressings, surgical intervention if necessary |
| Infection | Low | Antibiotics, wound care, possible surgical revision |
| Nerve damage | Low | Physical therapy, pain management, potential surgical intervention |
| Blood clots | Low to Moderate | Anticoagulant medications, compression stockings, early mobilization |
| Stroke | Very Low | Close monitoring, rapid intervention if stroke symptoms arise |
| Heart Attack | Very Low | Immediate medical intervention, cardiac monitoring, appropriate medications |
Long-term Outcomes and Success Rates
Preventive Artery Repair (PAR) offers a significant opportunity to improve long-term cardiovascular health for patients at risk. Understanding the success rates, influencing factors, and potential impact on quality of life is crucial for informed decision-making. Long-term follow-up studies are essential to evaluate the lasting benefits of this procedure.
Long-Term Success Rates
The success of PAR hinges on meticulous surgical technique and careful patient selection. Success rates are often measured by the absence of recurrent stenosis (narrowing of the artery) and the prevention of adverse events like myocardial infarction (heart attack). Studies have shown promising long-term results, with significant reductions in the risk of future cardiac events.
Factors Influencing Long-Term Outcomes
Several factors contribute to the long-term success of PAR. Patient adherence to post-operative lifestyle modifications, including diet, exercise, and smoking cessation, plays a pivotal role. The extent of pre-existing cardiovascular disease and the specific anatomical characteristics of the affected artery also influence the outcome. For example, a patient with a history of hypertension and diabetes may require more intensive post-operative management to maintain optimal long-term results.
Moreover, the surgeon’s expertise and experience can also significantly impact the long-term outcome.
Comparison with Other Treatment Options
PAR is often compared to medical therapies like medications and lifestyle changes. While these approaches can be effective in managing risk factors, PAR aims to directly address the underlying structural problem, potentially leading to better long-term outcomes, especially in patients with severe or complex arterial disease. For example, a patient with significant atherosclerosis might experience greater long-term benefit from PAR than from medical therapy alone.
However, each treatment option has its own set of potential benefits and risks, and the optimal choice depends on the individual patient’s circumstances.
Improved Quality of Life
PAR can significantly enhance the quality of life for patients by reducing the risk of future cardiac events. This translates to increased physical activity levels, reduced limitations in daily life, and a greater sense of well-being. For instance, a patient previously limited by angina (chest pain) might experience a substantial improvement in their ability to participate in physical activities, leading to a more fulfilling life.
Long-Term Functional Capacity and Mortality Rates
Data from various studies reveal a correlation between PAR and improved long-term functional capacity. Patients often report an increased ability to perform daily activities without experiencing significant limitations. Furthermore, long-term mortality rates tend to be lower in patients who undergo PAR compared to those managed with medical therapy alone, especially in those with high-risk factors. For instance, a meta-analysis of multiple studies may show a significant reduction in mortality within a 5-10 year follow-up period.
Comparison with Other Treatment Options
Preventive Artery Repair (PAR) is a significant advancement in cardiovascular care, but it’s crucial to understand how it stacks up against other strategies for preventing future heart attacks. This comparison will explore lifestyle modifications, medication, angioplasty, and PAR, evaluating their efficacy, safety, and cost-effectiveness.Understanding the strengths and weaknesses of each approach helps patients and healthcare providers make informed decisions about the best course of action for their individual needs.
Ultimately, the optimal strategy often involves a combination of approaches tailored to the specific risk profile of the patient.
Lifestyle Modifications
Lifestyle modifications play a pivotal role in preventing future heart attacks. These modifications encompass dietary changes, exercise regimens, and stress management techniques. A balanced diet low in saturated and trans fats, rich in fruits, vegetables, and whole grains, combined with regular physical activity, can significantly reduce the risk factors associated with heart disease. Stress reduction techniques, such as meditation or yoga, can also contribute to overall cardiovascular health.
Medication
Pharmacological interventions are crucial in managing risk factors and preventing future heart attacks. Medications like statins, blood pressure-lowering drugs, and antiplatelet agents can effectively control cholesterol levels, lower blood pressure, and reduce the risk of blood clots, thereby mitigating the likelihood of future cardiac events. Specific medication choices are tailored to individual patient needs and risk profiles. For example, patients with high cholesterol might be prescribed statins, while those with hypertension might be given blood pressure-lowering medications.
Angioplasty
Angioplasty, a minimally invasive procedure, involves inserting a catheter with a balloon to open narrowed or blocked arteries. This procedure is often used to address existing coronary artery disease. While it can alleviate immediate symptoms and improve blood flow, it doesn’t necessarily address the underlying causes of the blockage, potentially leading to recurrence. Angioplasty is a viable treatment option for acute situations but may not be as effective for preventing future heart attacks as a long-term strategy compared to PAR.
Comparison Table
| Treatment | Efficacy | Safety | Cost |
|---|---|---|---|
| Lifestyle Modifications | High, but often gradual improvements | Excellent, minimal risks | Low |
| Medication | High, but requires long-term adherence | Generally good, but potential side effects | Moderate to High (depending on the medication) |
| Angioplasty | Effective for immediate relief | Generally safe, but potential complications | High |
| PAR | High, addressing the root cause | Generally safe, but potential complications | High (initial cost) |
Cost-Effectiveness Analysis
The cost-effectiveness of PAR needs careful consideration. While the initial cost of PAR may be higher than other treatments, long-term savings can be realized by reducing the need for future procedures, hospitalizations, and lost productivity due to heart attacks. Factors like the patient’s overall health, the severity of the underlying condition, and potential complications will influence the long-term cost-effectiveness of PAR.
Conclusion
The choice between PAR and other treatment options depends on individual circumstances. Lifestyle modifications and medication are fundamental preventive strategies, often providing a strong foundation. Angioplasty addresses existing blockages, but PAR aims to prevent future problems by addressing the root cause. A comprehensive evaluation by a healthcare professional, considering the patient’s specific risk factors, is essential for determining the most suitable approach.
Wrap-Up
In conclusion, preventive artery repair, while a significant surgical intervention, can offer substantial long-term benefits for patients who’ve experienced heart attacks. Careful consideration of patient selection, surgical techniques, and post-operative care is crucial to maximizing success rates and minimizing risks. By understanding the procedure’s potential complications and comparing it to alternative treatments, patients can make informed decisions about their care.
The ultimate goal is to optimize cardiovascular health and enhance quality of life, and PAR is a crucial tool in achieving this.