Hundreds of medical procedures deemed unnecessary are raising serious concerns about healthcare practices. From unnecessary diagnostic tests to potentially harmful surgical interventions, the prevalence of these procedures highlights a crucial need for change. This isn’t just about wasted resources; it’s about patient safety, well-being, and the trust we place in our healthcare providers. The potential harm, both physical and emotional, is substantial.
This exploration delves into the reasons behind these procedures, their financial impact, and potential solutions for a more efficient and ethical healthcare system.
The issue extends beyond individual procedures to encompass broader systemic factors. From over-testing to a lack of preventative care, a range of issues contribute to the current problem. This analysis will present various categories of unnecessary procedures, examining their rationale, potential harm, and potential alternatives.
Introduction to the Issue of Unnecessary Medical Procedures
The practice of performing unnecessary medical procedures is a significant concern in healthcare systems worldwide. This phenomenon, often driven by factors beyond patient need, results in substantial costs, potential harm to patients, and a misallocation of valuable resources. The consequences of unnecessary procedures extend far beyond the immediate patient experience, impacting the entire healthcare landscape.Performing unnecessary procedures exposes patients to risks such as complications from surgery, adverse reactions to medications, and increased likelihood of infections.
These complications can lead to prolonged hospital stays, increased medical expenses, and diminished quality of life. Furthermore, the financial burden of unnecessary procedures places a strain on healthcare systems, potentially diverting funds from essential services and impacting access to care for those who truly need it.
Factors Contributing to the Prevalence of Unnecessary Procedures
Several factors contribute to the high prevalence of unnecessary medical procedures. These include physician incentives, pressure to maintain high volume, patient expectations, and inadequate oversight. In some cases, patients may demand procedures based on fear or misinformation, while physicians might feel pressured to perform procedures to maintain a high volume of activity, which can be tied to their professional reputation or financial incentives.
Insufficient oversight and lack of standardization in protocols also play a role in the problem.
Examples of Specific Medical Procedures Frequently Deemed Unnecessary
Numerous medical procedures are frequently questioned for their necessity. These procedures may include unnecessary diagnostic tests, such as certain imaging scans performed for minor complaints, and elective surgeries for conditions that may resolve naturally or respond well to less invasive interventions.
Table Outlining Categories of Unnecessary Medical Procedures
| Category | Examples | Rationale for Unnecessary Procedure | Potential Harm |
|---|---|---|---|
| Diagnostic Tests | Repeat blood tests for minor ailments, unnecessary imaging scans (e.g., X-rays for back pain with no fracture), genetic testing for conditions with low probability. | Often driven by physician or patient anxieties, lack of clear diagnostic criteria, or the pressure to identify a cause. | Exposure to radiation, unnecessary discomfort, potential for false positives leading to further, unnecessary procedures, and increased costs. |
| Surgical Interventions | Cosmetic surgeries for minor imperfections, unnecessary joint replacements, elective hernia repairs for asymptomatic hernias. | Driven by patient desire for improvement, social pressures, or a perceived need for a quick fix, rather than addressing the root causes. | Increased risk of complications from surgery, such as infection, bleeding, or nerve damage, prolonged recovery, and potential for long-term pain or disability. |
| Pharmaceutical Treatments | Prescription medications for conditions not requiring treatment, or using stronger medications than necessary. | Often based on anecdotal evidence or pressure to treat symptoms, rather than a thorough assessment of the patient’s overall health. | Adverse drug reactions, drug interactions, development of resistance to medications, and potential for masking underlying conditions. |
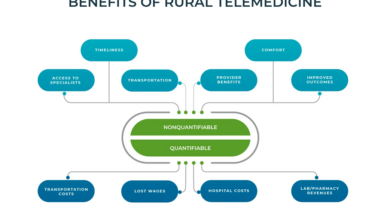
Economic Impact

Unnecessary medical procedures impose a significant financial burden on healthcare systems, patients, and families. The costs associated with these procedures extend far beyond the immediate expense, impacting resource allocation and potentially hindering access to essential, evidence-based care. The financial strain underscores the critical need for preventative measures and judicious utilization of medical interventions.
Financial Burden on Healthcare Systems
The escalating costs of unnecessary medical procedures strain healthcare budgets at all levels. These procedures often involve substantial use of resources like personnel, equipment, and facilities. Reduced funds available for preventive care, research, and the treatment of genuine health concerns are the inevitable consequences. For instance, a hospital performing numerous unnecessary procedures might find its ability to invest in advanced diagnostic equipment or staff training diminished.
This in turn impacts the quality of care available to patients requiring complex or specialized treatments.
It’s shocking to consider how many medical procedures are deemed unnecessary. This raises important questions about cost-effectiveness and patient well-being. For example, the recent “soul of diabetes talk” ( soul of diabetes talk ) highlighted the importance of preventative care and holistic approaches to managing the disease, which could potentially reduce the need for some procedures down the line.
Ultimately, a focus on preventative care and patient empowerment can help us reduce the number of unnecessary medical interventions.
Financial Ramifications on Patients and Families
Beyond the healthcare system, unnecessary procedures impose a substantial financial burden on patients and their families. These expenses encompass not only the direct costs of the procedure itself, including anesthesia, medications, and hospital stays, but also indirect costs such as lost wages, childcare expenses, and travel costs. For example, a patient undergoing an unnecessary surgical procedure might experience a significant loss of income while recovering, placing a financial strain on their household budget.
The emotional toll on families due to these unnecessary expenses can also be substantial.
Potential Savings Achievable by Reducing Unnecessary Procedures
Significant savings are potentially achievable through the reduction of unnecessary medical procedures. By implementing strategies that identify and mitigate unwarranted interventions, healthcare systems can redirect resources towards more effective and cost-effective care. These savings could be reinvested in preventive care programs, expanding access to quality healthcare services, or improving the infrastructure of the healthcare system.
It’s fascinating how many medical procedures are now questioned for their necessity. The recent scrutiny of unnecessary treatments highlights the importance of informed decisions, like whether or not you should get tested for vitamin D. A recent study suggests that routine vitamin D testing might not always be beneficial, and you can explore the pros and cons of testing further in this informative article: should you get tested for vitamin d.
Ultimately, this all points back to the broader issue of unnecessary procedures and the need for a more cautious and personalized approach to healthcare.
Comparison of Costs: Unnecessary vs. Necessary Procedures
The cost of unnecessary procedures often far outweighs the cost of preventive care. Preventive care, focused on early detection and health promotion, aims to avoid the need for costly interventions in the long run. For instance, regular screenings for conditions like hypertension or diabetes can prevent the need for expensive treatments later on. A preventative approach often yields long-term savings for both individuals and the healthcare system.
Cost Comparison Table
| Type of Procedure | Cost (USD) | Justification | Alternative |
|---|---|---|---|
| Unnecessary Knee Arthroscopy | $10,000 | Patient presented with minor, self-limiting knee pain, not justifying surgery. | Physical therapy, pain management |
| Unnecessary Cardiac Catheterization | $15,000 | Patient presented with stable angina, not requiring invasive procedure. | Pharmacological management, lifestyle modifications |
| Necessary Coronary Artery Bypass Graft (CABG) | $100,000 | Patient presented with significant coronary artery disease, requiring surgical intervention. | N/A |
| Necessary Colonoscopy | $1,000 | Patient presented with high risk of colon cancer. | N/A |
Patient Safety and Well-being
Unnecessary medical procedures, while seemingly innocuous, pose significant risks to patient safety and well-being. The potential for complications, adverse effects, and eroded trust in healthcare providers is substantial. Furthermore, these procedures can disrupt the course of appropriate care, causing emotional distress and hindering positive health outcomes. This section will delve into these multifaceted impacts.
Potential Risks Associated with Unnecessary Procedures
Unnecessary procedures introduce a range of potential risks, from minor inconveniences to serious complications. These risks stem from the inherent invasiveness of many medical procedures, the potential for human error, and the inherent variability in patient responses. Complications can manifest as infections, bleeding, allergic reactions, nerve damage, and even death. For instance, an unnecessary biopsy might lead to a localized infection, while an unnecessary surgery could result in a life-altering complication like blood clots or organ damage.
The cumulative effect of numerous unnecessary procedures across a population can lead to significant health burdens.
Impact on Patient Trust in Healthcare Providers
Patients develop trust in their healthcare providers through consistent care, accurate diagnoses, and transparent communication. Unnecessary procedures, perceived as non-essential or driven by financial incentives rather than patient need, can erode this trust. Patients who undergo unnecessary procedures may question the motives of their providers, potentially leading to a decline in adherence to future medical recommendations. This can hinder effective treatment and contribute to poor health outcomes.
Emotional Distress Caused by Unnecessary Procedures
The experience of unnecessary medical procedures can cause considerable emotional distress for patients. Anxiety, fear, and disappointment are common responses. Patients may feel violated, exploited, or that their autonomy has been disregarded. These emotional responses can have long-term effects on mental well-being, impacting the patient’s overall health and quality of life. Moreover, the emotional burden can lead to increased healthcare utilization and create additional costs for the healthcare system.
Delay or Hindrance of Appropriate Care
Unnecessary procedures can significantly delay or hinder the delivery of appropriate care. Resources, including physician time, hospital beds, and diagnostic tools, are diverted to procedures that do not address the patient’s actual health needs. This delay can impact the timely diagnosis and treatment of genuine medical issues, potentially leading to a worsening of the patient’s condition. Furthermore, unnecessary procedures can lead to a delay in appropriate preventive care, like screenings or vaccinations.
Patient Risks Associated with Different Procedure Categories, Hundreds of medical procedures deemed unnecessary
| Procedure Category | Potential Risks | Severity of Risk | Preventive Measures |
|---|---|---|---|
| Diagnostic Imaging (e.g., unnecessary CT scans) | Radiation exposure, allergic reactions to contrast agents, anxiety, potential for false positives leading to unnecessary further interventions | Moderate to high | Strict adherence to imaging guidelines, clear communication with patients about risks and benefits, use of alternative diagnostic methods where appropriate |
| Surgical Procedures (e.g., elective surgeries) | Infection, bleeding, blood clots, nerve damage, organ damage, prolonged recovery time | High | Thorough pre-operative assessment, informed consent process, adherence to surgical safety protocols, avoiding non-essential surgeries |
| Laboratory Tests (e.g., unnecessary blood tests) | Pain, bruising at the puncture site, potential for infection, anxiety, unnecessary costs | Low to Moderate | Appropriate selection of tests based on clinical indications, minimizing unnecessary procedures |
Quality Improvement Strategies
Reducing unnecessary medical procedures requires a multifaceted approach. Simply put, we need a concerted effort across all levels of the healthcare system. This involves not only identifying the procedures but also implementing effective strategies to prevent their occurrence in the first place. The aim is to ensure that patients receive the most appropriate care based on their individual needs, minimizing risks and maximizing health outcomes.
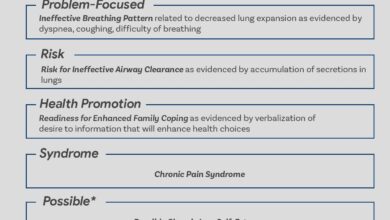
Identifying Unnecessary Procedures
A key element in reducing unnecessary procedures is proactive identification. This process involves a comprehensive review of existing procedures, considering factors such as patient history, clinical findings, and potential alternatives. Healthcare providers must be empowered to question the necessity of a procedure, fostering a culture of critical thinking and evidence-based decision-making.
- Review of Existing Protocols: Regularly reviewing existing clinical protocols and guidelines is crucial. These should be updated based on current research and best practices. For instance, a hospital could review its surgical procedures for appendectomies to ensure they are only performed when absolutely necessary, avoiding unnecessary surgeries.
- Standardized Procedure Criteria: Establishing clear criteria for when a procedure is warranted is vital. This ensures consistent application of guidelines across the board, eliminating ambiguity and reducing the likelihood of unnecessary interventions. For example, clear diagnostic criteria for certain conditions could help prevent unnecessary biopsies or imaging studies.
- Data Analysis: Analyzing procedure rates, patient demographics, and outcomes provides valuable insights into patterns and trends. This data-driven approach can help pinpoint areas where unnecessary procedures are most prevalent. This could involve tracking the frequency of certain procedures in specific age groups or for particular conditions.
Role of Healthcare Providers
Healthcare providers play a critical role in preventing unnecessary procedures. Their commitment to evidence-based practice and critical thinking is essential. Open communication with patients and fostering shared decision-making are vital components. Providers should be empowered to question unnecessary procedures, and be equipped with the knowledge and resources to do so.
- Patient Education and Shared Decision-Making: Transparent communication with patients about the necessity of procedures is paramount. This should involve explaining the potential benefits, risks, and alternatives. Jointly making decisions ensures the patient feels involved and informed, which helps prevent unnecessary interventions. This can involve discussing various treatment options with patients and allowing them to actively participate in their care plan.
- Proactive Questioning: Healthcare providers should routinely question the need for procedures. This includes asking about alternative diagnostic approaches, considering the potential for harm, and seeking consensus among the care team. A provider questioning the need for a particular diagnostic test or a surgical procedure demonstrates a commitment to best practices.
- Continuous Learning: Providers should actively engage in continuous professional development to stay updated on the latest research, guidelines, and best practices. This will enable them to make informed decisions about procedure necessity. For example, attending workshops or seminars on evidence-based medicine or critical care.
Best Practices in Reducing Unnecessary Procedures
Implementing best practices can significantly reduce unnecessary procedures. These practices focus on minimizing harm while maximizing patient benefit. Strategies should be tailored to specific clinical settings and patient populations.
- Pre-Procedure Assessment: Thoroughly evaluating patients before recommending a procedure is crucial. This involves a comprehensive review of medical history, current symptoms, and potential alternatives. A pre-operative assessment could involve a detailed review of a patient’s history, examination of their symptoms, and consideration of alternative treatments before recommending a surgery.
- Multidisciplinary Collaboration: Collaboration among different healthcare professionals is essential for comprehensive patient care. This ensures a coordinated approach, leading to more informed decisions regarding the need for procedures. This could include a team of doctors, nurses, and other specialists working together to determine the best course of action.
- Implementing Decision Support Tools: Using decision support tools can help providers make more informed decisions. These tools can offer evidence-based recommendations for diagnosis and treatment, potentially reducing unnecessary procedures. This could involve the use of algorithms or guidelines that can help determine whether a procedure is truly necessary based on the patient’s specific situation.
Educational Resources for Healthcare Providers
Providing educational resources is crucial for training healthcare providers on best practices. These resources should be readily available and easily accessible. These tools can include online courses, workshops, and guidelines.
- Online Courses: Online courses on evidence-based medicine, critical appraisal, and shared decision-making can equip providers with the necessary knowledge and skills to identify and reduce unnecessary procedures.
- Clinical Guidelines: Access to clear and concise clinical guidelines for various procedures is critical. These guidelines should be readily available and consistently updated.
- Workshops and Seminars: Workshops and seminars focused on specific procedures and their alternatives can provide practical training and enhance the skills of healthcare professionals.
Flowchart for Identifying Unnecessary Procedures
The flowchart below illustrates the process of identifying unnecessary procedures.
Start --> Patient Evaluation --> Review of Medical History --> Review of Diagnostic Tests --> Consider Alternatives --> Consult with Team --> Determine Necessity --> Procedure Recommended? (Yes/No) --> Documentation --> End
Ethical Considerations
The ethical implications of unnecessary medical procedures are profound and multifaceted, extending beyond the immediate patient to encompass the broader healthcare system and society. These procedures, often driven by factors beyond the patient’s best interests, raise critical questions about the allocation of resources, patient autonomy, and the overall responsibility of healthcare providers.
A crucial aspect of ethical practice is to prioritize patient well-being above all else, ensuring that interventions are both necessary and beneficial.
Healthcare providers bear a significant ethical responsibility to uphold the highest standards of care, avoiding interventions that offer little to no tangible benefit. This responsibility necessitates a deep understanding of the potential harms, both physical and psychological, associated with unnecessary procedures. The ethical considerations surrounding these procedures are deeply intertwined with the principles of beneficence, non-maleficence, and patient autonomy.
A commitment to evidence-based practice is essential to navigating these complexities.
Ethical Dilemmas Related to Unnecessary Procedures
Unnecessary procedures can lead to various ethical dilemmas. These dilemmas often arise when the potential benefits of a procedure are questionable, or when the potential risks outweigh the anticipated benefits. Patients may be pressured into procedures due to misinformation or the perception of a need, even when their actual health status does not warrant such intervention. Conflicts can also arise between the provider’s desire to maintain their reputation and the patient’s need for appropriate care.
It’s alarming to think about the hundreds of medical procedures now deemed unnecessary. Modern advancements in healthcare, particularly in areas like diabetes modern management strategies, are changing how we approach various health issues. By focusing on preventative care and proactive lifestyle adjustments, we can often avoid procedures that might be more invasive and costly. This shift in perspective is crucial for optimizing healthcare outcomes and reducing unnecessary procedures, leading to a more efficient and effective healthcare system.
diabetes modern management strategies highlight some key areas in this transformation.
Responsibility of Healthcare Providers
Healthcare providers have a fundamental ethical responsibility to prioritize patient well-being. This obligation necessitates a commitment to evidence-based practice, minimizing harm, and maximizing benefits. Providers must carefully evaluate the necessity of each procedure, considering both the patient’s individual circumstances and the available evidence. Transparency and open communication with patients are paramount to ensure informed consent and address potential concerns.
Ultimately, the provider’s ethical compass should guide them towards interventions that align with the patient’s best interests.
Need for Evidence-Based Guidelines
Evidence-based guidelines are essential in medical practice to mitigate the risk of unnecessary procedures. These guidelines provide standardized criteria for assessing the necessity of interventions, promoting best practices, and ensuring consistency across different healthcare settings. Guidelines must be regularly updated to reflect the latest research findings and advancements in medical knowledge. This ensures that procedures are grounded in current evidence, reducing the potential for unnecessary interventions.
Comparison of Ethical Frameworks
Various ethical frameworks can be applied to analyze the ethical implications of unnecessary medical procedures. Utilitarianism, for example, emphasizes maximizing overall benefit and minimizing harm. Deontology, on the other hand, focuses on adherence to moral duties and principles, irrespective of the consequences. Virtue ethics centers on the character and moral virtues of the healthcare provider. Applying these frameworks helps to identify potential conflicts and guide decision-making towards ethically sound practices.
Ethical Considerations in Various Medical Contexts
| Context | Ethical Principle | Potential Conflict | Resolution |
|---|---|---|---|
| Elective cosmetic procedures | Beneficence, Non-maleficence, Patient Autonomy | Potential for overselling benefits, patient pressure, financial incentives | Clear communication of risks and benefits, evidence-based assessment of need, avoiding unnecessary procedures |
| Diagnostic testing | Beneficence, Non-maleficence, Justice | Pressure to order extensive tests, lack of clinical suspicion | Evidence-based approach to testing, justification of test selection, appropriate use of imaging |
| Treatment for chronic conditions | Beneficence, Non-maleficence, Patient Autonomy | Overuse of aggressive treatments, lack of focus on holistic care | Individualized treatment plans, focus on patient preferences, consideration of alternative therapies |
Examples and Case Studies: Hundreds Of Medical Procedures Deemed Unnecessary
Unnecessary medical procedures pose a significant burden on both patients and healthcare systems. These procedures often result in increased costs, potential harm, and a diminished quality of life. Understanding real-world examples and case studies is crucial to highlighting the need for proactive measures to prevent these procedures. By examining specific instances, we can better identify patterns and implement effective strategies to reduce unnecessary interventions.
Common Examples of Unnecessary Procedures
Unnecessary procedures encompass a wide range of interventions, from minor diagnostic tests to major surgical procedures. A significant portion of these procedures stem from misinterpretations of symptoms, overdiagnosis, or the pursuit of a “better safe than sorry” approach. The sheer volume of these procedures often obscures the individual instances of unnecessary intervention, leading to systemic issues.
- Unnecessary Imaging Studies: Patients experiencing mild back pain might undergo multiple MRI or CT scans without a clear clinical indication. These scans expose patients to potentially harmful radiation and often do not yield clinically significant findings. The cost of these scans is substantial and can lead to a cascade of further, unnecessary tests and procedures.
- Preventive Procedures with Low Benefit: Some preventative procedures, such as prophylactic surgeries, may be performed despite limited evidence of their effectiveness. For instance, the removal of tonsils in children with minor symptoms is a procedure with often questionable long-term benefits, potentially leading to complications.
- Overuse of Antibiotic Prescriptions: Many cases of viral infections are treated with antibiotics, despite antibiotics being ineffective against viruses. This practice contributes to the rise of antibiotic-resistant bacteria, posing a serious threat to public health.
Case Studies: The Impact of Unnecessary Procedures
Examining real-life cases is crucial for understanding the impact of unnecessary procedures. These instances highlight the potential harm and financial burden associated with these interventions.
| Case Study | Description | Impact | Potential Solutions |
|---|---|---|---|
| Case 1: Over-screening for Cancer | A patient with a slightly elevated blood marker underwent multiple biopsies and diagnostic tests, all of which were ultimately negative. | High cost, emotional distress, potential for unnecessary physical harm from biopsies, and reduced trust in the healthcare system. | Develop clear diagnostic criteria and protocols to prevent over-testing. Employ risk stratification tools and shared decision-making with patients. |
| Case 2: Prophylactic Knee Replacement | An older adult with mild osteoarthritis underwent a knee replacement surgery, despite the potential for conservative treatments like physiotherapy and pain management to be more effective and less invasive. | Unnecessary surgery, increased risk of complications (e.g., infection, blood clots), prolonged recovery time, and significant financial burden. | Implement guidelines and protocols to evaluate the appropriateness of knee replacement surgery based on the patient’s individual condition and potential for conservative treatment success. |
| Case 3: Unnecessary Cardiac Procedures | Patients with minor heart conditions undergo invasive cardiac procedures without clear evidence of benefit. | High cost, risk of complications, and potential for patients to experience unnecessary fear and anxiety. | Implement guidelines and protocols to determine the need for invasive cardiac procedures. Promote the use of non-invasive diagnostic tools where appropriate. |
Illustrative Scenarios and Potential Solutions
The following scenarios demonstrate the need for change and highlight potential solutions.
- Scenario 1: A patient presents with mild chest pain. Instead of immediately ordering a cardiac catheterization, a comprehensive history, physical examination, and appropriate blood tests could determine if the pain is related to a non-cardiac cause. This approach minimizes unnecessary procedures and reduces costs.
- Scenario 2: A patient with chronic back pain is given a prescription for strong opioids. Instead of relying solely on medication, a multidisciplinary approach involving physical therapy, lifestyle modifications, and mental health support could offer more effective long-term management. This demonstrates that patient-centered care should involve a holistic approach.
Conclusion
In conclusion, the prevalence of unnecessary medical procedures presents a multifaceted problem with significant consequences for patients, healthcare providers, and the entire healthcare system. From economic burdens to compromised patient safety, the need for reform is clear. Ultimately, a commitment to evidence-based practice, improved communication between providers and patients, and a focus on preventative care are essential steps toward a more efficient and ethical healthcare future.
The discussion surrounding these procedures prompts crucial questions about the future of medical practice and the role of healthcare professionals in ensuring patient well-being.