When alzheimers isnt really alzheimers – When Alzheimer’s isn’t really Alzheimer’s, it opens a complex world of misdiagnosis and potential alternative conditions. Many conditions can mimic the symptoms of Alzheimer’s, leading to incorrect diagnoses and inappropriate treatments. Understanding the nuances of these conditions is crucial, as early and accurate diagnosis is essential for effective management and care. This blog post will explore the various factors that contribute to potential misdiagnosis, from symptom overlap and lifestyle influences to the importance of comprehensive evaluations and tailored treatment plans.
This exploration delves into the critical aspects of differentiating Alzheimer’s from other dementias, highlighting the importance of comprehensive neurological evaluations, and exploring the potential impact of lifestyle and environmental factors. We’ll also examine alternative treatments and the critical role of early detection in managing these conditions effectively.
Misdiagnosis and Differential Diagnoses
Navigating the complexities of cognitive decline often involves a delicate dance between identifying the underlying cause and providing appropriate care. Misdiagnosis of Alzheimer’s disease is unfortunately common, highlighting the critical need for thorough assessments and consideration of alternative diagnoses. This often leads to inappropriate treatments and an unnecessarily prolonged period of uncertainty for both patients and families. Understanding the spectrum of conditions that can mimic Alzheimer’s is essential for accurate diagnosis and effective management.Differentiating Alzheimer’s from other forms of dementia requires a comprehensive approach that goes beyond simply assessing memory loss.
The symptoms of various dementias can overlap, making accurate diagnosis challenging. Thorough neurological evaluations, including cognitive testing, medical history review, and physical examinations, are paramount in identifying the specific cause of cognitive impairment.
Conditions Mimicking Alzheimer’s, When alzheimers isnt really alzheimers
A range of conditions can present with symptoms similar to Alzheimer’s disease, demanding careful consideration during the diagnostic process. These include, but are not limited to: vascular dementia, frontotemporal dementia, Lewy body dementia, and depression.
- Vascular dementia often manifests with abrupt onset and step-wise cognitive decline, frequently following a stroke or other vascular event. Memory problems may be less prominent than executive function deficits, such as difficulty with planning or problem-solving. The presence of focal neurological deficits, like weakness or numbness, can be a clue towards vascular involvement. Distinguishing it from Alzheimer’s hinges on identifying the vascular history and presence of stroke-related markers.
- Frontotemporal dementia is characterized by early-onset personality and behavioral changes. These may include apathy, disinhibition, or compulsive behaviors. Language difficulties and problems with executive functions are also common. Memory loss, while present, is often less pronounced than in Alzheimer’s. This form of dementia typically affects the frontal and temporal lobes of the brain, leading to the characteristic behavioral and language symptoms.
- Lewy body dementia presents with a unique combination of fluctuating cognitive abilities, visual hallucinations, and parkinsonian motor symptoms. Cognitive fluctuations can range from periods of clarity to significant confusion. The presence of these additional symptoms, along with sleep disturbances, can help differentiate it from Alzheimer’s.
- Depression can mimic cognitive decline, causing symptoms such as memory problems, difficulty concentrating, and apathy. While these symptoms overlap with dementia, a thorough psychiatric evaluation is crucial. Distinguishing depression from dementia relies on assessing the presence of other mood symptoms, such as sadness, loss of interest, and sleep disturbances.
Importance of Comprehensive Neurological Evaluations
A comprehensive neurological evaluation is crucial for accurately diagnosing the underlying cause of cognitive impairment. This process involves a multifaceted approach:
- Detailed medical history, including past medical conditions, medications, and family history of dementia, is gathered.
- Cognitive testing, using standardized assessments, evaluates memory, language, problem-solving skills, and other cognitive domains.
- Physical examination assesses for neurological deficits, such as muscle weakness, tremors, or abnormal reflexes.
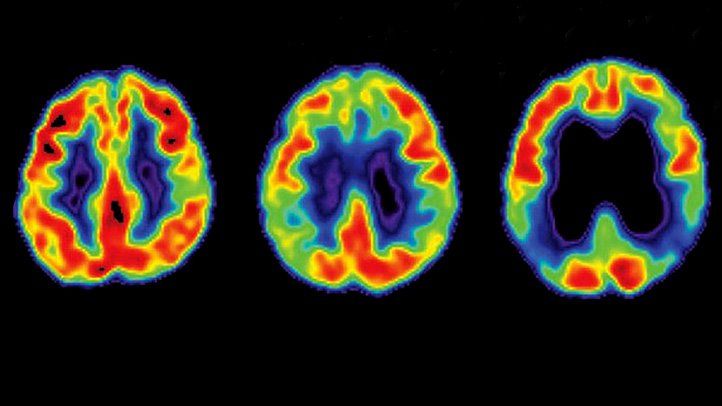
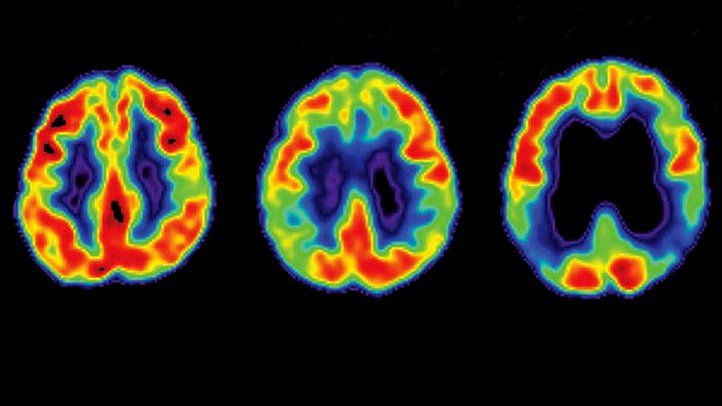
- Neuroimaging techniques, such as MRI or CT scans, help identify structural brain abnormalities that may suggest other conditions.
- Neuropsychological testing further investigates the specific cognitive strengths and weaknesses.
Ruling Out Other Potential Causes
A thorough assessment involves systematically ruling out other potential causes of cognitive decline. This includes:
- Vascular dementia: Evaluating past medical history for stroke, high blood pressure, or other vascular risk factors.
- Frontotemporal dementia: Examining for language or personality changes that may indicate frontal lobe involvement.
- Lewy body dementia: Evaluating for parkinsonian symptoms, visual hallucinations, and fluctuating cognitive abilities.
- Depression: Assessing for mood symptoms, sleep disturbances, and other emotional indicators.
- Medication side effects: Reviewing current medications and potential interactions.
Misdiagnosis Examples
Unfortunately, misdiagnosis of Alzheimer’s can lead to inappropriate treatments and ineffective interventions. A patient with vascular dementia, for instance, might receive medications primarily designed for Alzheimer’s, with little to no improvement in their condition. Early and accurate diagnosis is critical for appropriate management.
Comparison Table
| Feature | Alzheimer’s | Vascular Dementia | Frontotemporal Dementia | Lewy Body Dementia |
|---|---|---|---|---|
| Memory Loss | Early-onset, progressive | Often abrupt onset, step-wise decline | Often less prominent, overshadowed by language/personality changes | Fluctuating cognition |
| Other Symptoms | Language problems, visuospatial difficulties, executive dysfunction | Focal neurological deficits, e.g., weakness, numbness, balance problems | Behavioral changes (e.g., apathy, disinhibition), language impairment | Parkinsonian motor symptoms, visual hallucinations, fluctuating cognition |
Symptom Overlap and Variations
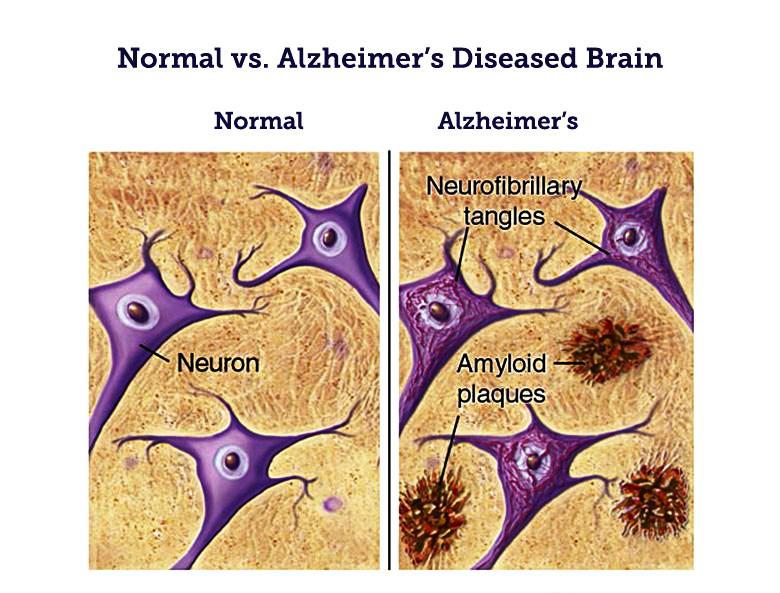
The intricate tapestry of human health often reveals overlapping symptoms across various conditions. Alzheimer’s disease, while possessing distinctive characteristics, can exhibit symptoms that mimic other neurological disorders, making accurate diagnosis a complex process. Understanding these overlaps and variations in symptom presentation is crucial for early detection and appropriate treatment. This is vital for ensuring individuals receive the care tailored to their specific needs and underlying condition.Symptom presentation in Alzheimer’s disease can vary significantly from person to person.
Factors such as the specific genetic predisposition, the rate of disease progression, and co-existing medical conditions all influence the outward manifestation of symptoms. Recognizing these variations is key to differentiating Alzheimer’s from other forms of cognitive decline. It’s also important to note that lifestyle factors, such as diet and exercise, can impact the trajectory of cognitive function, and these must be considered alongside other possible causes.
Symptom Overlap with Other Conditions
Numerous conditions can produce symptoms that mimic those of Alzheimer’s. Vascular dementia, frontotemporal dementia, and Lewy body dementia are among the most frequently considered possibilities. Symptoms like memory loss, confusion, and difficulty with language can appear in several conditions, requiring careful clinical assessment to distinguish between them. Furthermore, depression, anxiety, and certain medication side effects can also produce cognitive symptoms that mimic those seen in Alzheimer’s.
Variations in Symptom Presentation
Individuals with Alzheimer’s experience a range of symptom presentations. Some individuals might initially exhibit more pronounced memory problems, while others may show early signs of language difficulties or changes in personality. These variations highlight the complexity of the disease and underscore the need for a comprehensive evaluation of each patient’s specific presentation.
Importance of Patient History and Lifestyle Factors
A thorough patient history, encompassing details about past medical conditions, family history, lifestyle habits, and social support systems, is crucial in the diagnostic process. Factors like a history of head trauma, exposure to toxins, and the presence of sleep disorders can all influence cognitive function and must be considered. Lifestyle choices, such as diet, exercise, and engagement in social activities, also play a significant role in the trajectory of cognitive decline.
Impact of Co-occurring Medical Conditions
The presence of other medical conditions, such as diabetes, high blood pressure, and cardiovascular disease, can significantly impact cognitive function. These conditions can contribute to inflammation and vascular changes, potentially exacerbating cognitive decline. Moreover, the management of these co-occurring conditions plays a crucial role in preserving cognitive health.
Stages of Cognitive Decline and Symptom Overlap
| Stage | Key Characteristics | Potential Symptom Overlap | Distinguishing Features |
|---|---|---|---|
| Mild Cognitive Impairment (MCI) | Slight but noticeable decline in memory and other cognitive functions, yet daily life is not significantly impacted. | Can overlap with normal age-related cognitive changes, depression, or stress. | Careful assessment of cognitive performance compared to previous baseline. Consideration of the impact of lifestyle factors. |
| Early-Stage Alzheimer’s | Progressive decline in memory, language, and other cognitive functions. Challenges in daily tasks begin to emerge. | May mimic vascular dementia, frontotemporal dementia, or depression. Careful evaluation of symptom progression is key. | Progressive decline over time, impacting daily tasks and activities. Neuropsychological testing can help distinguish it from other conditions. |
| Moderate-Stage Alzheimer’s | Significant decline in cognitive abilities. Individuals require assistance with daily activities, such as dressing and eating. | Overlap with other dementia types can be more pronounced. Careful evaluation of the impact of medications or other medical conditions is important. | Increased dependence on others for daily care. Disturbances in sleep patterns and behaviors can be observed. |
| Late-Stage Alzheimer’s | Severe cognitive impairment. Individuals lose the ability to communicate effectively, recognize loved ones, and perform basic self-care tasks. | The overlap with other conditions may become less significant as the dementia progresses. Physical health issues may dominate. | Complete dependence on caregivers for all aspects of daily life. Loss of communication skills and recognition of loved ones. |
Role of Lifestyle and Environmental Factors
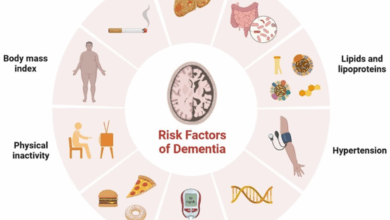
Understanding cognitive decline isn’t just about genetics. Lifestyle choices and environmental exposures play a significant role in shaping brain health, sometimes even masking or mimicking Alzheimer’s symptoms. This influence can be subtle, yet powerful, and it’s crucial to consider these factors when evaluating cognitive impairment. By examining diet, exercise, sleep, environmental toxins, infections, and the interplay with genetics, we gain a broader perspective on cognitive decline.
Lifestyle Factors and Cognitive Health
Lifestyle factors like diet, exercise, and sleep significantly impact cognitive health. A balanced diet rich in fruits, vegetables, and omega-3 fatty acids supports brain function. Regular physical activity promotes blood flow to the brain, fostering neuronal connections and potentially reducing the risk of cognitive decline. Adequate sleep is essential for memory consolidation and overall brain health. Sleep deprivation can impair cognitive function, impacting attention, concentration, and memory.
Environmental Exposures and Cognitive Function
Environmental exposures, such as exposure to heavy metals, pesticides, and air pollution, can negatively affect cognitive function. Similarly, certain infections, such as Lyme disease or HIV, have been linked to cognitive impairment. Chronic exposure to these harmful substances can potentially accumulate in the body, damaging brain cells and disrupting normal cognitive processes. The impact of these exposures can vary depending on individual susceptibility and the duration and intensity of the exposure.
Genetic Predisposition and Environmental Interactions
Genetic predisposition interacts with environmental factors to influence cognitive decline. Individuals with a genetic vulnerability to cognitive impairment may be more susceptible to the negative effects of environmental toxins or infections. For example, a person with a family history of Alzheimer’s may experience more pronounced cognitive decline if exposed to high levels of air pollution. This interaction highlights the complexity of cognitive decline and the importance of considering both genetic and environmental factors.
Sometimes, what looks like Alzheimer’s isn’t actually Alzheimer’s. It can be tricky to pinpoint the root cause, especially when considering other factors like a breast cancer survivor’s experience with the breast cancer survivor and covid vaccine and its potential long-term effects. It’s crucial to rule out other possibilities before jumping to conclusions about the diagnosis of Alzheimer’s.
Further investigation is key in such situations.
Prevalence of Cognitive Decline and Potential Environmental Factors
The prevalence of cognitive decline varies across different populations. Studies suggest that populations with higher exposure to environmental toxins, such as air pollution or certain industrial chemicals, may experience a higher rate of cognitive decline. Socioeconomic factors, access to healthcare, and educational opportunities can also play a role. For instance, populations with limited access to nutritious food or regular exercise might exhibit higher rates of cognitive impairment.
Sometimes, what seems like Alzheimer’s isn’t actually Alzheimer’s. It’s crucial to rule out other potential causes, like exposure to toxins. For example, the dangers of secondhand smoke in apartments and condominiums can mimic Alzheimer’s symptoms. This article highlights the serious health risks, which can impact cognitive function and lead to confusion, memory loss, and other concerning symptoms.
Understanding these factors is vital when considering potential diagnoses for cognitive decline.
Impact of Lifestyle Choices on Cognitive Function
| Lifestyle Choice | Potential Impact on Cognitive Function |
|---|---|
| Balanced Diet (Fruits, Vegetables, Omega-3s) | Improved memory, focus, and overall brain health |
| Regular Exercise | Enhanced blood flow, improved memory and cognitive function, potentially reducing risk of cognitive decline |
| Adequate Sleep | Essential for memory consolidation, improves attention and concentration |
| Reduced Exposure to Toxins | Minimizes damage to brain cells, potentially preserving cognitive function |
| Stress Management | Reduces risk of cognitive decline by promoting overall well-being |
Medical and Psychological Treatments: When Alzheimers Isnt Really Alzheimers
Navigating cognitive decline, especially when a definitive diagnosis like Alzheimer’s isn’t present, requires a multifaceted approach. Medical treatments often focus on managing symptoms and slowing potential progression, while psychological support is crucial for both the individual and their loved ones. This exploration delves into various treatment options, highlighting their potential benefits and risks, as well as the importance of individualized care plans.While there’s no cure for conditions mimicking Alzheimer’s, a range of treatments can help manage symptoms and improve quality of life.
These approaches vary significantly depending on the underlying cause of cognitive decline, emphasizing the need for accurate diagnosis. Effective treatment strategies often involve a combination of medical interventions and psychological support.
Alternative Medical Treatments for Cognitive Decline
Many individuals explore alternative therapies for cognitive decline, often seeking natural remedies and holistic approaches. These treatments can range from dietary supplements to specific exercises. It’s important to note that the scientific evidence supporting the efficacy of many alternative treatments is limited or nonexistent. It’s crucial to discuss any such therapies with a healthcare provider before starting them.
- Dietary Supplements: Some individuals use dietary supplements, such as omega-3 fatty acids, vitamin E, or ginkgo biloba, hoping to improve cognitive function. However, the effectiveness of these supplements in treating cognitive decline remains largely inconclusive. Potential benefits, if any, are often modest and may not outweigh the risks associated with prolonged use.
- Mindfulness and Meditation Practices: Practices like mindfulness and meditation have shown promise in improving focus and reducing stress. These practices may indirectly benefit cognitive function by promoting mental well-being and stress reduction, but more rigorous research is needed to determine their direct impact on cognitive decline.
- Herbal Remedies: Herbal remedies are often promoted for their potential cognitive benefits, but their safety and efficacy are often not well-established. The interaction of herbal remedies with prescription medications is another critical concern, and proper medical supervision is paramount.
Comparison of Therapies for Mimicking Conditions
Different conditions mimicking Alzheimer’s may respond differently to various therapies. For example, vascular dementia, a condition resulting from impaired blood flow to the brain, may benefit from treatments focusing on improving vascular health. Similarly, treatments for Lewy body dementia may focus on managing specific motor and cognitive symptoms.
| Condition | Potential Therapies | Considerations |
|---|---|---|
| Vascular Dementia | Blood pressure management, statins, and lifestyle modifications to improve vascular health. | Requires close monitoring of blood pressure and other cardiovascular factors. |
| Lewy Body Dementia | Cholinesterase inhibitors and antipsychotic medications (carefully prescribed). | Patients may be sensitive to antipsychotics, requiring careful monitoring. |
| Frontotemporal Dementia | Behavioral therapies and medications to manage behavioral and personality changes. | Focus on supporting caregivers and providing accommodations. |
Role of Psychological Support and Counseling
Cognitive decline significantly impacts individuals and their families. Psychological support and counseling play a vital role in navigating the emotional and practical challenges associated with these conditions. This support encompasses individual therapy for the affected person, as well as family counseling to address the needs of caregivers.
Counseling can provide strategies for coping with changes in behavior, memory, and communication. It also helps families navigate the practical challenges of caregiving, including financial planning and legal considerations.
Latest Research on Potential Treatments
Ongoing research explores various avenues for treating conditions mimicking Alzheimer’s. These include studies examining the role of inflammation, neuroprotective therapies, and genetic factors in the progression of these conditions. New therapeutic targets are emerging, but widespread application is still some time away.
Importance of Individualized Treatment Plans
Recognizing the diversity of conditions and individual responses is critical. Treatment plans should be tailored to the specific needs of each patient. This approach encompasses considering the underlying cause, the severity of symptoms, and the patient’s overall health status.
Early Detection and Prevention Strategies
Catching cognitive decline early is crucial, as interventions are most effective when implemented proactively. Early detection allows for timely diagnosis, enabling personalized treatment plans and lifestyle adjustments to slow or halt the progression of the underlying condition. Prevention strategies, focusing on modifiable risk factors, are vital in reducing the overall risk of developing conditions mimicking Alzheimer’s. This proactive approach prioritizes maintaining optimal brain health throughout life.
Importance of Early Detection
Early detection of cognitive decline is paramount in managing conditions that mimic Alzheimer’s. Prompt diagnosis enables timely intervention, potentially slowing or halting the progression of the disease. Early interventions can focus on addressing the specific underlying cause, such as vitamin deficiencies, medication side effects, or other treatable medical issues. Furthermore, early detection allows for the implementation of lifestyle modifications and support systems to improve quality of life.
Preventative Measures and Lifestyle Interventions
Numerous lifestyle factors significantly impact cognitive health. A balanced diet rich in fruits, vegetables, and antioxidants is essential. Regular physical activity, both aerobic and strength training, promotes blood flow to the brain and enhances cognitive function. Social engagement and mental stimulation through activities like puzzles, reading, and learning new skills contribute to maintaining cognitive reserve. Adequate sleep is crucial for memory consolidation and overall brain health.
Controlling cardiovascular risk factors, such as high blood pressure and cholesterol, also plays a key role in protecting brain health. Quitting smoking and limiting alcohol consumption are also beneficial. These lifestyle adjustments can mitigate the risk of cognitive decline and improve overall well-being.
Current Research on Early Detection Biomarkers
Research into early detection biomarkers is actively underway. Scientists are exploring various biological markers, including specific proteins in cerebrospinal fluid or blood, that may indicate an increased risk of cognitive decline. Neuroimaging techniques, such as magnetic resonance imaging (MRI) and positron emission tomography (PET), are also being investigated to identify early structural or functional changes in the brain.
Sometimes, what looks like Alzheimer’s isn’t actually Alzheimer’s. Underlying conditions can mimic the symptoms, making diagnosis tricky. Sadly, similar complexities exist in broader health crises. For instance, in Trump’s first three years, a shocking 2 million Americans lost healthcare and thousands died prematurely , highlighting how systemic issues can drastically impact health outcomes. This underscores the importance of accurate diagnoses and robust healthcare systems to ensure people aren’t just suffering from the symptoms, but receive the right treatment for the actual cause.
Genetic studies are also uncovering potential risk factors, allowing for the identification of individuals at higher risk of developing conditions that mimic Alzheimer’s. Early detection biomarkers will greatly enhance diagnostic accuracy and the potential for early intervention.
Flowchart for Assessing and Managing Potential Misdiagnosis
This flowchart Artikels a systematic approach to assessing and managing potential cases of misdiagnosed Alzheimer’s:
| Step | Action |
|---|---|
| 1 | Gather Comprehensive Medical History |
| 2 | Conduct a Thorough Neurological Examination |
| 3 | Order Relevant Diagnostic Tests (blood tests, neuropsychological assessments, brain imaging) |
| 4 | Consult with Specialists (neurologists, geriatricians, psychiatrists) |
| 5 | Review Existing Medical Records and Medications |
| 6 | Evaluate Lifestyle Factors and Environmental Exposures |
| 7 | Consider Differential Diagnoses and Rule Out Other Conditions |
| 8 | Develop a Personalized Management Plan |
| 9 | Monitor Progress and Adjust as Needed |
This structured approach facilitates a thorough evaluation, ensuring accurate diagnosis and appropriate management of potential misdiagnosis.
Social and Emotional Impact
The journey of navigating a suspected cognitive decline, especially when it’s a misdiagnosis, is profoundly impactful on both the individual and their loved ones. Beyond the medical implications, a complex web of emotional and social challenges emerges, demanding empathy, understanding, and tailored support. The experience can range from anxiety and confusion to profound feelings of isolation and grief.This impact is further amplified when the suspected condition is not the actual one, leading to a period of uncertainty, missed opportunities for appropriate intervention, and potentially harmful interventions.
Addressing these issues requires a multifaceted approach that goes beyond the clinical aspects of the case.
Emotional Challenges Faced by Individuals
Misdiagnosis can lead to feelings of isolation, frustration, and a loss of identity. Individuals may experience a decline in self-esteem as they struggle to adapt to the perceived limitations associated with the condition. Uncertainty about the future and the inability to participate fully in daily life can evoke feelings of fear and anxiety. The emotional distress can also affect their relationships with family and friends.
Emotional Challenges Faced by Families
Families face significant emotional distress during this period. Caregivers often experience high levels of stress, worry, and exhaustion, particularly when facing a misdiagnosis. They may grapple with feelings of helplessness, frustration, and the burden of trying to manage the individual’s needs. The lack of clarity regarding the correct diagnosis adds to the emotional toll, making it difficult for families to adjust to the situation and make informed decisions.
The financial burden associated with investigations and potential treatments can further exacerbate the stress.
Importance of Support Networks and Resources for Caregivers
Caregiver support is crucial in mitigating the emotional and practical challenges faced by families. Structured support groups, educational workshops, and access to mental health professionals can provide caregivers with the tools and resources they need to navigate this challenging period. These resources can offer practical advice, emotional support, and a sense of community. Peer support from other caregivers who have experienced similar situations can be invaluable.
Access to respite care can also reduce the caregiver’s burden and provide much-needed time for self-care.
Impact of Misdiagnosis on Quality of Life
A misdiagnosis can have a profound and lasting impact on the individual’s quality of life. The incorrect diagnosis can lead to inappropriate interventions and treatments that may not address the underlying condition. This delay in receiving the right diagnosis and treatment can result in unnecessary emotional distress, financial burden, and potentially irreversible damage to the individual’s physical and cognitive well-being.
The misdiagnosis can also damage relationships and create unnecessary stress and conflict within the family unit.
Social Stigma Associated with Cognitive Decline
The social stigma surrounding cognitive decline can create significant challenges for individuals and families. This stigma often manifests in the form of prejudice, discrimination, and social isolation. Individuals experiencing cognitive decline may face difficulties in maintaining their social connections and participating in activities that they once enjoyed. Families may also experience social isolation due to the stigma associated with the condition.
These factors can contribute to feelings of shame, embarrassment, and social exclusion. Open conversations and educational initiatives can help reduce the stigma associated with cognitive decline.
Structure for a Support Group for Individuals and Families Facing Potential Misdiagnosis
| Phase | Activities |
|---|---|
| Phase 1: Initial Orientation (First 2-3 Meetings) |
|
| Phase 2: Building a Support System (4-6 Meetings) |
|
| Phase 3: Advocacy and Empowerment (7+ Meetings) |
|
Final Thoughts
In conclusion, the intricate nature of cognitive decline, and the potential for misdiagnosis when it comes to Alzheimer’s, underscores the importance of thorough evaluations and individualized treatment plans. Understanding the overlap of symptoms, the role of lifestyle and environmental factors, and the various potential alternative diagnoses is essential for both patients and healthcare professionals. Early detection, proactive care, and robust support networks are vital for managing these complex conditions effectively and improving the quality of life for those affected.