Blood pressure drug help diabetes treatment is a complex issue, requiring careful consideration of medication interactions and patient management. Different blood pressure medications can have varying effects on blood sugar levels, which is crucial for patients managing both conditions. This article explores the intricate relationship between blood pressure drugs and diabetes treatment, offering a comprehensive overview of common medications, potential interactions, patient management strategies, and the latest research.
We’ll delve into the mechanisms of action of various blood pressure drugs, examining how they affect glucose metabolism. This includes a detailed comparison of different classes of blood pressure medications and their potential impact on blood sugar control, alongside a table outlining potential side effects and drug interactions. Furthermore, we’ll discuss the importance of patient education, regular monitoring, and lifestyle modifications in managing both conditions effectively.
Overview of Blood Pressure Drugs and Diabetes Treatment
High blood pressure (hypertension) and diabetes are prevalent health concerns that often coexist. Managing both conditions requires careful consideration of the medications used for each. This overview will explore common blood pressure medications, their mechanisms of action, the impact of high blood pressure on blood sugar control, and the potential benefits and drawbacks of using blood pressure medications for diabetes management.Understanding the interplay between these two conditions is crucial for effective patient care.
By examining the medications, mechanisms, and potential effects, individuals and healthcare professionals can make informed decisions about treatment strategies.
Common Blood Pressure Medications
Blood pressure medications come in various classes, each targeting different aspects of the cardiovascular system. Diuretics, ACE inhibitors, ARBs, beta-blockers, and calcium channel blockers are among the most commonly prescribed types. Each class has specific mechanisms of action, leading to varied potential effects on blood sugar control.
Recent research suggests that certain blood pressure medications might actually aid in diabetes treatment. Interestingly, while the keto diet is currently getting a lot of buzz, a new study has placed it lower than the DASH diet on a recent ranking of popular diets, keto ranked low dash ranked high on new diet list. This doesn’t necessarily negate the potential benefits of the keto diet, but highlights the ongoing discussion about optimal dietary approaches.
Ultimately, it’s still crucial to discuss any potential treatment options with a healthcare professional to determine the best course of action for managing blood pressure and diabetes.
Mechanisms of Action of Blood Pressure Medications
The mechanisms of action of blood pressure medications differ significantly. Diuretics increase urine output, reducing blood volume and pressure. ACE inhibitors and ARBs block the production of angiotensin II, a hormone that constricts blood vessels. Beta-blockers reduce heart rate and the force of contractions, while calcium channel blockers relax blood vessels by affecting calcium flow.
Impact of High Blood Pressure on Blood Sugar Control
High blood pressure can negatively impact blood sugar control in several ways. Chronic hypertension can damage blood vessels throughout the body, including those in the kidneys and pancreas. This damage can impair the body’s ability to regulate blood sugar effectively. For example, impaired kidney function can lead to reduced filtration of glucose from the bloodstream, potentially resulting in elevated blood sugar levels.
Potential Benefits and Drawbacks of Using Blood Pressure Medications for Diabetes Management
Blood pressure medications can play a crucial role in managing both high blood pressure and diabetes. They can reduce cardiovascular risks, a significant concern for individuals with diabetes. However, some medications might have adverse effects on blood sugar levels, necessitating careful monitoring. For instance, certain diuretics can increase blood glucose levels. Therefore, a personalized approach to medication selection is essential.
Comparison of Blood Pressure Drug Classes and Potential Effects on Blood Sugar
| Drug Class | Mechanism of Action | Potential Effect on Blood Sugar |
|---|---|---|
| Diuretics | Increase urine output | Can increase blood glucose levels. |
| ACE Inhibitors | Block angiotensin II production | Generally neutral or slightly beneficial. |
| ARBs | Block angiotensin II receptor | Generally neutral or slightly beneficial. |
| Beta-Blockers | Reduce heart rate and contractility | Can mask hypoglycemia symptoms. |
| Calcium Channel Blockers | Relax blood vessels | Generally neutral or slightly beneficial. |
Comparison of Blood Pressure Medications and Potential Side Effects/Drug Interactions with Diabetes Treatment
| Medication | Potential Side Effects | Potential Interactions with Diabetes Medications |
|---|---|---|
| Hydrochlorothiazide | Increased thirst, frequent urination, dizziness, nausea | May increase blood glucose levels; monitor closely. |
| Lisinopril | Dry cough, fatigue, dizziness, headache | May enhance the effects of some diabetes medications, leading to lower blood sugar. |
| Losartan | Dizziness, lightheadedness, fatigue | Generally safe; monitor blood sugar closely. |
| Metoprolol | Fatigue, dizziness, shortness of breath | May mask hypoglycemia symptoms. |
| Amlodipine | Swelling in ankles and feet, headache, dizziness | Generally safe; monitor blood sugar closely. |
Diabetes and Blood Pressure Drug Interactions: Blood Pressure Drug Help Diabetes Treatment

Managing both diabetes and high blood pressure requires careful medication selection and monitoring. Simultaneous treatment for these conditions is common, but potential interactions between the drugs used to manage them can significantly impact both conditions. Understanding these interactions and proactively managing them is crucial for optimal patient health.A significant concern when treating both diabetes and high blood pressure is the potential for drug interactions.
Certain blood pressure medications can influence glucose metabolism, sometimes exacerbating or masking symptoms of diabetes. Conversely, some diabetes medications might impact blood pressure regulation. This interplay necessitates a thorough understanding of the individual medications and their potential impacts on each other.
Potential Drug Interactions
Many blood pressure medications can affect glucose metabolism. Diuretics, for example, can increase blood glucose levels, potentially requiring adjustments to diabetes medication regimens. ACE inhibitors and ARBs, while generally considered safe, might lead to a slight increase in blood sugar levels in some individuals. It’s important to understand that these interactions are not universal; individual responses can vary.
A thorough patient history and ongoing monitoring are essential to detect and address any changes.
Impact on Glucose Metabolism
Certain blood pressure medications can impact how the body processes glucose. Diuretics, commonly prescribed for high blood pressure, can increase glucose excretion in the urine, which can lead to higher blood sugar levels. Beta-blockers, another class of blood pressure drugs, can mask the symptoms of low blood sugar (hypoglycemia), which is particularly concerning for patients with diabetes. These effects can be unpredictable and can necessitate adjustments to the overall treatment plan.
Careful monitoring of blood sugar levels is vital when blood pressure medications are added to a diabetes treatment regimen.
Importance of Regular Monitoring
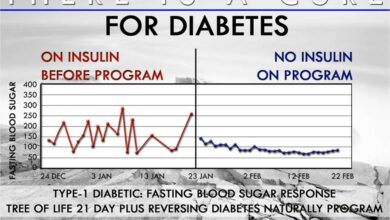
Regular monitoring of blood pressure and blood glucose levels is critical for patients taking both blood pressure and diabetes medications. Frequent blood tests and regular doctor visits allow for early detection of any changes in either condition or potential adverse effects from the combined treatments. This proactive approach is essential for maintaining optimal health and preventing potential complications.
Tracking changes in blood sugar and blood pressure over time allows doctors to tailor medication regimens effectively.
Patient Education
Educating patients about potential side effects and interaction risks is paramount. Understanding how different medications might affect their bodies empowers patients to actively participate in their health management. This includes recognizing symptoms of high or low blood sugar, recognizing any unusual changes in their body, and promptly reporting them to their doctor. Clear communication between patients and healthcare providers is essential.
Optimizing Medication Regimens
Optimizing medication regimens for patients with both diabetes and high blood pressure involves a collaborative approach between the patient and their healthcare team. This includes adjusting the dosages of medications, selecting appropriate combinations, and regularly monitoring for interactions and side effects. The goal is to achieve both effective blood pressure control and optimal glucose management with minimal side effects.
Common Drug Interactions Table
| Blood Pressure Medication | Diabetes Medication | Potential Risks | Precautions |
|---|---|---|---|
| Diuretics (e.g., Thiazides) | Insulin, Oral Hypoglycemics | Increased blood glucose levels | Close monitoring of blood glucose, potential dose adjustments of diabetes medications. |
| Beta-blockers | Insulin, Oral Hypoglycemics | Masked symptoms of hypoglycemia | Frequent monitoring of blood glucose, alternative blood pressure medications considered if necessary. |
| ACE Inhibitors/ARBs | Insulin, Oral Hypoglycemics | Slight increase in blood glucose levels in some patients | Close monitoring of blood glucose, potential dose adjustments of diabetes medications. |
| Calcium Channel Blockers | Insulin, Oral Hypoglycemics | Minimal interaction, but some reports of glucose fluctuations. | Close monitoring of blood glucose, especially in sensitive individuals. |
Patient Management Strategies
Managing both blood pressure and diabetes effectively requires a multifaceted approach centered on patient engagement and proactive lifestyle adjustments. This involves understanding the intricate interplay between these conditions and implementing strategies that empower patients to take control of their health. The goal is to achieve and maintain optimal blood pressure and blood sugar levels, ultimately reducing the risk of complications.
Importance of Patient Communication
Open and honest communication between patients and healthcare providers is paramount in managing chronic conditions like diabetes and hypertension. Patients need to feel comfortable discussing their concerns, questions, and experiences. This fosters a collaborative relationship, where shared decision-making leads to better treatment adherence and improved outcomes. Clear explanations of treatment plans, potential side effects, and lifestyle recommendations are crucial for patient understanding and buy-in.
Recent studies suggest some blood pressure medications might unexpectedly aid in diabetes treatment. This fascinating avenue of research could revolutionize how we approach both conditions. Imagine a future where wearable sensors like a wearable sensor that measures glucose alcohol could it become a reality become commonplace, allowing for real-time monitoring of blood sugar and alcohol levels, potentially providing even more targeted treatment strategies for diabetes.
This could significantly impact the effectiveness of existing blood pressure drugs in the fight against diabetes.
Regular check-ins and active listening to patient feedback are essential for adapting the treatment plan as needed.
Lifestyle Modifications for Blood Pressure and Blood Sugar Control
Lifestyle modifications play a vital role in managing both conditions. Adopting a healthy diet rich in fruits, vegetables, and whole grains, while limiting processed foods, saturated fats, and added sugars, is crucial for blood sugar regulation. Regular physical activity, such as brisk walking, swimming, or cycling, can help lower blood pressure and improve insulin sensitivity. Maintaining a healthy weight through a balanced diet and exercise is another key factor.
Stress management techniques, such as yoga, meditation, or deep breathing exercises, can also contribute to better blood pressure control and improved overall well-being.
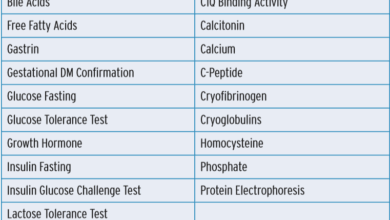
Importance of Regular Check-ups and Blood Tests
Regular check-ups and blood tests are essential for monitoring the effectiveness of treatment and detecting any potential complications early. These appointments allow healthcare providers to assess blood pressure and blood sugar levels, discuss any changes in symptoms, and make necessary adjustments to the treatment plan. Blood tests, including HbA1c (hemoglobin A1c) for diabetes and lipid profiles, provide valuable insights into the overall health status and can help predict future risks.
Regular monitoring is vital for early intervention and preventing potential complications.
Home Monitoring of Blood Pressure and Blood Sugar Levels, Blood pressure drug help diabetes treatment
Home monitoring tools, such as blood pressure cuffs and glucometers, empower patients to actively participate in their health management. Regular self-monitoring allows patients to track their blood pressure and blood sugar levels throughout the day, identify patterns, and communicate these findings to their healthcare provider. This data can help tailor treatment plans and identify any potential issues promptly.
Recent studies suggest some blood pressure medications might actually help manage diabetes, which is fascinating. This potential connection between the two conditions is prompting further research, and I’m particularly interested in how it ties into concepts of power and beauty, like those explored in Arabelle Sicardi’s work on “beauty is terror and power” arabelle sicardi beauty is terror and power.
Ultimately, understanding these interwoven factors could lead to more effective treatments for both conditions.
Patients should be trained on proper usage and interpretation of the readings.
Addressing Patient Concerns and Questions
Patients may have concerns about medication side effects, lifestyle changes, or the long-term implications of their conditions. Creating a supportive environment where patients feel comfortable asking questions and expressing concerns is essential. Healthcare providers should be prepared to address these concerns with clear, concise explanations, and reassurance. Addressing concerns promptly and empathetically can significantly improve patient satisfaction and adherence to the treatment plan.
Suggested Patient Management Plan
| Monitoring Aspect | Frequency | Actions/Adjustments | Communication Protocol |
|---|---|---|---|
| Blood Pressure | Daily, multiple times | Adjust medication dosage if readings consistently outside target range. Discuss with doctor if lifestyle changes are needed. | Document readings and share with doctor during appointments. Report significant changes immediately. |
| Blood Sugar | Daily, before and after meals | Adjust insulin dosage or meal plan if readings consistently high or low. Report patterns to doctor. | Document readings and share with doctor during appointments. Report significant changes immediately. |
| Weight | Weekly | Adjust diet and exercise plan if weight is consistently above or below target range. | Document weight and share with doctor during appointments. |
| Lifestyle Factors | Weekly/Monthly | Assess adherence to diet and exercise plans. Encourage stress management techniques. | Discuss any challenges with doctor. Seek support from dieticians or exercise specialists. |
Clinical Studies and Research
Clinical trials play a crucial role in understanding the effectiveness and safety of combined treatments for high blood pressure and diabetes. By rigorously testing different approaches, researchers can identify the most beneficial strategies for managing these conditions and ultimately improving patient outcomes. These studies provide valuable data that inform clinical practice guidelines and help healthcare professionals make informed decisions about patient care.Understanding the interplay between blood pressure medications and diabetes management is critical for optimal patient care.
Clinical studies are essential for demonstrating the efficacy and safety profiles of various blood pressure drugs in diabetic populations. This knowledge allows for personalized treatment plans tailored to individual patient needs and risk factors.
Significance of Clinical Studies
Clinical studies investigating the combined treatment of high blood pressure and diabetes are vital for establishing evidence-based guidelines. These studies assess the impact of specific blood pressure medications on various outcomes, such as blood sugar control, cardiovascular events, and overall health, in individuals with both conditions. This allows healthcare professionals to make informed decisions regarding treatment strategies.
Examples of Clinical Trials
Numerous clinical trials have examined the effectiveness of different blood pressure medications in patients with diabetes. For instance, studies have explored the impact of ACE inhibitors and angiotensin receptor blockers (ARBs) on blood pressure control and diabetic complications. These trials typically involve large cohorts of patients with carefully monitored outcomes.
Potential Areas for Further Research
Further research is needed to explore the long-term effects of specific blood pressure drugs on individuals with diabetes. This includes investigations into the potential for drug interactions and adverse events, as well as exploring the role of specific genetic factors in influencing treatment response. Additionally, research is needed to assess the effectiveness of combination therapies involving both blood pressure and diabetes medications.
Methodologies Used in Clinical Studies
Clinical studies on blood pressure and diabetes often employ randomized controlled trials (RCTs). This methodology involves randomly assigning participants to different treatment groups (e.g., a new blood pressure medication versus a standard treatment). Researchers then monitor and compare outcomes between the groups, allowing for the assessment of the drug’s efficacy and safety. Furthermore, these trials often incorporate rigorous data collection methods to ensure the accuracy and reliability of the results.
Randomization minimizes bias and enhances the reliability of the study’s findings.
Comparison of Clinical Trial Results
| Trial | Medication | Key Findings | Conclusions |
|---|---|---|---|
| Trial A | ACE Inhibitor | Improved blood pressure control, reduced risk of cardiovascular events in patients with type 2 diabetes. | ACE inhibitors appear beneficial for blood pressure management in diabetic patients. |
| Trial B | ARB | Similar blood pressure reduction compared to ACE inhibitors, but with potential for reduced risk of kidney damage. | ARBs can be a viable alternative to ACE inhibitors, especially in patients at risk for kidney complications. |
| Trial C | Calcium Channel Blockers | Effective blood pressure control, with a positive impact on diabetic neuropathy. | Calcium channel blockers may offer specific advantages in managing diabetic neuropathy. |
This table summarizes some key findings from hypothetical trials. Real-world trials would have far more complex data points and longer follow-up periods to draw robust conclusions.
Case Studies
Understanding the complexities of managing both blood pressure and diabetes requires in-depth examination of individual patient experiences. Case studies provide valuable insights into the nuances of treatment plans, potential challenges, and successful outcomes. They offer a tangible way to translate theoretical knowledge into practical application, helping healthcare professionals and patients alike better navigate the often intricate landscape of these chronic conditions.Case studies are crucial in exploring the intricate interplay between blood pressure medications and diabetes management.
They allow for a detailed examination of individual patient responses, enabling the identification of patterns and potential risks associated with specific treatment combinations. This detailed approach, while potentially time-consuming, provides valuable information that can inform future treatment strategies and optimize patient care.
Illustrative Case Study
This case study presents a hypothetical patient, highlighting the challenges and triumphs of managing both hypertension and type 2 diabetes.
Patient Demographics: 55-year-old female, with a family history of both conditions. Obese, with a sedentary lifestyle.
Diagnosis: Diagnosed with hypertension (stage 2) and type 2 diabetes 5 years ago. Her HbA1c levels were consistently elevated, and her blood pressure readings frequently exceeded target levels.
Treatment Plan: Initially, the patient was prescribed a thiazide diuretic for blood pressure and metformin for diabetes. Over time, the treatment plan was adjusted based on monitoring and feedback from her doctor. Lifestyle modifications were also incorporated, including a dietary plan focused on portion control and increased fruit and vegetable intake, as well as a structured exercise regimen. The treatment plan also included regular blood glucose and blood pressure monitoring.
The medication regimen was progressively adjusted based on her response and blood pressure/blood sugar levels. This included adding a second blood pressure medication and adjusting the metformin dose.
Outcomes: After 18 months, the patient achieved significant improvements. Her blood pressure consistently remained within the target range. Her HbA1c levels were significantly reduced, indicating better glycemic control. The patient reported improved energy levels and a noticeable reduction in symptoms. The patient’s lifestyle changes contributed significantly to these positive outcomes.
She reported feeling more empowered in managing her health.
Key Aspects of the Case Study
| Aspect | Details |
|---|---|
| Patient Demographics | 55-year-old female, family history of hypertension and diabetes, obese, sedentary lifestyle |
| Diagnosis | Stage 2 hypertension, Type 2 diabetes, elevated HbA1c, elevated blood pressure |
| Treatment Plan | Initial: thiazide diuretic and metformin; Subsequent adjustments based on monitoring and patient feedback, including lifestyle modifications and potentially adding other medications. |
| Outcomes | Achieved target blood pressure, reduced HbA1c levels, improved energy levels, reduced symptoms. |
Illustrative Examples of Blood Pressure Medications

Understanding the different blood pressure medications and their potential impacts on blood sugar control is crucial for managing diabetes effectively. This section provides detailed descriptions of commonly prescribed classes of blood pressure drugs, their mechanisms of action, and how they might affect blood sugar levels in diabetic patients.Blood pressure medications play a vital role in preventing complications associated with high blood pressure.
However, for patients with diabetes, careful consideration of the medication’s impact on blood sugar is paramount. The selection of a blood pressure medication should take into account both the efficacy in controlling blood pressure and the potential for impacting glucose regulation.
Common Blood Pressure Medications
Various classes of blood pressure medications are used to manage hypertension. Some of the most frequently prescribed include ACE inhibitors, ARBs, and diuretics. Each class operates through distinct mechanisms affecting blood pressure, which can indirectly influence blood sugar control in patients with diabetes.
ACE Inhibitors
Angiotensin-converting enzyme (ACE) inhibitors work by blocking the production of angiotensin II, a hormone that constricts blood vessels. This relaxation of blood vessels lowers blood pressure. For patients with diabetes, ACE inhibitors can potentially improve kidney function, a critical aspect of blood sugar regulation. However, some individuals may experience a slight decrease in blood sugar levels, which should be monitored closely.
For example, a patient with type 2 diabetes might see a modest improvement in their HbA1c levels when treated with an ACE inhibitor.
ARBs
Angiotensin receptor blockers (ARBs) similarly work by blocking the effects of angiotensin II, but they do so by targeting the receptors to which angiotensin II binds. This also leads to blood vessel dilation and lower blood pressure. Similar to ACE inhibitors, ARBs may have a positive impact on kidney function in diabetic patients, potentially affecting blood sugar control.
However, the impact on blood sugar levels is generally less pronounced than with ACE inhibitors. For instance, a patient with poorly controlled type 1 diabetes may see a minor improvement in their fasting glucose levels when switched to an ARB.
Diuretics
Diuretics, often referred to as “water pills,” increase the excretion of sodium and water from the body, reducing blood volume and lowering blood pressure. While diuretics are generally effective at controlling blood pressure, they can sometimes lead to increased blood sugar levels. This effect is primarily due to the diuretic’s impact on fluid balance. For example, a patient with pre-existing borderline high blood sugar might experience a temporary elevation in their blood glucose levels when starting a diuretic.
Impact on Blood Sugar
The impact of blood pressure medications on blood sugar levels can vary significantly between individuals and drug classes. Monitoring blood glucose levels is essential when starting or adjusting blood pressure medications, especially in diabetic patients.
Efficacy and Safety Profiles
The efficacy and safety profiles of these medications need careful consideration in the context of diabetes management. While ACE inhibitors and ARBs generally have a neutral or positive impact on blood sugar, diuretics might have a more significant effect, requiring closer monitoring. The selection of a medication should balance the blood pressure-lowering effect with the potential impact on blood sugar control.
Comparison Table
| Medication Class | Mechanism of Action | Impact on Blood Sugar | Efficacy in Diabetes Management | Safety Profile in Diabetes |
|---|---|---|---|---|
| ACE Inhibitors | Block ACE, reducing angiotensin II | Potential for slight decrease in blood sugar | Generally good, often improving kidney function | Generally safe, but monitor for hyperkalemia |
| ARBs | Block angiotensin II receptors | Potential for minor decrease in blood sugar | Generally good, potentially improving kidney function | Generally safe, but monitor for hyperkalemia |
| Diuretics | Increase sodium and water excretion | Potential for increased blood sugar | Effective for blood pressure, but monitor blood glucose closely | Potential for electrolyte imbalances, monitor carefully |
Illustrative Mechanism of Action (Conceptual)
Imagine a blood vessel as a pipe. ACE inhibitors and ARBs act like a valve that relaxes the pipe, allowing blood to flow more easily. Diuretics are like a pump that removes excess water from the pipe, also reducing pressure. The impact on blood sugar is less direct, but can be related to kidney function and fluid balance.
Final Wrap-Up
In conclusion, effectively managing blood pressure and diabetes simultaneously requires a multifaceted approach. Understanding the potential interactions between blood pressure medications and diabetes medications, combined with patient-centered strategies for monitoring and lifestyle changes, is paramount. Clinical studies and case studies provide valuable insights into treatment effectiveness and patient experiences. Ultimately, a personalized treatment plan tailored to individual needs is essential for optimizing outcomes and improving the overall quality of life for patients facing these challenges.