Treating diabetes with insulin beta therapies represents a groundbreaking approach to managing this chronic condition. Insulin beta cells are crucial for regulating blood sugar, and their dysfunction lies at the heart of diabetes. This exploration delves into the intricacies of these cells, current treatments, and emerging therapies, promising a future with more effective and personalized solutions for individuals living with diabetes.
From understanding the fundamental role of insulin beta cells in glucose regulation to exploring various insulin therapies and their limitations, this comprehensive overview provides a nuanced perspective on the potential of insulin beta cell therapies. We’ll examine different approaches, their potential benefits, and the challenges associated with this innovative area of research.
Introduction to Insulin Beta Cell Function
Insulin beta cells, nestled within the islets of Langerhans in the pancreas, are the unsung heroes of blood glucose regulation. These specialized cells play a critical role in maintaining a stable blood sugar level, a fundamental aspect of overall health. Their precise function and intricate mechanisms are vital for understanding diabetes and developing effective treatment strategies.Insulin secretion is a tightly controlled process, directly responding to changes in blood glucose levels.
When blood glucose rises after a meal, beta cells detect this increase and initiate a cascade of events leading to insulin release. This intricate dance of cellular signaling ensures that the body efficiently uses glucose for energy, preventing dangerous spikes and crashes.
Insulin Secretion Process
The process of insulin secretion in response to glucose is a fascinating example of cellular communication. Glucose entering the beta cell triggers a series of events. Glucose is metabolized, leading to an increase in ATP levels. This increased ATP closes ATP-sensitive potassium channels, causing membrane depolarization. Depolarization opens voltage-gated calcium channels, allowing calcium influx.
The resulting rise in intracellular calcium concentration stimulates the fusion of insulin-containing vesicles with the cell membrane, releasing insulin into the bloodstream. This carefully orchestrated sequence of events ensures a timely and appropriate insulin response to maintain blood glucose homeostasis.
Insulin Beta Cell Structure and Function
Insulin beta cells are characterized by a unique morphology and specialized organelles crucial for their function. These cells possess numerous mitochondria, reflecting their high energy demands for insulin synthesis and secretion. The presence of abundant rough endoplasmic reticulum and Golgi apparatus indicates the cell’s active role in protein synthesis, including insulin production. Furthermore, the extensive network of microfilaments and microtubules provides the structural support needed for intracellular transport and vesicle trafficking, facilitating the precise release of insulin.
These structural elements, intricately interconnected, contribute to the overall efficiency of insulin secretion.
Treating diabetes with insulin beta is a complex process, and while there are various approaches, recent research highlights the importance of holistic well-being. For example, a recent study, study finds best way to help people with depression lose weight , demonstrates that addressing underlying mental health issues can significantly impact weight management. Ultimately, a multifaceted approach incorporating both physical and mental health strategies is key to effectively managing diabetes with insulin beta.
Healthy vs. Impaired Insulin Beta Cell Function
| Characteristic | Healthy Insulin Beta Cell Function | Impaired Insulin Beta Cell Function |
|---|---|---|
| Glucose Sensitivity | Rapid and appropriate insulin secretion in response to rising glucose levels. | Delayed or inadequate insulin secretion in response to rising glucose levels. May also exhibit exaggerated or inappropriately timed insulin secretion. |
| Insulin Content | Adequate intracellular insulin stores. | Reduced insulin content in the cells. |
| Secretion Efficiency | Efficient fusion of insulin-containing vesicles with the cell membrane, resulting in rapid insulin release. | Reduced or impaired vesicle fusion and insulin release. Possible defects in intracellular trafficking. |
| Cell Viability | Maintaining a healthy cellular structure and function. | Potential for apoptosis (programmed cell death) or reduced cellular function. |
| Cellular Signaling | Appropriate and timely activation of intracellular signaling pathways. | Disruptions in the intracellular signaling cascades leading to insulin secretion. |
Impaired insulin beta cell function is a hallmark of type 2 diabetes. The table above highlights the differences in these crucial aspects between healthy and impaired cells. These discrepancies contribute to the dysregulation of blood glucose homeostasis and the development of diabetes. Understanding these nuances is critical for developing effective therapeutic interventions.
Current Treatments for Diabetes
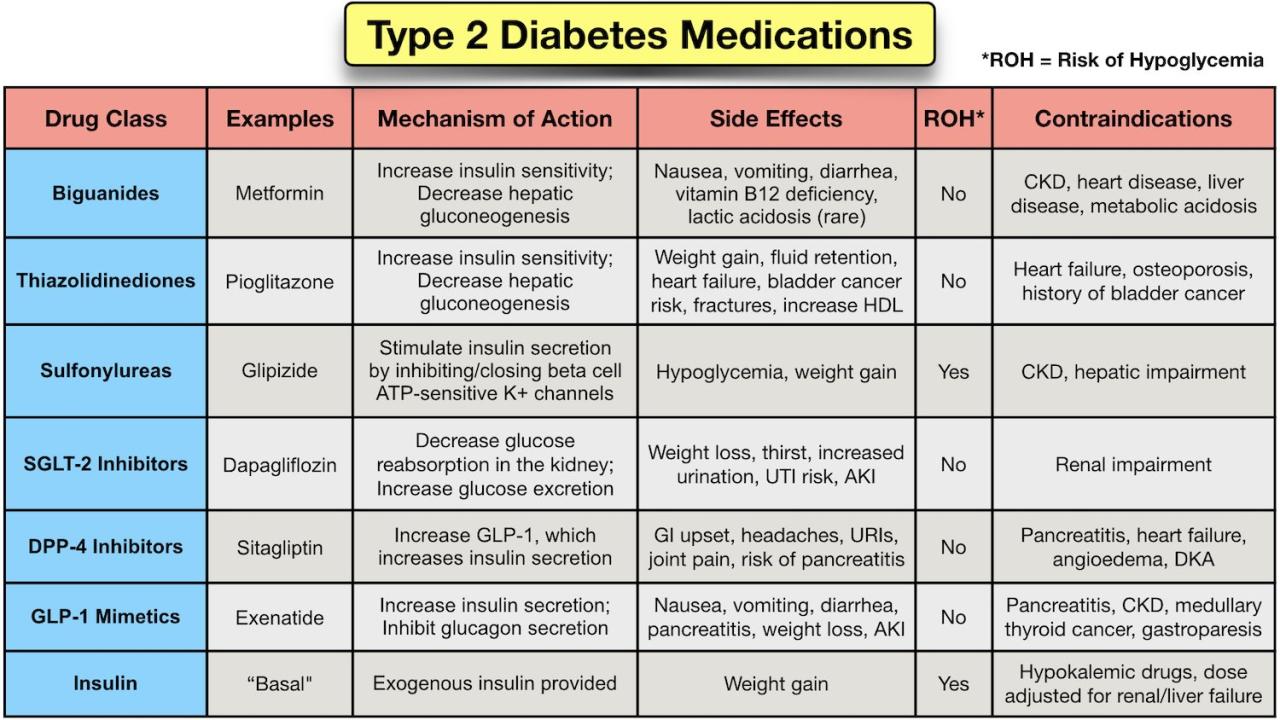
Diabetes, a chronic metabolic disorder, requires ongoing management to control blood glucose levels and prevent complications. Effective treatment strategies encompass lifestyle modifications, oral medications, and, in many cases, insulin therapy. This approach aims to achieve and maintain optimal blood glucose control, reducing the risk of long-term complications associated with diabetes.Current treatments for diabetes primarily focus on regulating blood glucose levels to prevent or delay the onset of serious complications like heart disease, kidney disease, nerve damage, and eye problems.
The chosen treatment strategy is tailored to the individual patient’s needs, considering factors such as the type of diabetes, blood glucose control goals, and potential side effects of different therapies.
Types of Insulin Therapies
Insulin therapies are crucial for managing diabetes, particularly in type 1 diabetes and in some cases of type 2 diabetes. Different types of insulin vary in their onset, peak action, and duration of effect, allowing for personalized regimens to mimic the natural insulin release pattern of a healthy pancreas.Various insulin types are available, each designed to meet specific needs.
Rapid-acting insulins, such as lispro and aspart, are injected shortly before meals to manage postprandial glucose spikes. Short-acting insulins, like regular insulin, have a more gradual onset and are used similarly. Intermediate-acting insulins, such as NPH insulin, provide a longer duration of action, helping to maintain blood glucose levels between meals and overnight. Long-acting insulins, including glargine and detemir, offer a steady basal insulin release throughout the day, mimicking the body’s natural insulin production.
Treating diabetes with insulin beta is a complex process, requiring careful monitoring and adjustments. While researching the latest advancements in insulin beta therapy, I stumbled upon news about a popular LED mask being recalled. This raises important questions about product safety, especially when considering the potential for health-related gadgets like these. Fortunately, resources like this popular LED mask being recalled what to know article provide essential information for consumers.
Thankfully, the science behind insulin beta therapy remains promising, and I’m optimistic about future developments in diabetes treatment.
Efficacy and Safety Profiles of Different Insulin Types, Treating diabetes with insulin beta
The efficacy and safety profiles of various insulin types are significant considerations in treatment planning. Rapid-acting insulins, for instance, are highly effective in controlling postprandial glucose excursions but require careful timing of administration. Long-acting insulins, on the other hand, provide consistent basal coverage but may increase the risk of hypoglycemia if not properly adjusted. The duration of action, peak effect, and overall glucose-lowering potential of each insulin type play a critical role in patient management.
Limitations of Current Diabetes Treatments
Current treatments for diabetes, while effective in many cases, have inherent limitations. The need for multiple daily injections or the inconvenience of continuous subcutaneous insulin infusion (CSII) devices can negatively impact patients’ adherence to treatment regimens. Potential side effects, such as hypoglycemia, weight gain, and allergic reactions, may also limit treatment options for some individuals. Furthermore, achieving optimal glycemic control while minimizing long-term complications remains a challenge for many patients.
Insulin Delivery Methods: Pros and Cons
Different insulin delivery methods offer varying degrees of convenience and control.
| Delivery Method | Pros | Cons |
|---|---|---|
| Syringe and needle | Cost-effective, widely available, simple to use. | Requires precise timing, potential for injection site reactions, and can be inconvenient for frequent injections. |
| Insulin pen | More convenient than syringes, easier to dose accurately, less chance of accidental needle-stick injuries. | Higher cost than syringes, requires careful handling to avoid improper dosing. |
| Continuous subcutaneous insulin infusion (CSII) | Provides more consistent glucose control, reduces the need for multiple daily injections, potentially improving quality of life. | Requires technical knowledge and training, higher cost, increased risk of hypoglycemia if not properly managed, potential for device malfunctions. |
| Insulin pump | Allows for flexible insulin delivery, reduces blood glucose fluctuations, improves quality of life, provides more consistent glucose control. | Requires significant training and technical knowledge, higher cost, increased risk of hypoglycemia if not managed properly, potential for device malfunctions. |
Treating Diabetes with Insulin Beta Cell Therapies
A promising frontier in diabetes treatment lies in therapies targeting the root cause: dysfunction or destruction of insulin-producing beta cells in the pancreas. This approach, unlike simply managing blood sugar, aims to restore the body’s natural ability to regulate glucose. By understanding the mechanisms behind beta cell failure and developing strategies to replace or regenerate them, researchers are striving to offer a more comprehensive and potentially curative solution for diabetes.Replacing or repairing damaged beta cells presents a compelling strategy for diabetes treatment.
Current insulin-based therapies address symptoms but do not address the underlying cause. The goal of beta cell therapies is to restore the body’s intrinsic ability to produce and secrete insulin, potentially leading to long-term remission and improved quality of life.
Insulin Beta Cell Replacement Strategies
The concept of replacing damaged beta cells involves transplanting functional beta cells into the pancreas. This transplantation can be derived from various sources, including human islets, stem cells, or even genetically engineered cells. The potential benefits of this approach are substantial, offering a long-term solution that could reduce the need for daily insulin injections. However, challenges remain, including immune rejection and the availability of suitable donor cells.
Stimulating Insulin Beta Cell Regeneration
Several approaches are being explored to stimulate the regeneration of insulin-producing beta cells. These strategies aim to trigger the body’s natural repair mechanisms, potentially fostering the growth of new beta cells. Strategies include the use of growth factors, immunomodulatory agents, and even gene therapy to enhance beta cell survival and proliferation. These methods offer a less invasive alternative to transplantation, focusing on restoring the body’s natural regenerative capacity.
Insulin Beta Cell Transplantation: Potential and Challenges
Insulin beta cell transplantation, involving the implantation of healthy beta cells from a donor into the recipient’s pancreas, holds significant promise for treating diabetes. Success depends on the careful selection and preparation of donor cells and the recipient’s immune response. Studies have demonstrated the potential for improved glycemic control and reduced insulin requirements in recipients following successful transplantation.
However, immune rejection remains a significant hurdle, requiring immunosuppressive therapies that can have long-term side effects. Ethical considerations regarding the source of donor cells and the potential for misuse also need careful consideration.
Ethical Considerations and Challenges of Beta Cell Therapies
The use of beta cell therapies raises several ethical concerns. One major concern is the source of donor cells, whether from cadavers, stem cells, or genetically engineered cells. Furthermore, the potential for immune rejection requires immunosuppressive medications that may have significant side effects. The cost and accessibility of these treatments are also critical factors that must be addressed for equitable access.
Summary of Insulin Beta Cell Therapies
| Therapy Type | Description | Potential Benefits | Challenges |
|---|---|---|---|
| Insulin Beta Cell Transplantation | Implantation of healthy beta cells into the recipient’s pancreas. | Potential for long-term remission, reduced insulin dependency. | Immune rejection, availability of donor cells, immunosuppressive therapy side effects. |
| Insulin Beta Cell Regeneration | Stimulating the body’s natural repair mechanisms to regenerate beta cells. | Less invasive than transplantation, potentially addressing underlying causes. | Effectiveness and long-term efficacy remain to be determined, potential side effects of therapies. |
Research and Development in Insulin Beta Cell Therapy
The quest to find a cure for diabetes often hinges on the ability to regenerate or replace damaged insulin-producing beta cells in the pancreas. Current research is actively exploring various avenues to achieve this goal, including the use of stem cells and other regenerative medicine approaches. These innovative techniques hold promise for a future where individuals with diabetes can potentially live healthier lives.Regenerative medicine approaches for diabetes treatment focus on stimulating the body’s natural repair mechanisms to restore lost or damaged insulin-producing beta cells.
This can involve prompting the pancreas to generate new beta cells or introducing functional beta cells through transplantation. Early clinical trials and ongoing research provide valuable insights into the efficacy and safety of these approaches, offering a glimpse into the future of diabetes management.
Stimulating Insulin Beta Cell Regeneration
Researchers are actively pursuing strategies to stimulate the regeneration of insulin-producing beta cells within the pancreas. These strategies aim to encourage the pancreas to naturally produce new beta cells, potentially reducing or eliminating the need for lifelong insulin injections. Methods include the use of growth factors, which can signal cells to proliferate and differentiate into beta cells, as well as manipulating the local environment within the pancreas to foster a more conducive environment for beta cell growth.
Exciting advancements are continuously being made in this area, offering hope for individuals with diabetes.
Stem Cell Therapies
Stem cell therapies represent a promising frontier in regenerative medicine for diabetes. These therapies leverage the remarkable ability of stem cells to differentiate into various cell types, including beta cells. Stem cells can be sourced from various sources, each with its own advantages and disadvantages. The goal is to cultivate and implant these stem cells into the pancreas, where they can mature and produce insulin, thus restoring normal blood glucose levels.
Different types of stem cells are being explored for their potential in this area.
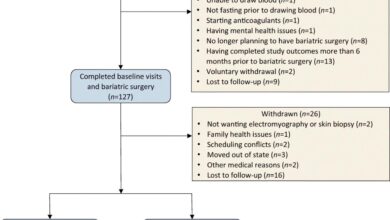
Examples of Clinical Trials and Ongoing Research Studies
Several clinical trials are currently underway, investigating the safety and efficacy of stem cell-based therapies for diabetes. These trials often involve transplanting stem cells derived from different sources, such as embryonic stem cells, induced pluripotent stem cells (iPSCs), or mesenchymal stem cells, into the pancreas of individuals with type 1 or type 2 diabetes. The results of these trials are eagerly awaited to evaluate the long-term effects and potential benefits of these treatments.
Comparison of Stem Cell Types
| Stem Cell Type | Source | Advantages | Disadvantages |
|---|---|---|---|
| Embryonic Stem Cells | Embryos | High differentiation potential | Ethical concerns, immune rejection |
| Induced Pluripotent Stem Cells (iPSCs) | Adult cells reprogrammed | Avoids ethical concerns, potentially reduced immune rejection | Efficiency of reprogramming, long-term safety |
| Mesenchymal Stem Cells (MSCs) | Bone marrow, adipose tissue | Lower immunogenicity, relatively easier to obtain | Limited differentiation potential compared to iPSCs or embryonic stem cells |
This table provides a concise overview of the different stem cell types utilized in insulin beta cell therapy. Each type offers unique advantages and disadvantages, influencing the choice of approach for individual clinical trials.
Potential Benefits and Limitations: Treating Diabetes With Insulin Beta
Treating diabetes with insulin beta cell therapies holds immense promise for revolutionizing diabetes management. However, like any medical advancement, these therapies come with potential benefits and limitations that must be carefully considered. This section explores the advantages, risks, and practical implications of these innovative approaches.
Potential Advantages
Insulin beta cell therapies offer the tantalizing prospect of restoring or enhancing the body’s natural ability to produce insulin. This could lead to a more stable blood sugar control, reducing the need for frequent insulin injections or the inherent risks associated with daily medication management. Furthermore, the potential for a personalized treatment approach, tailored to the individual’s needs, could enhance the quality of life for those with diabetes.
- Improved glycemic control: Restoring functional beta cells can lead to a more consistent and stable blood sugar level, reducing the frequency of highs and lows, which can be detrimental to overall health. This can significantly reduce the need for exogenous insulin injections or other daily medications.
- Reduced risk of long-term complications: Maintaining consistent blood sugar levels can mitigate the development or progression of long-term diabetes complications such as neuropathy, nephropathy, and retinopathy.
- Enhanced quality of life: The improved metabolic stability and reduced reliance on daily medication can lead to a higher quality of life for patients. Patients can engage in activities and routines without the constant worry of blood sugar fluctuations.
- Potential for personalized treatment: Future therapies might allow for a more individualized approach, tailoring treatment to specific genetic predispositions and metabolic profiles. This can result in more effective and efficient therapies.
Potential Risks and Limitations
Despite the potential advantages, insulin beta cell therapies are not without inherent risks. Careful consideration must be given to the safety and efficacy of these therapies before widespread adoption.
- Immune rejection: Transplanted cells may be rejected by the recipient’s immune system, requiring immunosuppressive drugs to prevent rejection. This can have its own set of side effects. For example, long-term use of immunosuppressants can increase the risk of infections and certain cancers.
- Tumor formation: In some cases, transplanted cells may have the potential to form tumors, although this is a rare occurrence. This is a critical concern that requires stringent safety monitoring during and after transplantation.
- Ethical considerations: The use of stem cells or other sources for creating beta cells raises ethical concerns related to their origin and use. Careful consideration and regulation of the source materials are essential.
- Variability in effectiveness: The efficacy of beta cell therapies can vary significantly between individuals, making it crucial to develop personalized treatment approaches to ensure optimal results.
Long-Term Effects and Potential Complications
The long-term effects of insulin beta cell therapies remain a subject of ongoing research. Potential complications need careful evaluation.
- Long-term immunosuppression: Immunosuppressants used to prevent rejection can have long-term side effects, such as increased risk of infections and certain types of cancers. Careful monitoring is crucial for minimizing these risks.
- Development of new complications: Although potentially reducing existing complications, new complications might arise as a result of the therapy itself, requiring further research to identify and mitigate them.
- Maintaining cell function: Long-term stability of transplanted beta cells is crucial. Strategies to ensure the cells function properly and maintain their function over time are essential to maximizing the therapeutic benefits.
Cost-Effectiveness and Accessibility
The cost-effectiveness and accessibility of insulin beta cell therapies are critical factors for widespread adoption.
- High initial costs: The development and implementation of these therapies may initially incur high costs, making them potentially inaccessible to many. This can create disparities in healthcare access.
- Ongoing costs: The need for ongoing monitoring, medication, and potential follow-up procedures will also contribute to the long-term cost of these therapies.
- Research and development: Continued investment in research and development is critical to improving the cost-effectiveness and accessibility of these therapies.
Comparison of Approaches
| Therapy Approach | Potential Benefits | Potential Drawbacks |
|---|---|---|
| Stem cell-derived beta cells | Potential for personalized treatment, scalability | Ethical concerns, immune rejection, tumor formation risk |
| Islet transplantation | Potential for improved glycemic control, reduced reliance on insulin | Immune rejection, need for immunosuppression, limited donor availability |
| Gene therapy | Potential for long-term solution, personalized approach | Potential off-target effects, safety concerns, cost |
The Future of Diabetes Treatment

The journey towards a future free from the debilitating effects of diabetes is driven by innovative research and technological advancements. Insulin beta cell therapies, particularly those focused on regeneration and transplantation, are poised to revolutionize diabetes management, offering the potential for a cure or significantly improved control. This approach moves beyond simply managing symptoms, aiming to restore the body’s natural ability to regulate blood sugar.Current treatments for diabetes primarily focus on managing blood glucose levels.
However, the future promises a shift towards therapies that address the root cause of the disease, leading to long-term remission and potentially preventing complications. This paradigm shift is expected to lead to significant improvements in patient quality of life and reduce the overall burden of diabetes on healthcare systems.
Future Directions in Insulin Beta Cell Therapies
Research into insulin beta cell therapies is progressing rapidly. Scientists are exploring various approaches, from genetic engineering to biomaterials, to enhance beta cell function and survival. One promising area is the development of 3D bioprinting techniques to create functional islets of Langerhans, the clusters of cells in the pancreas that produce insulin. These bioengineered islets could potentially be transplanted into patients, offering a personalized and effective treatment.
Additionally, stem cell therapies are being investigated to generate new beta cells, potentially eliminating the need for donor cells. This is a critical step in ensuring access and minimizing the ethical concerns associated with donor organs.
Treating diabetes with insulin beta can be a game-changer for managing blood sugar levels. Finding the right balance, though, can sometimes take some trial and error. Speaking of finding the right balance, a good night’s sleep is crucial for overall health, especially if you’re managing a chronic condition like diabetes. That’s why investing in a supportive mattress, like the ones reviewed in the guide on the best mattress for back sleepers , is important.
A comfortable mattress can help you get the restful sleep you need to support your insulin beta therapy and overall well-being.
Potential Impact on Diabetes Management
The impact of insulin beta cell therapies on diabetes management is expected to be profound. Imagine a future where individuals with type 1 diabetes could potentially lead normal, healthy lives without daily insulin injections. For type 2 diabetes, the prospect of restoring or enhancing insulin production could significantly improve metabolic control, reducing the risk of long-term complications. Furthermore, these therapies might play a crucial role in preventing diabetes in susceptible individuals.
Early intervention strategies could focus on bolstering beta cell function to prevent the onset of the disease, potentially reversing the pre-diabetic state.
Predicted Advancements and Breakthroughs
Several breakthroughs are anticipated in the coming years. Improved understanding of the complex signaling pathways involved in beta cell function could lead to the development of targeted therapies. Furthermore, advances in immunology could potentially minimize immune rejection of transplanted cells. The development of closed-loop systems integrating insulin beta cell therapies with continuous glucose monitoring (CGM) and automated insulin delivery devices could create a truly personalized and effective treatment approach.
Such advancements will provide a significant leap in the management of diabetes.
Impact on Healthcare Systems
| Aspect | Predicted Impact ||—|—|| Reduced Healthcare Costs | Lower long-term costs associated with diabetes complications, such as kidney failure, heart disease, and blindness. Reduced need for frequent hospitalizations. || Improved Patient Outcomes | Increased quality of life and reduced burden of disease for patients. Enhanced metabolic control and reduced risk of long-term complications. || Increased Access to Care | Potential for wider availability of treatment, particularly for individuals with limited access to current treatments.
This is especially crucial in developing countries. || Enhanced Research and Development | Increased investment in diabetes research, leading to further advancements in diagnosis and treatment. This is crucial to maintain a forward-thinking approach to diabetes management. || Shift in Focus | Transition from primarily reactive treatment to proactive prevention and cure strategies. |
Illustrative Case Studies
Unveiling the potential of insulin beta cell therapies requires a deeper look into real-world applications. This section presents case studies, illustrating the diverse treatment approaches, outcomes, and experiences of individuals undergoing these innovative therapies. Each case offers a glimpse into the journey of patients navigating this promising frontier in diabetes treatment.These case studies are not intended to represent a comprehensive overview of all possible outcomes.
Rather, they highlight specific instances of how these therapies are being employed and the results observed. Understanding the nuances of each individual’s response to the treatment allows for a more nuanced discussion about the potential benefits and limitations of this therapeutic approach.
Case Study Summaries
These case studies offer a glimpse into the variety of responses to insulin beta cell therapies, underscoring the need for personalized treatment plans. Recognizing individual differences in patient response is crucial for developing effective and tailored approaches to diabetes management.
| Case Study | Therapy Approach | Patient Profile | Outcome | Patient Experience |
|---|---|---|---|---|
| Case 1 | Islet transplantation | A 45-year-old male with type 1 diabetes, diagnosed at age 20. Patient exhibited significant complications, including neuropathy and nephropathy. | Partial restoration of insulin production, leading to a significant reduction in daily insulin requirements. Improvement in neuropathy symptoms, and stabilization of kidney function. | The patient reported a substantial improvement in quality of life, with reduced reliance on multiple daily injections and better control over blood glucose levels. |
| Case 2 | Stem cell-derived beta cell transplantation | A 32-year-old female with type 2 diabetes, diagnosed at age 28. She had struggled with medication compliance and experienced poor glycemic control. | Improved glycemic control, and a noticeable decrease in the need for oral hypoglycemic medications. However, some residual insulin dependence remained. | The patient expressed satisfaction with the procedure, noting a reduction in the frequency and severity of hypoglycemic episodes. She appreciated the potential long-term impact on her overall health. |
| Case 3 | Gene therapy targeting beta cell function | A 60-year-old female with type 2 diabetes, diagnosed at age 55. Patient presented with a history of cardiovascular disease. | Significant reduction in blood glucose levels, and improvement in overall metabolic profile. Notably, a stabilization of cardiovascular risk factors. | The patient reported a noticeable improvement in energy levels and overall well-being, attributing this to the sustained control of blood glucose levels. |
Effectiveness of Different Therapies
Analyzing the effectiveness of various insulin beta cell therapies reveals a pattern of variable outcomes. Islet transplantation, for example, has demonstrated positive results in restoring insulin production and reducing reliance on exogenous insulin. However, the success is contingent on factors like patient health status and the extent of pre-existing complications. Stem cell-derived beta cell therapies also hold promise, but require further investigation to understand the long-term efficacy and potential complications.
Gene therapy approaches, although promising, need further clinical trials to fully assess their potential and safety profile.
Last Word
In conclusion, treating diabetes with insulin beta therapies holds immense promise for revolutionizing diabetes management. While challenges remain, ongoing research and development, combined with a deeper understanding of insulin beta cell function, offer hope for a future where individuals with diabetes can achieve better control and improved quality of life. The ethical considerations and potential long-term effects must be carefully evaluated alongside the potential benefits.
The path forward requires continued dedication and innovation to unlock the full potential of this promising field.