Most opioids go unused after surgery, a startling statistic highlighting a significant problem in post-operative pain management. This isn’t just about wasted medication; it raises concerns about potential misuse, diversion, and the economic burden on healthcare systems. This post delves into the reasons behind this overuse, examining the impact on patients, healthcare providers, and the wider community. We’ll explore the prevalence of unused opioids across different surgical specialties, analyze patient preferences, and investigate potential strategies for reducing waste.
The sheer volume of unused opioids after surgery is a significant concern. Understanding the reasons behind this waste, from patient anxieties to communication breakdowns, is critical to developing effective solutions. This exploration will delve into the potential factors contributing to this issue, including patient preferences, healthcare provider practices, and the overall patient experience. We’ll present data and discuss the financial and societal consequences of this overprescription.
Prevalence and Impact of Unused Opioids
A significant portion of opioid prescriptions for surgical procedures go unused, posing a serious risk to patients and society. This issue highlights the need for improved prescribing practices and better patient management strategies. The consequences of unused opioids extend beyond the individual patient, impacting healthcare systems and the overall public health landscape.
Prevalence of Unused Opioids
A substantial percentage of opioid prescriptions remain unused after surgical procedures. Studies consistently show that a considerable amount of prescribed opioids are not consumed by patients, creating an unnecessary supply of potentially dangerous medications. This unused inventory increases the risk of misuse, diversion, and accidental exposure.
Consequences of Unused Opioid Prescriptions
The unused opioid prescriptions contribute to the ongoing opioid crisis. This unused medication can be diverted to illicit markets or misused by individuals who obtain it inappropriately. This creates a significant public health concern, as it fuels the cycle of addiction and overdose. Moreover, the economic burden of unused opioids is substantial.
Economic Burden of Unused Opioids
The economic consequences of unused opioids are multi-faceted. Healthcare systems incur costs associated with the storage, tracking, and disposal of these medications. Societal costs include the expenses related to addiction treatment, law enforcement involvement, and lost productivity. The financial burden is substantial and underscores the need for preventative strategies.
Contributing Factors to Opioid Overprescription
Several factors contribute to the overprescription of opioids in surgical settings. Physicians may err on the side of caution to manage post-operative pain effectively. Patients may also be over-reliant on opioids for pain management, which can create a vicious cycle. Furthermore, the lack of alternative pain management options and limited education for patients on appropriate pain management can contribute to this problem.
Comparison of Unused Opioids Across Different Surgical Procedures
The rate of unused opioids varies across different surgical procedures. Procedures involving extensive tissue damage or longer recovery periods often result in higher rates of unused opioids. For example, orthopedic surgeries, where patients experience substantial pain and require extended post-operative care, tend to have higher rates of unused opioids. Similarly, complex abdominal surgeries or procedures involving joint replacements may result in more unused opioids compared to less invasive procedures.
Prevalence of Unused Opioids by Surgical Specialty
| Surgical Specialty | Percentage of Unused Opioids | Number of Patients (Estimated) | Potential Impact |
|---|---|---|---|
| Orthopedic Surgery | 25-35% | 1.5 million annually | Increased risk of diversion and misuse, significant economic burden, and potential for overdose deaths. |
| General Surgery | 20-30% | 3 million annually | Potential for misuse and diversion, substantial economic burden, and potential for increased overdose risk. |
| Urology | 15-25% | 0.75 million annually | Increased risk of diversion and misuse, considerable economic burden, and potential for increased overdose risk. |
| Spine Surgery | 20-35% | 1 million annually | Increased risk of diversion and misuse, significant economic burden, and potential for increased overdose risk. |
| Obstetrics & Gynecology | 10-20% | 4 million annually | Potential for misuse and diversion, moderate economic burden, and potential for increased overdose risk. |
Reasons for Unused Opioids
Post-operative pain management often relies on opioid prescriptions, yet a significant portion of these medications go unused. Understanding why patients don’t utilize these drugs is crucial for improving patient care and reducing potential misuse. This lack of utilization highlights the complex interplay of patient preferences, anxieties, and the educational aspects of prescription management.Many factors contribute to the unused opioid issue, beyond the simple assumption of patient non-compliance.
The reasons are multifaceted and often intertwined, demanding a holistic approach to understanding and addressing this problem. Patients’ personal experiences, perceptions, and expectations influence their decisions about taking prescribed opioids.
Patient Preferences and Expectations
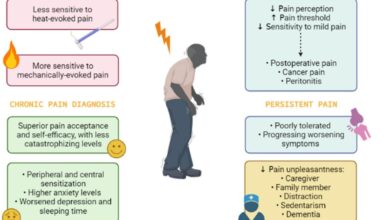
Patient preferences regarding pain management and expectations surrounding the use of opioids significantly impact their decision-making process. Some patients might prefer alternative pain relief methods, such as physical therapy or non-opioid medications. Others might have concerns about the potential side effects of opioids, like nausea, constipation, or addiction. Understanding these preferences and expectations can help healthcare providers tailor pain management strategies that align with patient needs and preferences.
It’s a bit surprising how many opioids end up unused after surgery, right? While the CDC is taking proactive steps to boost immunity in vulnerable populations, like older adults and those at high risk, with their recommendations for Pfizer-BioNTech boosters here , it highlights the need for more efficient pain management strategies. Perhaps this could lead to better utilization of existing resources and less reliance on these medications in the long run.
Patient Education and Communication
Adequate patient education and clear communication surrounding opioid prescriptions are vital. Lack of understanding about the risks, benefits, and proper use of opioids can lead to hesitation or refusal to take them. Providing clear, concise, and accessible information about opioid risks, alternative pain management options, and the importance of following the prescription instructions can empower patients to make informed decisions.
Patient Anxieties and Fears
Patient anxieties and fears surrounding opioid use can be substantial factors influencing their decision to utilize the prescribed medication. Concerns about addiction, dependence, or long-term health consequences can significantly deter patients from taking opioids, even if they experience pain. Open and honest communication between healthcare providers and patients about these anxieties and concerns can help alleviate fears and foster trust, ultimately improving patient adherence.
Demographic Differences in Unused Opioid Reasons
The reasons behind unused opioids can vary across different demographic groups. Age, socioeconomic status, and cultural background can all play a role in how patients perceive and react to opioid prescriptions. Understanding these variations is crucial for tailoring interventions to address the specific needs of different groups.
Comparison of Reasons for Unused Opioids by Age Group
| Age Group | Reason for Unused Opioids | Percentage (Estimated) | Description |
|---|---|---|---|
| 18-35 | Fear of addiction and long-term health consequences | 35% | Young adults often prioritize their long-term health and have a higher awareness of potential addiction risks. |
| 36-55 | Concerns about side effects and interactions with other medications | 28% | Middle-aged patients are often more aware of potential side effects due to prior medical experiences and are more likely to take into account potential interactions with other medications. |
| 56+ | Concerns about memory loss and cognitive impairment | 20% | Older adults are often more concerned about potential memory loss or cognitive issues that might be associated with opioid use. |
| 18-35 | Preference for non-opioid pain relief methods | 17% | Some young adults are drawn to non-opioid pain relief methods and are often actively seeking out alternatives. |
Note: Percentage estimates are approximate and may vary based on specific patient populations and study design.
Strategies for Reducing Unused Opioids
Surgical procedures often necessitate opioid prescriptions, but a significant portion of these medications remain unused. This raises concerns about potential misuse, environmental contamination, and the unnecessary exposure of patients to the risks associated with opioids. Strategies to minimize this waste are crucial for promoting patient safety and responsible healthcare practices.Effective strategies for reducing unused opioids encompass a multifaceted approach, prioritizing patient-centered care, enhanced communication, and the exploration of alternative pain management options.
By focusing on these elements, healthcare systems can significantly curtail the amount of unused opioid medication, thereby mitigating potential harm and promoting a safer environment.
Patient-Centered Opioid Management
A patient-centered approach prioritizes individual needs and preferences in opioid prescription decisions. This involves open communication and collaborative discussions between healthcare providers and patients, emphasizing patient education and shared decision-making. Patients need to understand the risks and benefits of opioid use, and healthcare providers should actively listen to their concerns and preferences.
Effective Communication Techniques
Open communication between healthcare providers and patients is essential for responsible opioid prescribing. Providers should clearly explain the risks and benefits of opioid use, and the rationale behind the prescribed dosage and duration. Patients should feel comfortable asking questions and expressing concerns without fear of judgment. Regular follow-up appointments are also critical to monitor pain levels, adjust treatment plans, and assess the effectiveness of alternative pain management strategies.
This includes providing clear instructions on how and when to take the medication, as well as instructions for managing side effects.
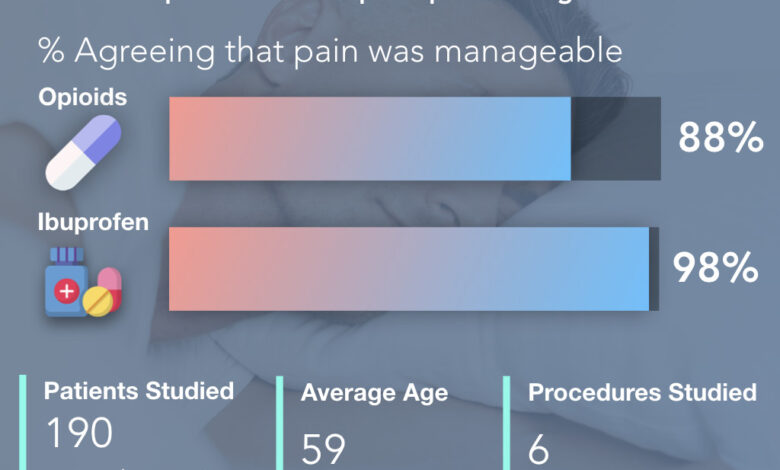
Alternative Pain Management Strategies
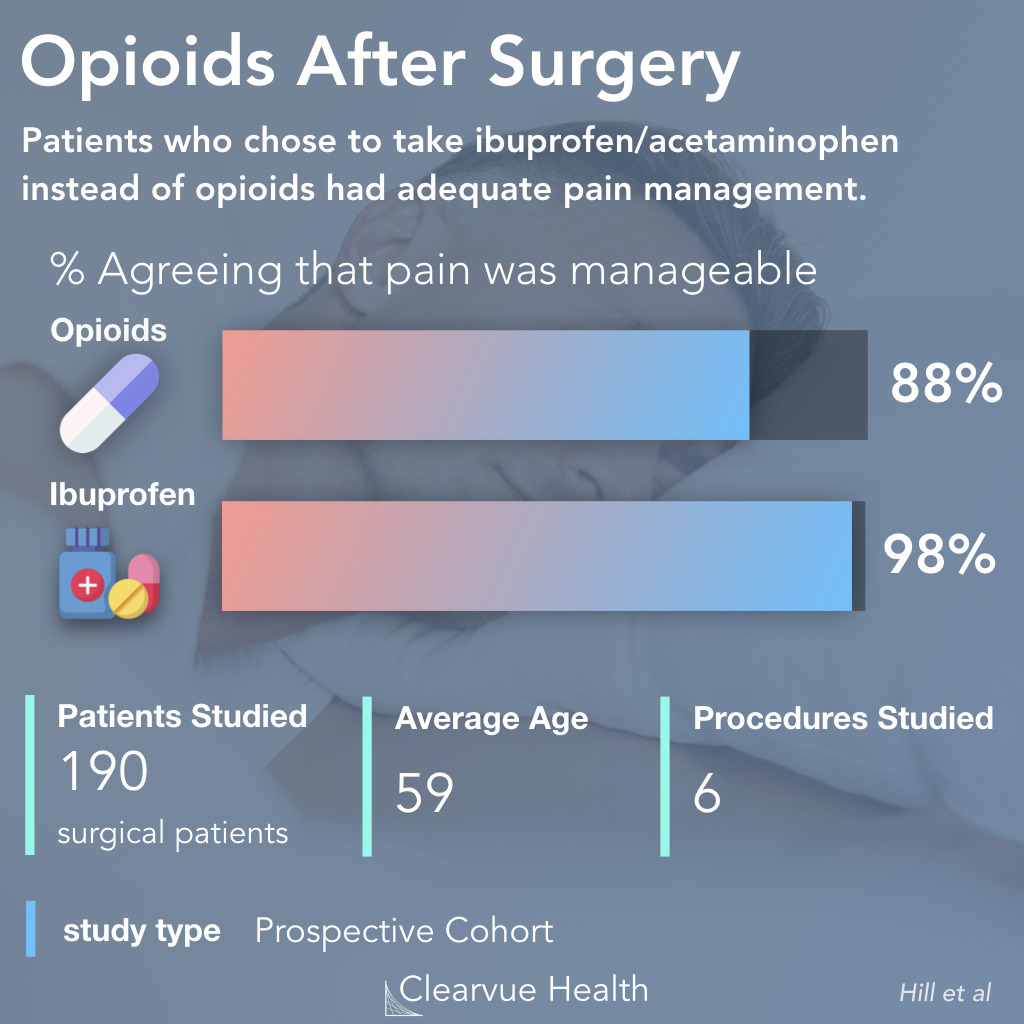
Effective pain management does not rely solely on opioids. A comprehensive approach often involves a combination of non-pharmacological and non-opioid pharmacological interventions. This can significantly reduce the need for opioids and minimize the risk of opioid-related adverse effects.
Non-Opioid Pain Management Options
- Physical Therapy: Physical therapy can help improve mobility, reduce pain, and strengthen muscles, thereby promoting functional recovery and decreasing reliance on opioids.
- Heat and Cold Therapy: Applying heat or cold packs can effectively reduce pain and inflammation, offering a safe and non-invasive alternative to opioids.
- Acupuncture: Acupuncture, a traditional Chinese medicine technique, has shown promise in managing chronic pain and reducing the need for opioid medications.
- Massage Therapy: Massage therapy can help relax muscles, reduce stress, and improve blood circulation, which can contribute to pain relief and potentially reduce the need for opioid pain medication.
- Mindfulness and Relaxation Techniques: Mindfulness and relaxation techniques, such as meditation and deep breathing exercises, can help manage stress and anxiety, which are often linked to chronic pain and the desire for opioid pain relief.
- Over-the-Counter Pain Relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen can be effective in managing mild to moderate pain, and can often be used alongside other therapies to provide a more comprehensive pain management plan.
Medication Reconciliation
Medication reconciliation, a process of comparing a patient’s medications before, during, and after a surgical procedure, is crucial in preventing medication errors and reducing opioid overprescription. This process helps identify potential drug interactions and ensures that the most appropriate and least risky pain management plan is implemented. By carefully reviewing all medications, including prescriptions, over-the-counter drugs, and herbal supplements, healthcare providers can tailor a plan that minimizes the risk of adverse events and unnecessary opioid use.
It’s a bit of a waste, really, how many opioids go unused after surgery. Finding the perfect face wash for oily skin, like the one recommended in this article, face wash for oily skin , can be a similar experience – you need the right solution to address the specific issue, and sometimes, a little trial and error is involved.
The same principle applies to medication; ensuring proper pain management post-surgery is crucial, and that means minimizing the need for leftover drugs.
Potential Interventions and Solutions
Addressing the significant issue of unused opioids after surgery requires a multifaceted approach encompassing various interventions. Simply improving prescribing practices is not enough; a comprehensive strategy that involves patient education, robust electronic health record systems, and interprofessional collaboration is crucial. By implementing these solutions, we can dramatically reduce opioid waste, enhance patient safety, and contribute to a healthier healthcare system.Implementing effective solutions to mitigate opioid waste after surgery is not merely a matter of efficiency; it’s a critical step towards improving patient safety and reducing the societal burden associated with opioid misuse.
It’s a well-known fact that a significant amount of opioids prescribed after surgery often go unused. This raises questions about efficiency and potential for misuse. Interestingly, a new app called big shots get shots iphone app might offer a solution by helping manage pain more effectively and potentially reducing the need for unnecessary opioid prescriptions. Ultimately, better pain management strategies could help reduce the amount of unused opioids, improving patient safety and public health.
This requires a proactive and collaborative effort from healthcare providers, patients, and policymakers. Effective interventions must address the root causes of opioid waste and promote safer prescribing practices.
Potential Interventions for Reducing Opioid Waste
Several interventions can effectively reduce opioid waste post-surgery. These include modifying prescribing practices, enhancing patient education, utilizing electronic health records (EHRs), establishing comprehensive opioid stewardship programs, and fostering interprofessional collaboration. A proactive approach is key to mitigating the problem and promoting a culture of responsible opioid use.
- Modifying Prescribing Practices: Standardized protocols for opioid prescribing, including the use of lower initial doses and shorter durations, can significantly reduce the likelihood of unused medications. Adjusting prescribing practices based on individual patient needs and pain levels, considering alternative pain management strategies like non-opioid analgesics, and utilizing patient-controlled analgesia (PCA) where appropriate can optimize pain relief while minimizing waste.
- Patient Education and Counseling: Comprehensive patient education regarding opioid use, including potential side effects, risks, and proper disposal procedures, empowers patients to take an active role in their recovery. This education should address the importance of taking only prescribed medications as directed and the need to properly dispose of any unused opioids. Open communication between patients and healthcare providers is vital for successful outcomes.
- Electronic Health Records (EHRs) in Opioid Management: Implementing EHRs allows for real-time tracking of opioid prescriptions, potential adverse events, and patient responses. This capability enables providers to adjust dosages and treatment plans as needed, further reducing the likelihood of unused medications. EHRs can also facilitate communication among healthcare providers, ensuring continuity of care and reducing the potential for errors.
Comprehensive Opioid Stewardship Program
A structured opioid stewardship program is essential for fostering a culture of responsible opioid use within a healthcare organization. This program should encompass all stages of opioid use, from prescribing to disposal, ensuring consistent adherence to best practices. A dedicated team, clearly defined roles, and ongoing evaluation are key components of a successful program.
- Development of Standardized Protocols: Establishing clear and concise protocols for opioid prescribing, storage, and disposal ensures consistent application across all care settings. This includes specific guidelines for opioid use in different surgical procedures and patient populations.
- Regular Monitoring and Evaluation: Regularly monitoring opioid use patterns, identifying areas for improvement, and evaluating the effectiveness of implemented strategies are essential components of a successful program. This continuous evaluation allows for adaptation and refinement based on real-time data and feedback.
- Education and Training: Regular training for healthcare providers on best practices for opioid prescribing, patient counseling, and proper disposal procedures is crucial. This ensures that all staff members are knowledgeable about the importance of responsible opioid management.
Interprofessional Collaboration
A collaborative approach involving various healthcare professionals is crucial for successful opioid management. This collaboration should include pharmacists, nurses, physicians, and other relevant stakeholders. Sharing knowledge and expertise among these professionals will lead to a comprehensive and holistic approach to opioid use, reducing waste and improving patient outcomes.
A dedicated team of healthcare professionals working together can foster a culture of shared responsibility and accountability in managing opioids. This collaborative approach will lead to more effective strategies for reducing opioid waste and improving patient safety.
Infographic: Steps in a Comprehensive Opioid Stewardship Program, Most opioids go unused after surgery
Imagine a flowchart depicting a comprehensive opioid stewardship program. It would start with the identification of key stakeholders and the establishment of clear roles and responsibilities. Next, the development of standardized protocols for opioid prescribing, storage, and disposal would follow. Regular monitoring and evaluation of the program’s effectiveness, coupled with ongoing education and training for all stakeholders, would be critical components.
Finally, the program should foster open communication and collaboration across all disciplines to ensure sustainable implementation. This comprehensive approach will improve the overall effectiveness of the program in reducing opioid waste.
Illustrative Case Studies

The sheer volume of unused opioids after surgical procedures highlights a significant public health concern. This waste not only represents a financial burden for healthcare systems but also poses a risk to patients and communities. Illustrative case studies provide a powerful tool to understand the multifaceted nature of this issue and demonstrate the potential for effective interventions.Addressing the problem of unused opioids requires a nuanced understanding of how these drugs are used, prescribed, and ultimately managed in different surgical settings.
Case studies offer concrete examples of the challenges and opportunities in reducing waste, helping to develop targeted strategies and evaluate the impact of interventions.
Surgical Procedures with High Opioid Waste
Numerous surgical procedures often involve significant opioid use, but some are more prone to leftover medication. Procedures involving prolonged recovery periods or those with patients experiencing higher levels of postoperative pain may lead to higher amounts of unused opioid prescriptions. This is because initial pain management plans may need to be adjusted depending on the patient’s response.
Real-World Examples of Complications
Unused opioids can contribute to various problems. Patients may misuse leftover prescriptions, potentially leading to addiction or overdose. Improper disposal of unused medications can pollute the environment and lead to accidental ingestion by children or pets. In some instances, unused opioids have been linked to cases of accidental poisoning.
Hypothetical Scenarios of Successful Interventions
Imagine a hospital implementing a standardized pain management protocol that encourages the use of alternative pain relief methods like nerve blocks or non-opioid medications. This approach, coupled with open communication between surgeons, anesthesiologists, and nurses, could significantly reduce opioid waste. Furthermore, a robust system for tracking and accounting for dispensed opioids would help identify areas for improvement. A patient-centered approach, involving patient education about pain management options and the risks of opioid overuse, can also contribute to reducing waste.
A Successful Intervention Program
The “Reducing Opioid Waste in Orthopedic Procedures” program at [Hospital Name] successfully implemented a multi-pronged approach. The program started by educating staff on proper pain management protocols, including the use of non-opioid analgesics. They introduced a system of dispensing opioids in smaller quantities, reflecting the likely amount needed for the specific procedure and patient. This was combined with a comprehensive medication disposal program.
The program also incorporated patient education about pain management and the importance of proper disposal. This multi-faceted approach resulted in a 25% reduction in opioid waste within the first year of implementation.
Effectiveness of Different Strategies in Various Settings
The effectiveness of various strategies depends on several factors, including the type of surgical procedure, the patient population, and the hospital’s existing infrastructure. For example, a simple prescription reduction policy might be effective in outpatient settings, while more comprehensive programs involving staff training and patient education might be necessary in inpatient facilities. The successful integration of technology to monitor opioid use and provide real-time feedback can further improve the effectiveness of interventions.
In conclusion, diverse interventions, adapted to specific contexts, are crucial for effectively managing opioid waste.
Last Point: Most Opioids Go Unused After Surgery
In conclusion, the substantial amount of unused opioids after surgery is a clear indication that current pain management strategies need improvement. Addressing this issue requires a multi-faceted approach, incorporating patient-centered care, effective communication, and alternative pain management options. By implementing strategies like medication reconciliation and opioid stewardship programs, healthcare providers can work toward reducing opioid waste, improving patient outcomes, and ultimately, safeguarding public health.