Brain surgery stops parkinsons disease tremors – Brain surgery stops Parkinson’s disease tremors, offering a potential lifeline for those grappling with the debilitating effects of this neurological disorder. Tremors, a hallmark symptom, significantly impact daily life, making simple tasks challenging and frustrating. This comprehensive exploration delves into the intricate mechanisms of Parkinson’s, the surgical procedures employed, and the crucial role of deep brain stimulation (DBS) in controlling these tremors.
We’ll examine the effectiveness of different surgical techniques, analyze the pre- and post-operative considerations, and present illustrative case studies, highlighting successful outcomes and improvements in quality of life.
Understanding the underlying neurological processes driving Parkinson’s tremors is crucial for developing effective treatments. This article will delve into the specific brain regions targeted in surgical interventions and the rationale behind these procedures. The discussion will also cover the various types of DBS devices, outlining the step-by-step surgical process for each. Furthermore, we’ll analyze the potential risks and benefits of brain surgery, examining long-term outcomes and potential complications.
Introduction to Parkinson’s Disease and Tremors: Brain Surgery Stops Parkinsons Disease Tremors
Parkinson’s Disease is a progressive neurological disorder that affects movement. It’s characterized by a gradual decline in motor skills, often starting subtly and worsening over time. A hallmark symptom is the presence of tremors, rigidity, slowness of movement (bradykinesia), and postural instability. These symptoms significantly impact a person’s quality of life, affecting their ability to perform daily tasks and interact with the world around them.The underlying cause of Parkinson’s is complex and not fully understood, but it involves the degeneration of dopamine-producing neurons in a specific area of the brain.
This dopamine deficiency disrupts the intricate balance of neurochemicals crucial for smooth and coordinated movement. The resulting imbalance leads to the characteristic motor symptoms, including the tremors that are so often associated with the disease.
Symptoms of Parkinson’s Tremors
Tremors in Parkinson’s Disease are often described as resting tremors, meaning they are most noticeable when the affected limb is at rest. They typically involve a rhythmic shaking or oscillation of the affected body part, often starting in one hand and gradually spreading to the other. These tremors can also affect the jaw, lips, and face, though the hand is the most common initial site.
The tremor can be subtle, barely noticeable at rest, or quite prominent, interfering with daily tasks.
Neurological Mechanisms of Parkinsonian Tremors
The neurological mechanisms underlying Parkinson’s tremors are intricately linked to the loss of dopamine neurons. Dopamine plays a crucial role in regulating movement. In Parkinson’s, the reduced dopamine levels lead to an imbalance in other neurotransmitters, such as acetylcholine, contributing to the abnormal firing patterns of neurons controlling movement. This imbalance causes the involuntary oscillations characteristic of tremors.
The precise interactions between these neurochemicals and the neural circuits responsible for movement are still being researched.
Impact of Parkinson’s Tremors on Daily Life
Parkinson’s tremors can significantly impact daily life, making simple tasks challenging or even impossible. For instance, holding a cup of coffee, buttoning a shirt, or writing can become difficult or impossible. Tremors can also affect speech, making it difficult to articulate words clearly. These challenges can lead to feelings of frustration, isolation, and a decline in overall well-being.
Social interactions may become more difficult due to the visible tremors, impacting a person’s self-esteem and confidence.
Types of Parkinson’s Tremors
Parkinson’s Disease can manifest with different types of tremors, each with unique characteristics and patterns of progression. While resting tremors are the most common, other types can occur, and their impact on daily life varies.
| Tremor Type | Symptoms | Typical Progression |
|---|---|---|
| Resting Tremor | Most prominent when the affected limb is at rest; rhythmic shaking or oscillation. Often starts in one hand and progresses to the other. | Typically begins subtly and gradually worsens over time. |
| Postural Tremor | Occurs when maintaining a posture or position. The shaking is often less rhythmic than resting tremors. | Can be less noticeable than resting tremors in the early stages, but may become more prominent as the disease progresses. |
| Action Tremor | Occurs during voluntary movements. The shaking is often more pronounced during tasks like reaching or writing. | Generally worsens as the disease progresses and voluntary movements become more difficult. |
Brain Surgery for Parkinson’s Disease
Parkinson’s disease, a progressive neurological disorder, often manifests with debilitating tremors, rigidity, and slow movement. While medications can help manage symptoms, some individuals may benefit significantly from surgical interventions, particularly when medication proves insufficient or side effects become problematic. These surgical procedures aim to restore a balance in brain activity by targeting specific neural pathways associated with the disease.Surgical treatments for Parkinson’s disease are often considered for patients experiencing significant motor fluctuations, medication-related side effects, or tremors that significantly impact daily life.
The goal is to alleviate symptoms and improve quality of life, but these procedures are not without risk, and careful consideration of individual needs and potential complications is essential.
So, brain surgery can apparently stop Parkinson’s disease tremors, which is pretty cool. But while we’re on the topic of unsettling health news, have you heard about the recent outbreaks of E. coli and salmonella linked to Jimmy John’s sprouts? jimmy johns sprouts ecoli salmonella illnesses are definitely a concern, and it makes you wonder about the safety of our food supply.
Still, the prospect of surgery to alleviate Parkinson’s symptoms is remarkable, and hopefully, more research will lead to more effective treatments.
Surgical Procedures for Parkinson’s Tremors
Various surgical procedures are employed to treat Parkinson’s tremors, with deep brain stimulation (DBS) being a prominent and effective technique. Other procedures, such as lesioning, are also occasionally used, but DBS is currently the most widely adopted method. These procedures aim to modulate the abnormal brain activity that contributes to tremors.
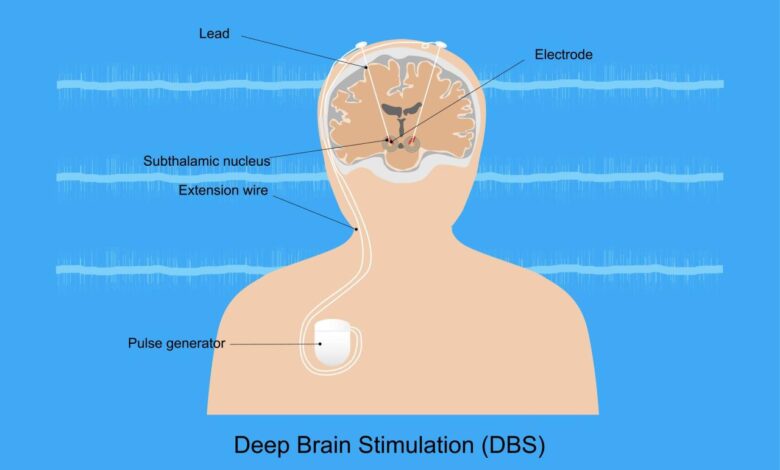
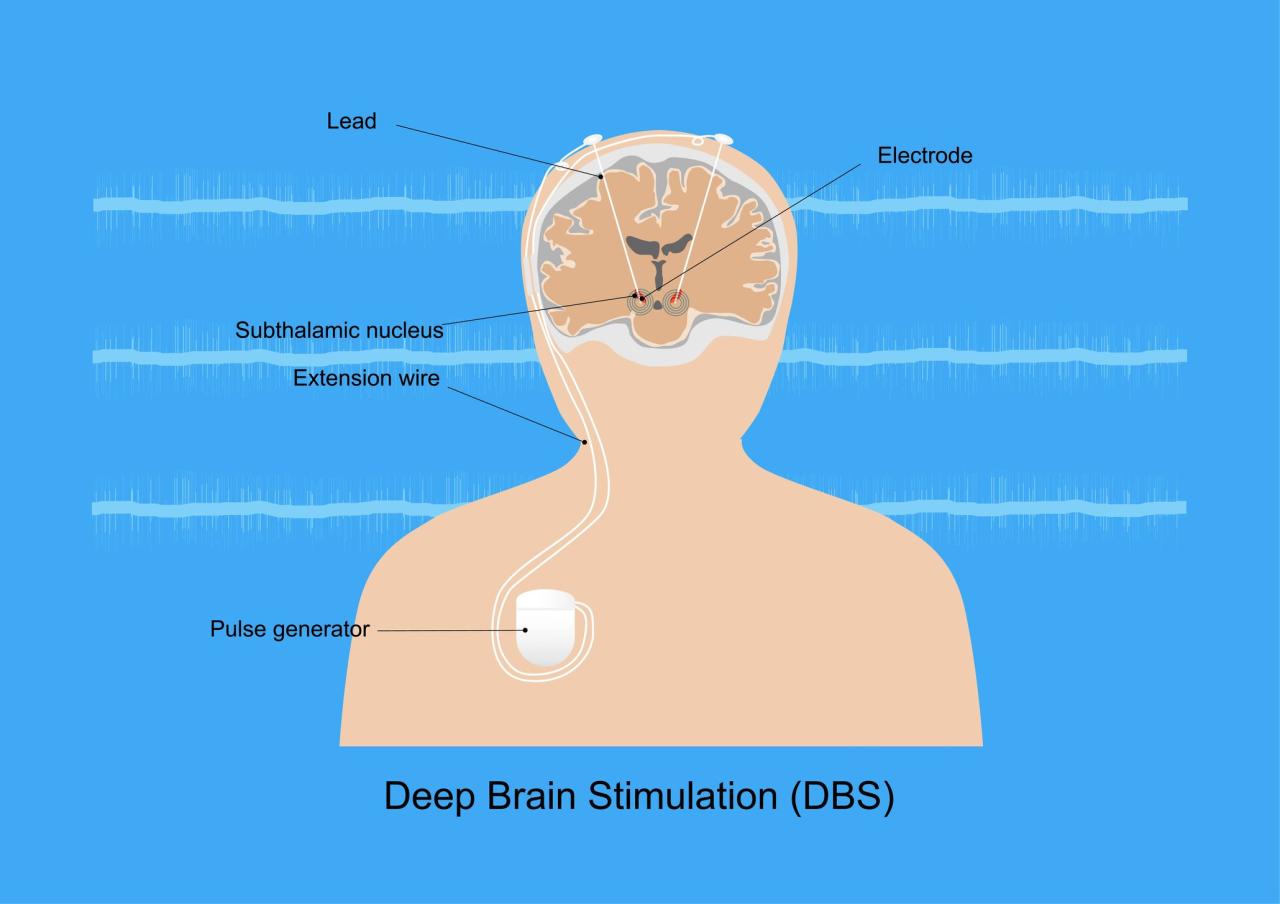
Deep Brain Stimulation (DBS)
Deep brain stimulation involves implanting a small device, similar to a pacemaker, into the brain. This device delivers electrical impulses to specific brain regions, effectively interrupting the abnormal signals causing tremors and other Parkinson’s symptoms. The targeted brain regions are chosen based on their involvement in the disease’s pathophysiology. The procedure allows for precise modulation of neuronal activity, often leading to significant symptom improvement.
Targeted Brain Regions
The selection of specific brain regions for surgical intervention is crucial. Subthalamic nucleus (STN) and globus pallidus internus (GPi) are frequently targeted in DBS procedures for Parkinson’s. The STN is implicated in motor control circuits, while the GPi plays a critical role in regulating movement. The choice of target depends on factors like the individual’s specific symptoms, the effectiveness of previous treatments, and the overall clinical picture.
Types of Deep Brain Stimulation Devices
Several types of DBS devices are available, differing in their features and functionalities. These devices deliver electrical pulses with adjustable parameters, allowing for fine-tuning of stimulation to optimize therapeutic outcomes. Differences include battery life, programming capabilities, and the range of stimulation parameters. Specific device selection is often tailored to the individual patient’s needs and preferences.
Brain surgery can surprisingly stop Parkinson’s disease tremors, a truly remarkable advancement in medical science. However, finding the perfect mattress, like choosing between a Purple Hybrid and a Casper, can be just as important for a good night’s sleep, which directly impacts overall well-being, as critical as those medical breakthroughs are. Ultimately, whether it’s a surgical procedure or a new mattress, the focus remains on improving quality of life for those affected by these challenges.
Finding the right comfort and support, such as comparing purple hybrid vs casper mattress options, can have a significant impact on daily life. So, while brain surgery is a powerful tool, a supportive mattress can be an equally important part of the treatment journey.
Deep Brain Stimulation Surgery Procedure
A typical deep brain stimulation surgery involves several key steps. First, a precise neurosurgical mapping of the targeted brain regions is performed. Then, the neurosurgeon creates a small opening in the skull to access the targeted area. Next, specialized electrodes are implanted into the selected region. Finally, a small pulse generator, often placed under the collarbone, is connected to the electrodes.
The system is then programmed to deliver targeted electrical pulses, adjusting the stimulation parameters as needed.
Surgical Techniques and Risks
| Surgical Technique | Rationale | Potential Risks |
|---|---|---|
| Deep Brain Stimulation (DBS) | Precisely targets brain regions associated with tremors, improving motor control. | Infection, bleeding, stroke, device malfunction, lead displacement, and stimulation-related side effects (e.g., dyskinesia). |
| Lesioning (e.g., Pallidotomy) | Damages specific brain areas to disrupt abnormal pathways. | Stroke, cognitive impairment, and speech problems. |
The Role of Brain Surgery in Parkinson’s Tremor Control
Brain surgery, a complex and potentially life-altering procedure, plays a crucial role in managing Parkinson’s disease symptoms, including tremors. While medication remains the primary treatment approach, surgical interventions offer a viable option for individuals who do not adequately respond to medications or experience intolerable side effects. This exploration delves into the effectiveness, benefits, limitations, and long-term outcomes of surgical procedures for Parkinson’s tremors.Surgical interventions for Parkinson’s tremors aim to reduce abnormal brain activity contributing to the tremors.
This is achieved by targeting specific brain regions associated with the tremors, either by destroying or stimulating these areas. The choice of surgical technique depends on individual factors, including the severity of symptoms, the response to medication, and overall health.
Effectiveness of Brain Surgery in Reducing Parkinson’s Tremors
Surgical procedures, like deep brain stimulation (DBS) and lesioning, have shown varying degrees of success in reducing Parkinson’s tremors. The effectiveness is highly individualized, depending on the patient’s specific condition and the surgical approach. Studies have demonstrated that, for some individuals, surgical interventions can significantly lessen tremor severity, improving their quality of life. However, it’s important to understand that not all patients experience the same level of improvement.
Potential Benefits and Limitations of Surgical Interventions
Surgical procedures for Parkinson’s tremor management offer potential benefits, including significant reduction in tremor severity and improved motor function. However, these procedures also carry limitations. The most significant benefit is the potential for substantial improvement in quality of life for those with debilitating tremors. However, surgical interventions involve risks, including potential complications such as infections, bleeding, and stroke.
The decision to undergo surgery must carefully weigh these potential benefits against the risks. Furthermore, the effectiveness of surgery can vary significantly between individuals, and not all patients experience the anticipated outcomes.
Comparison of Surgical Techniques in Managing Tremors
Different surgical techniques are employed to manage Parkinson’s tremors, each with its own characteristics. Deep brain stimulation (DBS) involves implanting electrodes in specific brain regions, which deliver electrical impulses to regulate abnormal brain activity. Lesioning, on the other hand, involves destroying targeted brain tissue to reduce abnormal signals.
Long-Term Outcomes and Potential Complications
Long-term outcomes of brain surgery for Parkinson’s tremors can be variable. Positive outcomes include sustained reduction in tremor severity, improved motor function, and an enhanced quality of life. However, potential complications include infection, bleeding, stroke, and device malfunction. The risk of these complications varies based on individual factors and surgical technique. Proper post-operative care and ongoing monitoring are essential to manage potential complications and ensure optimal outcomes.
Table Comparing Surgical Techniques
| Surgical Technique | Success Rate (Estimated) | Recovery Time (Estimated) | Potential Complications |
|---|---|---|---|
| Deep Brain Stimulation (DBS) | 60-80% effective in reducing tremors | Several weeks to months | Infection, bleeding, stroke, device malfunction |
| Lesioning (e.g., Pallidotomy) | 40-70% effective in reducing tremors | Several weeks to months | Infection, bleeding, stroke, unintended damage to surrounding areas |
Note: Success rates and recovery times are estimates and can vary based on individual patient factors.
While brain surgery can seemingly stop Parkinson’s disease tremors, it’s important to remember that a healthy diet plays a crucial role in overall well-being. Trying a delicious, low-carb alternative like the tabay atkins tofu tacos recipe can be a fun way to explore flavorful options. After all, focusing on balanced nutrition can complement any medical treatment, and help manage symptoms of Parkinson’s disease.
The surgery still remains a valuable option for some, though.
Pre- and Post-Surgical Considerations

Brain surgery for Parkinson’s disease offers a potential path to alleviate debilitating tremors and other symptoms. However, meticulous pre-surgical evaluation and a robust post-operative care plan are crucial for successful outcomes. This section details the critical steps involved in navigating this complex process.Thorough assessment of the patient’s medical history and current condition is paramount to optimizing the surgical approach and minimizing potential complications.
The pre- and post-operative phases necessitate a multidisciplinary approach, involving neurologists, neurosurgeons, anesthesiologists, and physical therapists, all working collaboratively to ensure optimal patient care.
Pre-Surgical Evaluation Process
The pre-surgical evaluation process is a comprehensive investigation into the patient’s suitability for deep brain stimulation (DBS) surgery. This meticulous assessment aims to identify potential risks and ensure the procedure aligns with the patient’s individual needs.This involves a series of crucial medical assessments and diagnostic tests. The goal is to understand the patient’s specific neurological condition, potential responses to treatment, and identify any underlying health issues that could impact the surgical process or recovery.
- Neurological Examination: A detailed neurological examination assesses the severity and type of Parkinson’s symptoms, including tremor, rigidity, bradykinesia, and postural instability. This evaluation also helps in identifying any co-existing neurological conditions that might affect the surgery or recovery.
- Medical History Review: A thorough review of the patient’s medical history, including previous illnesses, surgeries, allergies, and medications, is essential. This helps in identifying potential complications and in tailoring the surgical approach to the patient’s unique medical profile. For instance, a patient with a history of bleeding disorders might require special precautions during the procedure.
- Imaging Studies: Advanced imaging techniques, such as MRI and CT scans, are employed to create detailed images of the brain. These images provide vital information about the brain’s structure, identifying potential anatomical variations or underlying conditions that might influence the surgical plan. These images help the surgical team plan the precise placement of electrodes for optimal stimulation.
- Neuropsychological Testing: Neuropsychological evaluations assess cognitive functions, memory, and personality. This information is vital for understanding how the patient might be affected by the surgery and recovery process, particularly regarding cognitive changes, which are sometimes reported in patients undergoing DBS.
Post-Operative Care and Rehabilitation
The post-operative period necessitates a structured rehabilitation program tailored to the individual patient. Recovery is a multifaceted process involving physical, occupational, and speech therapies, aimed at regaining lost functions and adapting to the new neurological state.
- Initial Monitoring: Close monitoring of vital signs, neurological status, and surgical site is crucial in the immediate post-operative period. This vigilance ensures the detection and prompt management of any complications, such as bleeding or infection.
- Physical Therapy: Physical therapy plays a pivotal role in restoring mobility and strength. Exercises and therapies are tailored to address the patient’s specific needs and limitations. For instance, regaining balance and coordination, and reducing stiffness, are key goals of physical therapy.
- Occupational Therapy: Occupational therapy focuses on improving daily living skills. This includes activities that enhance independence in tasks such as dressing, eating, and bathing. Occupational therapy addresses the practical challenges that patients might face in performing everyday activities after the surgery.
- Speech Therapy: Speech therapy helps patients regain clear communication. It addresses speech problems that may arise after the procedure, especially when it involves communication-related regions of the brain.
Patient’s Role in Recovery
Patient participation is paramount in the recovery process. Active engagement and adherence to the prescribed treatment plan significantly contribute to positive outcomes.
- Adherence to Post-operative Instructions: Strictly following post-operative instructions, such as medication schedules and activity restrictions, is crucial. Adherence to these guidelines is vital to ensure a smooth and safe recovery. Following instructions, like maintaining a healthy diet and getting adequate rest, will help the body heal and reduce potential complications.
- Active Participation in Therapy: Patients are encouraged to actively participate in physical, occupational, and speech therapies. This active involvement is essential for achieving optimal recovery and regaining lost functions. Regular attendance and engagement in therapy exercises are key to success.
- Open Communication with Healthcare Professionals: Open and honest communication with healthcare professionals is essential. Patients should promptly report any concerns or discomfort. This proactive approach helps ensure the timely identification and management of any potential complications. This includes discussing any side effects or changes in symptoms with the team.
Pre- and Post-Operative Guidelines
| Category | Pre-Operative Guidelines | Post-Operative Guidelines |
|---|---|---|
| Medical Assessments | Comprehensive medical history review, neurological examination, imaging studies, neuropsychological testing. | Regular monitoring of vital signs, neurological status, and surgical site. |
| Therapy | Evaluation of current functional status to determine needs and plan for post-operative therapies. | Structured physical, occupational, and speech therapy sessions to enhance recovery. |
| Lifestyle | Medication adherence, healthy diet, adequate sleep. | Adherence to medication schedules, activity restrictions, and follow-up appointments. |
Illustrative Case Studies
Navigating the complexities of Parkinson’s disease often requires personalized approaches. Surgical interventions, while significant, are not a one-size-fits-all solution. Understanding how these procedures impact individual patients provides valuable insights into their effectiveness and limitations. Success stories, paired with detailed analyses of the surgical strategies, offer a richer understanding of the possibilities and challenges.
Case Study 1: Deep Brain Stimulation (DBS) for Severe Tremors
This case highlights the efficacy of DBS in managing debilitating tremors. Patient A, a 65-year-old, presented with severe resting and action tremors significantly impacting their daily life. These tremors made simple tasks like eating and writing nearly impossible.
- Pre-Surgical Symptoms: Patient A experienced significant difficulty with fine motor skills, frequently dropping utensils, and struggling with speech clarity due to the tremor’s effect on vocal cords. Their quality of life was drastically reduced.
- Surgical Approach: The surgical team targeted the thalamus using a specialized DBS system. Micro-electrodes were precisely implanted to stimulate the thalamus, interfering with the neural pathways responsible for the tremors. The procedure involved precise anatomical localization of the target region to minimize risk.
- Post-Surgical Outcomes: Following the procedure, Patient A experienced a remarkable reduction in tremors. The ability to perform everyday tasks, like eating and writing, was restored, leading to a noticeable improvement in their quality of life. They reported a significant increase in independence and a reduction in anxiety. Regular follow-up sessions adjusted the stimulation parameters to optimize tremor control.
Long-term outcomes showed sustained effectiveness of the DBS system.
Case Study 2: Lesioning Procedures for Specific Tremor Patterns, Brain surgery stops parkinsons disease tremors
This section describes a case utilizing a different surgical technique, highlighting its targeted approach.
- Pre-Surgical Symptoms: Patient B, a 48-year-old, experienced a specific pattern of postural tremors. The tremors significantly affected their ability to maintain balance, leading to frequent falls. They required assistance with mobility.
- Surgical Approach: A focused lesioning procedure was performed. A specialized instrument was used to create a controlled lesion in a specific region of the brain responsible for the tremors. This targeted approach was selected due to the patient’s specific tremor characteristics. The procedure was guided by advanced imaging and careful neurosurgical planning.
- Post-Surgical Outcomes: Post-surgery, Patient B exhibited a significant improvement in balance and reduced frequency of falls. While the tremors were not completely eliminated, the severity and frequency were substantially reduced. The patient was able to resume their activities with improved independence, and a more optimistic outlook. The procedure’s targeted approach minimized the potential for unwanted side effects.
Ethical Considerations
Brain surgery for Parkinson’s disease, while offering potential benefits, raises crucial ethical considerations. Navigating these complex issues requires a thoughtful and nuanced approach that prioritizes patient well-being, autonomy, and societal responsibility. A comprehensive understanding of these ethical implications is essential for responsible implementation of this procedure.
Informed Consent and Decision-Making
Patients undergoing brain surgery for Parkinson’s disease have a fundamental right to informed consent. This necessitates a thorough explanation of the procedure, its potential risks and benefits, alternative treatments, and the long-term implications. The patient’s understanding of the information presented is crucial. Clinicians must ensure the patient comprehends the complex medical information and is capable of making an autonomous decision.
This includes assessing the patient’s cognitive capacity and emotional state, ensuring they are not unduly influenced by external pressures.
Risks and Benefits
The decision-making process regarding brain surgery must carefully weigh the potential benefits against the inherent risks. Deep brain stimulation, a common procedure, offers the possibility of significantly reducing tremors and other Parkinson’s symptoms. However, it is not without risks. Potential complications include infection, bleeding, stroke, and adverse effects on cognitive function. Furthermore, the long-term effectiveness and impact on the patient’s quality of life must be considered.
Detailed pre-surgical discussions and realistic expectations regarding the outcome are vital. Patients should be made aware that symptom improvement is not guaranteed and that some patients may experience unforeseen complications.
Societal Implications
The availability of brain surgery for Parkinson’s raises questions about equitable access to this technology. Considerations of cost, insurance coverage, and geographic limitations need to be addressed. Furthermore, the potential for misuse or inappropriate application of the procedure requires vigilance. Ethical guidelines and regulatory oversight are essential to ensure that the procedure is used responsibly and ethically.
These factors must be carefully weighed against the benefits for the individual patient.
Key Ethical Principles
| Ethical Principle | Explanation |
|---|---|
| Autonomy | Respecting the patient’s right to make their own decisions about their treatment, free from coercion or undue influence. |
| Beneficence | Acting in the best interests of the patient, maximizing potential benefits and minimizing risks. |
| Non-maleficence | Minimizing harm to the patient and ensuring that the risks of the procedure are carefully considered and mitigated. |
| Justice | Ensuring equitable access to the procedure, considering factors such as socioeconomic status and geographical location. Avoiding discrimination in treatment. |
Future Directions and Research
The journey to better manage Parkinson’s disease, particularly its debilitating tremors, is far from over. Ongoing research and development promise exciting advancements in brain surgery techniques, novel therapies, and a deeper understanding of the neurological mechanisms at play. This exploration into future directions will shed light on potential breakthroughs that could significantly improve the lives of those affected.Current treatments, while effective for many, have limitations.
Future research aims to refine existing approaches and discover entirely new strategies to alleviate symptoms and potentially slow or even reverse the progression of the disease. This includes a critical focus on personalized treatment plans tailored to the individual needs of each patient.
Ongoing Research and Development Efforts
A multitude of research groups worldwide are dedicated to advancing the understanding and treatment of Parkinson’s disease. This involves investigating the underlying causes, developing more effective therapies, and improving the precision and safety of surgical interventions. Clinical trials are constantly evaluating new drug candidates and surgical procedures, providing valuable data on their efficacy and side effects.
Potential Advancements in Brain Surgery Techniques
Technological advancements are driving innovations in brain surgery. Minimally invasive techniques, such as focused ultrasound and deep brain stimulation with improved targeting systems, are showing promising results. Researchers are exploring ways to further refine these methods, reducing invasiveness and improving long-term outcomes. The development of more sophisticated imaging techniques allows for a more precise identification of target areas in the brain, further enhancing the precision of surgical procedures.
Emerging Therapies
Emerging therapies offer potential complements or replacements to existing treatments. These include gene therapy approaches aimed at correcting genetic defects associated with Parkinson’s and stem cell therapies designed to replace damaged brain cells. Experimental therapies, such as those employing neuroprotective agents, aim to prevent or slow the progression of the disease, a significant advancement beyond current symptom management.
Promising Areas of Research Related to Parkinson’s Tremors
Research is actively exploring novel approaches to control tremors, specifically targeting the neural circuits involved. This includes investigating the use of non-invasive brain stimulation techniques, such as transcranial magnetic stimulation, to modulate neural activity and reduce tremor severity. Additionally, investigations into the role of specific neurotransmitters in tremor generation are providing insights into potential drug targets for more targeted tremor control.
Table of Current and Future Research Areas in Parkinson’s Treatment
| Research Area | Current Status | Future Directions |
|---|---|---|
| Deep Brain Stimulation (DBS) | Established as a significant treatment option | Development of more precise targeting methods; integration with advanced imaging; personalized stimulation protocols. |
| Focused Ultrasound | Showing promise in reducing invasiveness and improving targeting | Further refinements to reduce side effects and improve treatment efficacy; applications in various brain regions. |
| Gene Therapy | Early-stage research with some promising preclinical results | Development of safe and effective vectors for gene delivery; targeting specific genes implicated in Parkinson’s. |
| Stem Cell Therapies | Clinical trials underway | Improved differentiation and integration of transplanted cells; development of more efficient delivery methods. |
| Neuroprotective Agents | Ongoing research | Identification of novel compounds with neuroprotective properties; development of targeted drug delivery systems. |
| Non-invasive Brain Stimulation | Emerging as a potential complementary therapy | Refinement of techniques to improve targeting; optimization of stimulation parameters for tremor control. |
Final Conclusion
In conclusion, brain surgery, particularly deep brain stimulation, emerges as a promising avenue for managing Parkinson’s tremors. While surgical interventions carry potential risks, the positive outcomes for many patients underscore the potential for significant improvements in quality of life. Further research and development are crucial for refining surgical techniques and enhancing long-term outcomes. The ethical considerations surrounding such procedures must also be carefully addressed to ensure responsible and compassionate application.
This exploration highlights the intricate interplay between medical science and patient well-being in addressing the complex challenges of Parkinson’s.
