Signs your migraine treatment isnt working – Signs your migraine treatment isn’t working. Understanding these signs is crucial for adjusting your treatment plan and achieving better migraine management. This post explores common symptoms, treatment adherence issues, medication effectiveness, potential underlying conditions, lifestyle factors, and the importance of seeking professional guidance.
We’ll delve into the specifics of recognizing when your current migraine treatment isn’t producing the desired results. From persistent symptoms to medication side effects and potential underlying medical issues, we’ll provide practical insights and actionable strategies to help you navigate this complex journey.
Identifying Symptoms of Ineffective Treatment
Understanding if your migraine treatment is working as intended is crucial for managing your condition effectively. This involves recognizing subtle changes in your symptoms, pain patterns, and triggers, which can signal a need for adjustments in your treatment plan. Monitoring these aspects allows for proactive communication with your healthcare provider, leading to improved symptom management.Migraines are complex, and what works for one person may not work for another.
Therefore, careful observation of your response to treatment is key. Regular documentation of your experiences can help you and your doctor identify patterns and pinpoint areas where adjustments are necessary.
Persistent Migraine Symptoms Despite Treatment
Recognizing that your migraine symptoms persist or worsen despite treatment is a vital step towards effective management. Some common symptoms that might indicate treatment ineffectiveness include:
- Headaches that are more frequent than usual, lasting longer, or occurring more intensely.
- A change in the location or type of headache pain. For instance, a shift from a throbbing pain to a sharp, stabbing sensation.
- The emergence of new, previously unknown symptoms accompanying your headaches.
- Increased sensitivity to light, sound, or smells.
- Difficulty concentrating or experiencing confusion.
Escalating or Worsening Pain Patterns
Monitoring how your migraine pain changes over time is essential for assessing treatment effectiveness. Patterns to watch for include:
- Increased duration of migraine attacks.
- Rise in the intensity of pain, making it harder to manage daily activities.
- More frequent migraine attacks with shorter intervals between them.
- Emergence of new migraine attack triggers, suggesting a disconnect between the treatment and the underlying cause.
- A shift in the location of the pain from the typical spot, potentially indicating a new trigger or underlying issue.
Documenting Migraine Frequency and Intensity
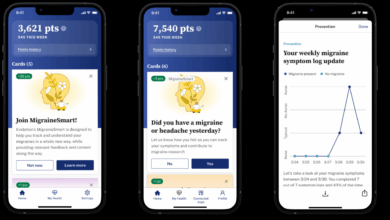
Detailed records of your migraine episodes provide valuable insights for assessing treatment effectiveness.
- Keeping a migraine diary is highly recommended. Record the date, time, duration, intensity (using a scale of 1-10), and location of each migraine attack. Also, note any accompanying symptoms.
- Using a pain scale can help quantify the intensity of your pain, facilitating communication with your healthcare provider.
- Tracking the frequency of attacks (e.g., number of attacks per week or month) helps identify patterns and trends.
Migraine Triggers and Treatment Failure, Signs your migraine treatment isnt working
Understanding your migraine triggers can be vital in determining if your current treatment approach is suitable. There is a potential link between identified triggers and treatment failure.
- Identifying triggers, such as stress, caffeine withdrawal, specific foods, or environmental factors, is crucial for effective migraine management. If you notice a sudden increase in migraine episodes after a change in your diet or environment, this could indicate a potential connection.
- Consider whether the treatment is effectively addressing the triggers. For example, if your migraines are frequently triggered by stress, your treatment plan should incorporate stress-reducing techniques.
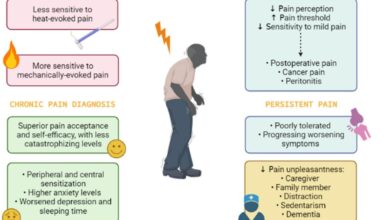
Physical Sensations and Treatment Ineffectiveness
Physical sensations beyond head pain can indicate treatment ineffectiveness. Pay attention to:
- Nausea or vomiting, which often accompany migraines and might persist despite treatment.
- Dizziness or vertigo, especially if new or worsening.
- Numbness or tingling in the face or extremities, if a new symptom.
- Changes in vision, such as blurred vision or double vision, which can indicate underlying issues.
Comparing Symptoms Before and After Treatment
A table can visually illustrate the difference in your migraine symptoms before and after initiating treatment.
| Symptom | Before Treatment | After Treatment |
|---|---|---|
| Frequency of attacks | 3-4 per week | 4-5 per week |
| Pain intensity (1-10) | 8 | 7 |
| Duration of attack | 4-6 hours | 4 hours |
| Accompanying symptoms | Nausea, photophobia | Nausea, photophobia, numbness |
Evaluating Treatment Adherence
Following your migraine treatment plan meticulously is crucial for effective management. Consistent adherence to prescribed protocols significantly impacts the success of your therapy. Understanding the factors that can hinder adherence allows you to proactively address potential obstacles and optimize your treatment outcomes. This proactive approach will lead to more predictable and manageable migraine experiences.Adherence to a migraine treatment plan is more than just taking medication; it encompasses understanding the specific instructions, adhering to the prescribed dosage, and maintaining a consistent schedule.
Feeling like your migraine treatment isn’t cutting it? A few telltale signs might indicate it’s time to adjust your approach. Increased frequency or severity of attacks, or maybe the pain just isn’t responding as expected, could be a sign you need to explore other options. Interestingly, Obamacare’s impact on healthcare access, especially in rural areas, has been quite significant, and Obamacare helped keep rural hospitals open , highlighting the importance of comprehensive care for everyone, not just in city centers.
Ultimately, if your migraine treatment isn’t yielding the desired results, it’s crucial to consult your doctor to pinpoint the root cause and explore alternative solutions.
A proactive approach, including understanding potential barriers to adherence, and implementing strategies to overcome them, will ultimately improve your overall migraine management.
Importance of Following Prescribed Treatment Protocols
Adherence to the prescribed treatment protocol is paramount for managing migraine effectively. This involves not only taking medications as directed but also incorporating lifestyle adjustments recommended by your healthcare provider. Inconsistency in treatment can lead to ineffective symptom control and potentially more frequent or severe migraines. This is due to the medication not having enough time to build up to an effective level, or in some cases, the body developing a resistance to the medication.
Consistency is key.
Potential Reasons for Non-Adherence to Treatment Plans
Numerous factors can contribute to non-adherence to treatment plans. Understanding these factors can help identify potential obstacles and develop strategies for improvement.
- Medication side effects: Unpleasant side effects, such as nausea, dizziness, or fatigue, can discourage patients from continuing their medication regimen. This is particularly true if the side effects are severe or prolonged. For instance, a patient experiencing severe nausea after taking a migraine preventative might be less likely to take the medication consistently.
- Cost of medications: High medication costs can create financial barriers, leading patients to skip doses or discontinue treatment altogether. In this case, exploring cost-saving options, such as generic alternatives or patient assistance programs, can be helpful.
- Lack of understanding of the treatment plan: Patients may not fully comprehend the importance of the treatment plan or the long-term benefits of consistent adherence. Clearly explaining the treatment plan and its importance is critical.
- Lifestyle factors: Busy schedules, stress, and other lifestyle demands can make it difficult to remember or prioritize medication intake. For instance, a patient with a demanding work schedule may find it challenging to remember to take their medication at the designated times.
- Poor communication between patient and healthcare provider: A lack of clear communication about treatment expectations, side effects, or potential adjustments can lead to confusion and decreased adherence. Clear and regular communication with your doctor is essential.
Common Mistakes Regarding Medication Timing, Dosage, or Frequency
Inconsistent medication intake can significantly impact treatment effectiveness. Common mistakes include skipping doses, taking medication at irregular times, or adjusting dosages without consulting a healthcare professional.
- Skipping doses: Even one missed dose can disrupt the medication’s effectiveness, especially for preventive medications. This can lead to more frequent and intense migraines.
- Taking medication at irregular times: Maintaining a consistent schedule for medication intake is crucial for the body to adapt to the treatment and build up an effective concentration of the medication.
- Adjusting dosages without professional guidance: Altering medication dosages without consulting a healthcare provider can be dangerous and ineffective. Dosage adjustments should always be made under medical supervision.
Strategies to Improve Medication Adherence
Implementing strategies to improve medication adherence can significantly enhance treatment outcomes. These strategies include simplifying medication regimens, using reminders, and building support networks.
- Simplifying medication regimens: A simpler regimen with fewer medications or doses taken at more manageable intervals can improve adherence. Consider combining medications or using a single-dose formulation whenever possible.
- Using reminders: Utilizing medication reminders, such as pill organizers, alarms, or mobile apps, can help patients remember to take their medication on schedule.
- Building support networks: Connecting with support groups or sharing experiences with others facing similar challenges can provide motivation and encouragement. Consider joining online or in-person support groups to share your experiences and connect with others.
Treatment Options and Potential Side Effects
The following table Artikels various treatment options and their potential side effects. It is essential to discuss these potential side effects with your healthcare provider.
| Treatment Option | Potential Side Effects |
|---|---|
| Triptans | Nausea, tingling, dizziness, or feelings of pressure in the head |
| NSAIDs | Gastrointestinal upset, stomach pain, or kidney problems |
| CGRP inhibitors | Injection site reactions, flu-like symptoms, or allergic reactions |
| Botox | Injection site pain or bruising |
Comparison of Administration Methods
Different administration methods for migraine medications can influence their effectiveness and patient adherence. Oral medications are often convenient, but their absorption and effectiveness can vary.
- Oral medications: These medications are generally easy to administer but can have variable absorption rates and require patients to remember to take them at specific times.
- Injectable medications: Injectable medications, such as CGRP inhibitors, can offer faster relief but require a healthcare provider’s administration. This may be inconvenient for some patients.
- Nasal sprays: Nasal sprays offer a localized delivery of medication and can provide rapid relief for acute migraines.
Assessing the Effectiveness of Medication Types
Migraine treatment often involves a personalized approach, and understanding how different medication types work, their potential side effects, and interactions is crucial for successful management. Choosing the right medication and dosage is a key aspect of effective migraine treatment. This section delves into the specifics of various migraine medications, helping you navigate the complexities of this challenging condition.Migraine medications are broadly categorized into preventative and abortive types, each targeting different stages of the migraine cycle.
Figuring out if your migraine treatment is hitting the mark can be tricky. Sometimes, despite sticking to your plan, you might notice symptoms persisting or even worsening. This could be a sign that the current approach isn’t working. Interestingly, some common cancer screenings, like those used to detect rheumatoid arthritis, sometimes have surprising applications in diagnosing other conditions.
For example, the approach used in common cancer screening used to detect rheumatoid arthritis might reveal subtle indicators that your migraine treatment isn’t effectively addressing the root cause of your discomfort. This could point to the need for a different treatment strategy or a more in-depth evaluation by your doctor.
Understanding their distinct mechanisms of action can greatly assist in determining the most appropriate course of treatment.
Preventative Medications
Preventative medications aim to reduce the frequency and severity of migraine attacks over time. These medications often need to be taken consistently for several weeks to build up their effect.
- Tricyclic antidepressants: These medications can help reduce the frequency of migraine attacks by influencing neurotransmitter levels. Common side effects include drowsiness, dry mouth, and constipation.
- Beta-blockers: Beta-blockers can help prevent migraine attacks by blocking the effects of stress hormones on the blood vessels in the brain. Potential side effects include fatigue, dizziness, and slow heart rate.
- Calcium channel blockers: These medications can help prevent migraine attacks by reducing the dilation of blood vessels. Common side effects include dizziness, swelling, and headache.
- Anti-epileptic drugs: Certain anti-epileptic drugs, like topiramate, can reduce the frequency of migraine attacks by modifying neuronal activity. Possible side effects include tingling sensations, dizziness, and difficulty concentrating.
- CGRP inhibitors: These newer medications target calcitonin gene-related peptide (CGRP), a protein implicated in migraine pain. Side effects can include injection site reactions, nausea, and fatigue.
Abortive Medications
Abortive medications are taken during a migraine attack to stop or lessen its intensity. They typically work faster than preventative medications.
- Triptans: Triptans are a common type of abortive medication that constricts blood vessels in the brain. Common side effects include chest tightness, tingling sensations, and nausea. Specific triptan use should be tailored based on individual patient factors, like history of cardiovascular issues.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs like ibuprofen or naproxen can reduce inflammation and pain associated with migraine attacks. Common side effects include stomach upset and gastrointestinal discomfort. Individuals with pre-existing stomach ulcers or conditions should carefully consider their use.
- Ergotamine: Ergotamine medications can help constrict blood vessels, but they should be used with caution due to potential side effects. These side effects can range from nausea to numbness and can be exacerbated by concomitant use of other medications.
Medication Interactions
Many medications can interact with migraine medications, potentially altering their effectiveness or causing adverse effects. Patients should always inform their doctor about all medications they are taking, including over-the-counter drugs and supplements.
Factors Influencing Medication Effectiveness
Individual responses to migraine medications vary widely. Factors that may influence a medication’s effectiveness include:
- Individual sensitivity: Some people may be more sensitive to certain medications, leading to a stronger reaction or decreased efficacy.
- Medication adherence: Regular and consistent use of prescribed medications is essential for optimal results.
- Underlying health conditions: Existing medical conditions may affect how a medication is metabolized or interact with other drugs.
- Migraine triggers: Identifying and managing migraine triggers can help improve medication effectiveness.
- Dosage and timing: Proper dosage and timing of medication administration can significantly impact efficacy.
Medication Resistance or Inefficacy
Medication resistance or inefficacy can occur for various reasons, including:
- Incorrect diagnosis: An inaccurate diagnosis may lead to the inappropriate selection of medications.
- Underlying medical conditions: Unidentified or untreated medical conditions can affect the effectiveness of treatment.
- Medication interactions: Concurrent medications can interfere with the effectiveness of migraine treatments.
- Individual variability: Responses to medications can differ significantly between individuals.
Comparison of Migraine Medication Classes
| Medication Class | Mechanism of Action | Efficacy | Common Side Effects |
|---|---|---|---|
| Triptans | Constricts blood vessels | High | Nausea, chest tightness, tingling |
| NSAIDs | Reduces inflammation | Moderate | Stomach upset, gastrointestinal discomfort |
| CGRP inhibitors | Targets CGRP | High | Injection site reactions, nausea, fatigue |
Considering Underlying Medical Conditions

Sometimes, a migraine’s stubbornness isn’t due to a treatment failing, but rather to an underlying medical condition. These hidden issues can significantly impact how your body responds to migraine medications, making it crucial to consider them in your treatment plan. Ignoring potential underlying conditions can delay accurate diagnoses and optimal management of your migraines.Understanding the connection between underlying medical conditions and migraine treatment outcomes is essential.
Figuring out if your migraine treatment’s not cutting it can be tricky. Maybe you’re noticing more frequent headaches despite sticking to your routine. Or perhaps you’re finding yourself reaching for extra pain relievers more often. Interestingly, research suggests that the comforting presence of a canine companion can positively impact sleep quality, as detailed in this fascinating study on why women sleep better with dogs.
Either way, if you’re noticing these patterns, it might be a good time to chat with your doctor about adjusting your treatment plan. Perhaps a different approach or medication could be the solution you’re looking for.
A variety of health problems can influence how your body reacts to medications, potentially causing the treatment to be ineffective. This is why a thorough evaluation by a healthcare professional is essential to identify any hidden factors that might be influencing your migraines.
Relationship Between Underlying Conditions and Treatment Outcomes
Migraine treatment effectiveness can be significantly affected by concurrent medical conditions. These conditions can interfere with the body’s ability to metabolize or utilize medications, leading to suboptimal results. For instance, a thyroid imbalance might alter the body’s response to triptans, resulting in diminished pain relief. Similarly, certain digestive issues can impact the absorption of oral medications, impacting their effectiveness.
Examples of Other Health Issues Impacting Migraine Responses
Several medical conditions can influence migraine responses to treatment. Gastrointestinal issues, such as inflammatory bowel disease or irritable bowel syndrome, can affect medication absorption, potentially diminishing the effectiveness of oral migraine medications. Similarly, hormonal fluctuations, like those experienced during menopause or with polycystic ovary syndrome, can trigger or exacerbate migraine attacks, making it difficult to predict treatment outcomes.
Blood pressure disorders can also influence the efficacy of certain medications.
Potential Diagnostic Tests
Identifying underlying medical conditions necessitates a thorough evaluation. Diagnostic tests may include blood tests to assess hormone levels, thyroid function, or other potential imbalances. Imaging studies, such as MRIs or CT scans, might be used to identify structural abnormalities or other potential issues within the brain or other relevant areas. Neurological evaluations can help rule out other neurological disorders that might mimic migraine symptoms.
Communicating with a Healthcare Provider
Open communication with your healthcare provider is crucial when suspecting an underlying condition. Be prepared to discuss any other health issues you are experiencing, including symptoms, treatment history, and any medications you are currently taking. Providing detailed information will allow your provider to thoroughly assess your situation and make informed decisions regarding further testing or treatment.
Table of Potential Medical Conditions Affecting Migraine Treatment Response
| Potential Medical Condition | Possible Impact on Migraine Treatment |
|---|---|
| Thyroid disorders | May alter medication metabolism and efficacy. |
| Gastrointestinal issues (e.g., IBD, IBS) | May impact medication absorption, reducing effectiveness. |
| Hormonal imbalances (e.g., menopause, PCOS) | May trigger or exacerbate migraines, affecting treatment response. |
| Blood pressure disorders | May influence the efficacy of certain medications. |
| Neurological disorders (e.g., MS) | May mimic migraine symptoms, impacting treatment outcomes. |
| Head injuries | May contribute to migraine development or alter treatment response. |
Analyzing Lifestyle Factors

Migraines aren’t just a headache; they’re a multifaceted condition influenced by various aspects of daily life. Understanding how lifestyle choices affect migraine frequency and intensity is crucial for effective management. This section delves into the pivotal role of sleep, stress, diet, hydration, exercise, and the creation of a personalized prevention plan.Lifestyle factors significantly impact migraine experiences. The interplay between daily routines and migraine triggers can be complex, but recognizing these patterns can lead to targeted interventions and reduced migraine episodes.
Identifying and addressing these lifestyle elements can often be as effective as medication adjustments, or even more so, in some cases.
Sleep Hygiene and Migraine Frequency
Adequate sleep is essential for overall health, and its importance in migraine management cannot be overstated. Poor sleep quality and quantity are often linked to increased migraine risk and severity. Establishing a regular sleep schedule, creating a relaxing bedtime routine, and ensuring a dark, quiet, and cool sleep environment can contribute significantly to better sleep and reduced migraine episodes.
Stress Management and Migraine Triggers
Chronic stress is a well-known migraine trigger. Techniques like meditation, deep breathing exercises, yoga, and spending time in nature can help manage stress levels and potentially reduce migraine frequency. Learning to identify personal stress triggers and developing coping mechanisms is an integral part of migraine prevention.
Diet and Migraine Outcomes
Diet plays a crucial role in migraine management. Certain foods and beverages can act as triggers, while others may provide relief or prevention. Identifying individual dietary triggers is often a process of trial and error. Keeping a detailed food diary can help pinpoint problematic foods.
Dietary Changes for Migraine Improvement
Specific dietary changes can be beneficial for migraine sufferers. Reducing or eliminating caffeine, alcohol, aged cheeses, processed meats, and certain types of chocolate can be effective in some individuals. Increasing consumption of fruits, vegetables, and whole grains can promote overall well-being and potentially reduce migraine risk. Consider consulting a registered dietitian for personalized dietary recommendations.
Dehydration and Migraine Pain
Dehydration can be a significant migraine trigger. Maintaining adequate hydration throughout the day is crucial for preventing headaches. Carry a water bottle and sip water regularly, especially during physical activity or in hot weather. Pay attention to thirst cues and drink water proactively.
Regular Exercise and Physical Activity
Regular physical activity is a powerful tool in migraine prevention. Exercise releases endorphins, which have pain-relieving properties. Finding activities that are enjoyable and sustainable is key to maintaining a consistent exercise routine. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
Creating a Personalized Migraine Prevention Plan
Developing a personalized migraine prevention plan involves integrating lifestyle modifications into daily routines. Consider the specific triggers identified for each individual, and create a plan that addresses them effectively. This plan should include sleep hygiene strategies, stress management techniques, dietary modifications, hydration practices, and regular exercise. It’s important to track the effectiveness of these changes and adjust the plan as needed.
This plan is dynamic and should evolve based on individual experience and feedback.
Seeking Professional Guidance: Signs Your Migraine Treatment Isnt Working
Understanding that your migraine treatment isn’t working can be frustrating. Taking proactive steps to address the issue is crucial for managing your condition effectively. A collaborative approach with your healthcare provider is essential to achieving optimal results and improving your quality of life. This involves open communication, critical evaluation of the treatment plan, and a willingness to explore alternative strategies.
Questions to Ask Your Healthcare Provider
Effective communication with your healthcare provider is paramount. Asking insightful questions about your treatment’s effectiveness will facilitate a deeper understanding of the situation and pave the way for adjustments to the treatment plan. Here are some important questions to consider:
- How well is the current treatment addressing the frequency and intensity of my migraine attacks?
- Are there any potential side effects of the current medication that I should be aware of?
- Are there any other medications or treatment options that might be more effective for my specific type of migraine?
- Are there any lifestyle changes I can make to potentially reduce the triggers for my migraines?
- How long should I expect to see improvement with the current treatment plan?
- What are the potential reasons why the current treatment isn’t providing the desired results?
- Are there any diagnostic tests that could help determine the underlying cause of my migraines?
- How can I better track and document my migraine attacks to help us evaluate the treatment plan?
- What is the estimated success rate of different migraine treatment options, considering my individual circumstances?
Adjusting or Changing a Treatment Plan
Adjusting or changing a treatment plan is a collaborative process. It involves careful consideration of the current treatment’s effectiveness, potential side effects, and the possibility of alternative approaches. Your healthcare provider will guide you through the process, weighing the benefits and risks of each option.
- The adjustment process may involve altering the dosage, frequency, or type of medication.
- Adding a complementary therapy, such as biofeedback or mindfulness techniques, may also be considered.
- In some cases, discontinuing the current treatment and starting a new one may be necessary.
Importance of Open Communication
Maintaining open and honest communication with your healthcare team is crucial for effective migraine management. This includes sharing your concerns, experiences, and observations about your condition.
- Open communication fosters a collaborative relationship, enabling your healthcare provider to tailor the treatment plan to your specific needs.
- Honest feedback about the effectiveness of the treatment helps identify areas that need adjustment.
- Regular check-ins with your healthcare provider allow for timely adjustments to the treatment plan, ensuring optimal outcomes.
Benefits of Seeking a Second Opinion
A second opinion can provide valuable insights and alternative perspectives on your migraine treatment. It can also confirm the accuracy of the initial diagnosis and treatment plan.
- A second opinion can offer a fresh perspective and potentially uncover new avenues for effective treatment.
- This can lead to a more personalized and effective approach to migraine management.
- It can also build confidence in the chosen treatment plan and help manage expectations.
Managing Expectations
Understanding that migraine treatment outcomes can vary is crucial. While some individuals may experience significant improvement, others may require more time and experimentation to find a treatment plan that works best for them.
- Be prepared for a period of trial and error to find the most effective approach to your migraine.
- Managing expectations involves acknowledging that finding the optimal treatment may take time.
- Realistic expectations will contribute to a more positive experience and encourage continued engagement in the treatment process.
Resources for Finding Specialists
Accessing the expertise of specialists in migraine management is vital for comprehensive care. These specialists possess the knowledge and experience to address complex cases and provide tailored treatment plans.
| Resource | Description |
|---|---|
| Online Directories | Online resources can provide listings of specialists in your area. |
| Referral Services | Your primary care physician can offer referrals to specialists in migraine management. |
| Professional Associations | Professional organizations often have directories of certified migraine specialists. |
Closure
Ultimately, recognizing the signs your migraine treatment isn’t working is a vital step towards a more effective and personalized management strategy. By understanding the various contributing factors and actively communicating with your healthcare provider, you can work towards achieving better control over your migraine episodes and improving your overall well-being. Remember, consistency in monitoring your symptoms, open communication, and a collaborative approach with your healthcare team are key to navigating this process successfully.