Sputum direct fluorescent antibody dfa – Sputum direct fluorescent antibody (DFA) is a crucial diagnostic tool in identifying respiratory pathogens. This method allows for rapid detection of these pathogens, providing valuable information for clinicians to make timely and effective treatment decisions. The test utilizes fluorescent antibodies to pinpoint the presence of specific organisms in sputum samples, offering a quick and targeted approach to diagnosis. This comprehensive guide delves into the intricacies of sputum DFA, from specimen collection to result interpretation, empowering readers with a thorough understanding of this vital diagnostic procedure.
Understanding the intricacies of specimen collection and preparation, the underlying immunologic principles, and the interpretation of results is paramount. Proper handling and transportation of samples are crucial to maintain sample integrity and accuracy. The process involves precise steps to ensure reliable results and minimize potential errors. The detailed procedure, coupled with insights into the various applications, strengthens the understanding of this valuable diagnostic method.
Introduction to Sputum DFA
Sputum direct fluorescent antibody (DFA) testing is a crucial diagnostic tool in microbiology labs. It’s a rapid and efficient method for identifying specific microorganisms in clinical specimens, particularly in respiratory infections. This technique leverages the fluorescent properties of antibodies to visually detect the presence of targeted pathogens. Understanding the process and its clinical significance is important for healthcare professionals.The clinical significance of sputum DFA testing lies in its ability to rapidly diagnose infections, particularly those caused by pathogens like
- Legionella* species,
- Chlamydia pneumoniae*, and
- Mycobacterium tuberculosis*. A positive result often guides immediate treatment decisions, potentially preventing the progression of the infection and improving patient outcomes. Early diagnosis and targeted treatment are essential in managing respiratory illnesses effectively.
Specimen Requirements for DFA Testing
Appropriate specimen collection is critical for accurate DFA results. The quality and quantity of the sputum sample directly impact the test’s reliability. Ideally, the specimen should be collected in a sterile container, and the patient should be instructed to expectorate a fresh, deep cough sample. The sample should be transported promptly to the laboratory to prevent degradation of the pathogens.
A proper specimen collection technique and prompt transport to the lab ensure the integrity of the sample, increasing the reliability of the DFA test.
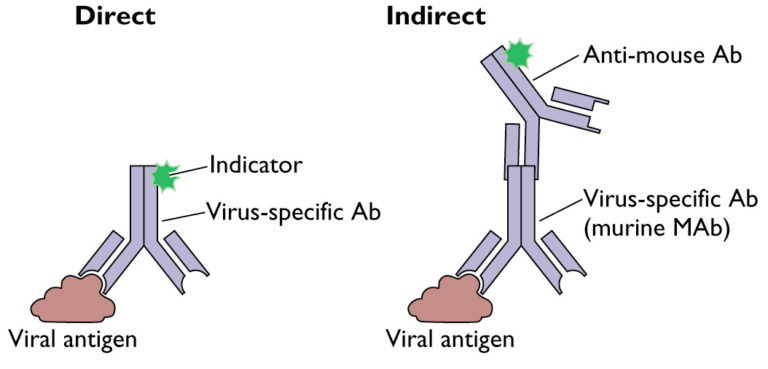
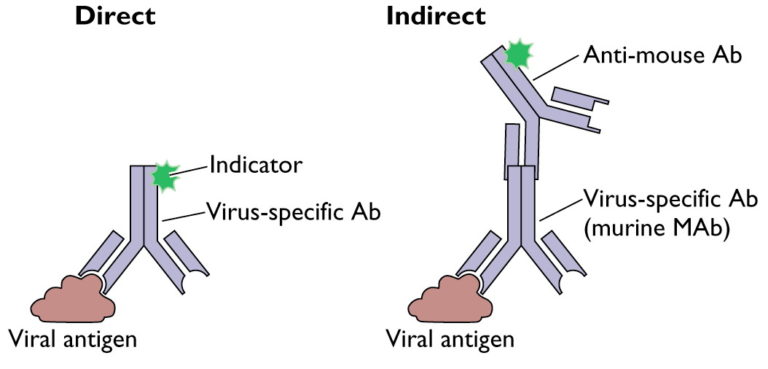
General Principles of Fluorescent Antibody Techniques
Fluorescent antibody techniques utilize the binding affinity of antibodies to specific antigens. The principle involves labeling antibodies with a fluorescent dye, such as fluorescein isothiocyanate (FITC). When the labeled antibody binds to the target antigen in the specimen, the fluorescence is emitted, allowing visualization under a fluorescence microscope. This specific binding and fluorescence allow for rapid identification of the target microorganism, differentiating it from other components in the specimen.
The intensity of the fluorescence correlates with the concentration of the target antigen.
Steps Involved in Performing a DFA Test
The process of performing a sputum DFA test involves several key steps. First, the sputum sample is prepared by staining and processing to optimize visualization. Next, the prepared specimen is exposed to specific fluorescently labeled antibodies that are designed to bind to the target pathogen. Following incubation, the slide is examined under a fluorescence microscope. The presence of fluorescence indicates the presence of the target pathogen.
The fluorescent signal is specific to the target pathogen and not to other components in the specimen. The intensity of the fluorescent signal can correlate with the pathogen load.
Interpretation of Results
A positive result indicates the presence of the target pathogen in the specimen. A negative result suggests the absence of the target pathogen in the specimen. It’s essential to interpret the results in conjunction with the patient’s clinical presentation and other diagnostic tests. The clinical context and additional laboratory tests are vital in determining the final diagnosis and guiding appropriate treatment strategies.
Specimen Collection and Preparation
Proper specimen collection and preparation are crucial for accurate results in direct fluorescent antibody (DFA) testing for sputum samples. Errors at this stage can significantly impact the reliability of the test outcome. This section details the critical steps to ensure a high-quality sample for reliable DFA results.
Sputum Collection Techniques
Collecting sputum for DFA requires careful attention to detail. Patients should be instructed to expectorate sputum directly into a sterile container. Ideally, the sample should be obtained in the morning, before the patient eats or drinks anything. This minimizes contamination from saliva and food particles. Thorough hand hygiene is paramount for the collector.
Sputum direct fluorescent antibody (DFA) tests are a crucial diagnostic tool for identifying certain respiratory infections. Understanding these tests can be helpful, especially when considering conditions like narcolepsy with cataplexy, a fascinating neurological disorder, which you can learn more about by checking out this helpful resource: faqs what is narcolepsy with cataplexy. However, DFA tests remain a key component in pinpointing the specific pathogens causing respiratory issues.
It’s important to use a sterile container to prevent contamination.
- Patient Instruction: Patients should be clearly instructed on the importance of coughing up sputum from deep within the lungs, rather than saliva or phlegm from the throat. This requires adequate explanation, including the distinction between the desired specimen and other secretions. The collection should be performed in a clean environment to avoid cross-contamination.
- Sterile Containers: Use sterile, leak-proof containers to collect the sputum. These containers are specifically designed for clinical specimen collection and should be clearly labeled with the patient’s identification details, date, and time of collection.
- Sample Volume: The optimal sample volume for DFA testing varies depending on the specific laboratory procedure. However, a sufficient amount of sputum is necessary to ensure adequate material for examination.
Sputum Preparation for DFA Testing
The preparation of the sputum sample is critical to ensure that the target organisms are adequately exposed to the fluorescent antibodies.
- Immediate Processing: Ideally, the sputum sample should be processed immediately after collection. However, if immediate processing is not possible, the sample should be refrigerated (at 2-8°C) and processed within 24 hours to minimize degradation of the target pathogens.
- Specimen Decontamination: A decontamination step is often necessary to remove interfering substances such as saliva, mucus, or cellular debris. This may involve a series of washes and centrifugation steps to separate the desired microbial components from other materials.
- Smear Preparation: A thin smear of the sputum sample is prepared on a glass slide. This allows for efficient visualization and identification of the target organisms under a fluorescent microscope.
Potential Sources of Error
Errors during specimen collection and preparation can lead to inaccurate DFA results.
- Contamination: Contamination of the sample with extraneous materials, such as saliva, can interfere with the test and lead to false-positive or false-negative results. Thorough collection procedures and sample handling are critical to minimize contamination.
- Improper Handling: Delayed processing or inappropriate storage conditions can compromise the integrity of the specimen, leading to inaccurate results. Maintaining the proper temperature and avoiding cross-contamination during transport and processing is essential.
- Insufficient Sample Volume: An insufficient sample volume may not contain a sufficient number of target organisms to be detected by the DFA test. Adequate volume is crucial for reliable results.
Specimen Handling and Transport
Proper handling and transport are critical for maintaining the integrity of the specimen.
- Secure Packaging: The sputum sample should be packaged securely to prevent leakage or spillage during transport. A sturdy container with a tight-fitting lid is essential.
- Chain of Custody: Maintaining a proper chain of custody is essential to ensure the traceability and integrity of the sample throughout the entire process.
- Labeling: Properly labeling the container with the patient’s information, date, and time of collection is crucial for accurate identification and tracking.
Suitable Sputum Specimens and Preparation
| Specimen Type | Appropriate Preparation |
|---|---|
| Induced Sputum | Collect as soon as possible after induction, following standard collection procedures. |
| Expectorated Sputum | Collect in a sterile container, ideally in the morning before eating or drinking. Process promptly or refrigerate if immediate processing is not possible. |
| Bronchoalveolar Lavage (BAL) Fluid | Collect BAL fluid, centrifuge to obtain sediment. Prepare smears from the sediment. |
Principle of the DFA Test
The direct fluorescent antibody (DFA) test is a rapid and sensitive method for identifying specific microorganisms in clinical specimens, such as sputum. Its unique capability to directly visualize the target organism under a fluorescent microscope makes it a valuable tool in microbiology labs. This method is particularly useful for diagnosing infections caused by organisms that might be difficult to cultivate in a laboratory setting.The DFA test leverages the principle of immunofluorescence, utilizing labeled antibodies to detect and identify the presence of specific microorganisms in a sample.
This technique provides a quick turnaround time, aiding in timely diagnosis and appropriate treatment decisions.
Immunologic Principle, Sputum direct fluorescent antibody dfa
The DFA test relies on the specific binding of antibodies to antigens. Antibodies, highly specialized proteins produced by the immune system, recognize and bind to specific molecular structures on the surface of microorganisms. These antigens are unique markers for each type of organism. The antibodies used in the DFA test are pre-labeled with a fluorescent dye. This labeling allows for visualization of the antibody-antigen complex under a fluorescence microscope.
Components of the DFA Test Procedure
The DFA test utilizes several key components:
- Fluorescently-labeled antibodies: These antibodies are specifically designed to bind to a particular target organism. They are crucial for detecting the presence of the organism in the specimen.
- Specimen: The sample, such as sputum, is collected and prepared to facilitate the detection of the target microorganism.
- Fluorescent microscope: The microscope is equipped with a special light source that excites the fluorescent dye, allowing the antibody-antigen complexes to be visualized.
Antibody Binding to Target Organism
The fluorescently-labeled antibody binds to the specific antigen on the target organism’s surface through a process known as antigen-antibody binding. This interaction is highly specific, ensuring that the antibody only binds to the target organism and not to other components in the specimen. The strength and specificity of this binding are essential for accurate results.
Fluorescence Generation
When the labeled antibody binds to the target organism, the fluorescent dye is activated. The excitation light source from the microscope illuminates the fluorescent dye, causing it to emit light at a different wavelength. This emitted light is detected by the microscope’s camera and displayed as fluorescence. The intensity and color of the fluorescence are indicative of the presence and quantity of the target organism in the sample.
Flowchart of the DFA Test
+-----------------+ | Specimen | +-----------------+ | Preparation |--->+-----------------+ +-----------------+ | Antibody Binding| | Sample Prep |--->+-----------------+ +-----------------+ | | DFA Reagent Add|--->+-----------------+ | |--->| Fluorescent | +-----------------+ | Visualization| | Antibody Incubation|--->+-----------------+ | |--->| +-----------------+ | Result Analysis | | Observation Under |--->+-----------------+ | Fluorescence Micr.|--->| +-----------------+ | | Result |--->+-----------------+ | | +-----------------+
Interpretation of Results
Deciphering the results of a Sputum Direct Fluorescent Antibody (DFA) test is crucial for accurate diagnosis and subsequent treatment of respiratory infections.
A correct interpretation relies on understanding the test’s limitations, potential sources of error, and the clinical context of the patient’s presentation. The DFA test provides a rapid and relatively inexpensive method for identifying specific pathogens in sputum samples, but it’s not a definitive answer. Proper interpretation involves considering the test’s sensitivity and specificity alongside other diagnostic tools.
Positive DFA Test Results
A positive DFA test result indicates the presence of the targeted pathogen in the sputum sample. This finding, however, requires careful consideration within the broader clinical picture. A positive result strongly suggests an infection, but further investigation might be necessary to determine the severity and the optimal treatment approach. The presence of certain organisms in sputum can be a strong indicator of various respiratory infections.
For example, a positive result for
-Legionella pneumophila* in a patient with pneumonia-like symptoms could strongly suggest Legionnaires’ disease.
Negative DFA Test Results
A negative DFA test result signifies that the targeted pathogen was not detected in the sputum sample. This result does not definitively rule out infection, especially if the clinical presentation strongly suggests one. The patient’s symptoms, the severity of the illness, and the presence of other symptoms should be considered alongside the negative DFA result. A negative result might also suggest the infection is caused by a different pathogen than the one tested for, or the infection is not yet in a stage where the target organism is present in the sample.
Causes of False-Positive and False-Negative Results
False-positive results in a DFA test can arise from cross-reactivity with other antigens, contamination of the sample, or a previous infection with a similar organism. In contrast, false-negative results may be due to low numbers of the target organism in the sample, improper specimen collection or preparation, or the use of an inappropriate antibody in the test. It’s also possible that the target organism is not the cause of the infection, or it’s present but not in a detectable amount in the sample at that time.
Limitations of the DFA Test
The DFA test, like any diagnostic tool, has certain limitations. It is not as sensitive as culture methods for detecting some organisms, especially when the number of pathogens is low. The test’s accuracy depends on the quality of the specimen and the expertise of the laboratory personnel performing the test. Furthermore, the DFA test is designed to detect specific organisms.
If the infection is caused by a pathogen not included in the test, the result will be negative, even if the infection is present.
Comparison of DFA Results with Other Diagnostic Methods
| Diagnostic Method | Strengths | Weaknesses |
|---|---|---|
| DFA | Rapid, relatively inexpensive, detects specific organisms | Less sensitive than culture, depends on sample quality |
| Culture | High sensitivity, identifies specific organism | Time-consuming, may not be able to identify all organisms |
| PCR | High sensitivity and specificity, detects genetic material | More expensive, may not always identify viable organisms |
Clinical Significance of Positive DFA Results
| Organism | Clinical Significance |
|---|---|
| *Legionella pneumophila* | Legionnaires’ disease |
| *Haemophilus influenzae* | Bacterial pneumonia, epiglottitis |
| *Streptococcus pneumoniae* | Pneumonia, meningitis |
| *Chlamydia pneumoniae* | Respiratory infections |
Applications and Uses
Sputum direct fluorescent antibody (DFA) testing stands as a valuable diagnostic tool in clinical microbiology, offering rapid and efficient identification of various respiratory pathogens. This technique’s speed is particularly advantageous in situations requiring prompt treatment decisions, especially in patients with severe respiratory infections. The method’s specificity and sensitivity contribute to accurate diagnoses, minimizing the need for more time-consuming and expensive confirmatory tests in many cases.
Applications in Clinical Microbiology
DFA testing is a critical component of the diagnostic pathway for respiratory infections. It plays a significant role in guiding treatment strategies by rapidly identifying the causative agent. The test’s speed allows for timely interventions, which can be crucial in managing severe infections, preventing complications, and optimizing patient outcomes.
Infectious Agents Detectable by DFA
DFA testing can detect a variety of infectious agents responsible for respiratory tract infections. These agents include bacteria, fungi, and viruses, each with distinct clinical implications. The ability to rapidly identify these pathogens helps clinicians make informed decisions about patient management and treatment protocols.
Specific Organisms Detected
The DFA test is particularly effective in detecting specific organisms commonly associated with respiratory infections. These include, but are not limited to,
-Legionella pneumophila*,
-Mycobacterium tuberculosis*,
-Chlamydia pneumoniae*, and various influenza viruses. The test’s ability to target specific organisms helps clinicians tailor treatment to the specific pathogen, leading to improved patient outcomes.
List of Pathogens Detectable by DFA
- Legionella pneumophila
- Mycobacterium tuberculosis
- Chlamydia pneumoniae
- Influenza viruses (various types)
- Streptococcus pneumoniae
- Haemophilus influenzae
- Pseudomonas aeruginosa
- Staphylococcus aureus
Clinical Implications of Detectable Pathogens
Understanding the clinical implications of the detectable pathogens is crucial for appropriate patient management. The rapid identification of the specific pathogen allows clinicians to select the most effective antimicrobial therapies and tailor treatment protocols. This targeted approach is particularly beneficial in preventing the development of drug resistance.
| Pathogen | Clinical Implications |
|---|---|
| Legionella pneumophila | Causes Legionnaires’ disease, a severe form of pneumonia, often requiring aggressive antibiotic treatment. |
| Mycobacterium tuberculosis | Causes tuberculosis, a chronic infectious disease that can affect various organs. Treatment requires prolonged antibiotic therapy. |
| Chlamydia pneumoniae | Causes atypical pneumonia, often presenting with milder symptoms than other types of pneumonia. Appropriate antibiotic treatment is necessary. |
| Influenza viruses | Cause seasonal influenza, ranging from mild symptoms to severe complications, potentially necessitating antiviral medications. |
| Streptococcus pneumoniae | A common cause of bacterial pneumonia, often requiring prompt antibiotic treatment to prevent complications. |
| Haemophilus influenzae | Can cause pneumonia, meningitis, and other infections, particularly in children. Prompt antibiotic treatment is essential. |
| Pseudomonas aeruginosa | Can cause pneumonia, especially in immunocompromised patients, and often requires specific antibiotic regimens. |
| Staphylococcus aureus | Causes pneumonia and other respiratory infections, including those that can be methicillin-resistant (MRSA), necessitating specific antibiotic regimens. |
Comparison with Other Diagnostic Methods
The direct fluorescent antibody (DFA) test, while a valuable tool, isn’t the only method for identifying respiratory pathogens. Understanding its strengths and weaknesses in comparison with other techniques is crucial for optimal patient care. This section will delve into the comparative advantages and disadvantages, highlighting the turnaround time, cost, and accuracy of each method.
Sputum direct fluorescent antibody (DFA) tests are crucial for diagnosing respiratory infections, like pneumonia. It’s fascinating how advancements in medical diagnostics allow us to pinpoint the cause of illness. Thinking about that, it’s inspiring to hear about Ann Hathaway’s recent pregnancy announcement, ann hathaway reveals pregnancy after fertility struggles , after her fertility struggles. It reminds us of the strength and resilience of the human spirit.
While these two seemingly unrelated topics differ greatly, both highlight the importance of perseverance and medical breakthroughs. DFA tests are vital tools for swift and accurate diagnoses in respiratory cases, ensuring the right treatment plan is followed.
Comparison with Culture Methods
Culture methods, traditionally used for identifying bacterial and viral pathogens, often require several days for growth and identification. This extended turnaround time can delay appropriate treatment. In contrast, the DFA test provides rapid results, typically within 1-2 hours, enabling prompt initiation of therapy. While culture methods offer a more comprehensive identification of the specific pathogen, DFA is highly specific for detecting the presence of certain antigens.
Sputum direct fluorescent antibody (DFA) tests are a quick way to identify certain bacteria and fungi in respiratory samples. Knowing this, it’s crucial to remember that rheumatoid arthritis (RA) patients, for example, might have underlying ear issues that need attention, as detailed in ra patients need to be screened for ear problems. These ear problems can sometimes be linked to respiratory infections, which is why a DFA test remains a valuable tool in diagnosing and managing respiratory conditions.
Comparison with Polymerase Chain Reaction (PCR)
Polymerase Chain Reaction (PCR) is another molecular diagnostic method that can detect genetic material of pathogens. PCR boasts high sensitivity and specificity, often detecting even small amounts of pathogen DNA. DFA, on the other hand, relies on visualizing the pathogen’s antigens. The rapid turnaround time of DFA is a key advantage, particularly in situations requiring immediate intervention.
PCR, while precise, can be more expensive and might require specialized equipment and expertise.
Comparison with Rapid Antigen Tests
Rapid antigen tests, like those for influenza or strep throat, provide relatively quick results, usually within minutes. These tests are generally simple to perform and less expensive than PCR. DFA also offers rapid results, often within an hour or two. DFA, in certain cases, might be more sensitive than rapid antigen tests for specific pathogens, like Legionella pneumophila.
Advantages and Disadvantages of DFA Testing
- Advantages: DFA is a rapid method, often offering results in a few hours. It’s relatively inexpensive compared to some other molecular techniques, such as PCR. It’s simple to perform, requiring minimal specialized equipment.
- Disadvantages: DFA has limited sensitivity, meaning it might not detect all present pathogens, especially in low-concentration situations. The test is highly dependent on the quality of the specimen and the expertise of the technician. It also has limited capacity to differentiate between different strains of pathogens. Additionally, the range of pathogens detectable is narrower compared to culture methods.
Limitations and Strengths of the DFA Test
The DFA test excels at rapid detection of specific antigens, making it valuable in urgent situations where immediate treatment is necessary. Its strength lies in its speed and relative simplicity. However, its sensitivity is often lower compared to molecular methods like PCR, potentially missing some infections. The test’s specificity, however, remains high for the targeted pathogens.
Turnaround Time Comparison
Turnaround time is a critical factor in choosing a diagnostic method. DFA results are typically available within 1 to 2 hours, significantly faster than culture methods (which can take days) and often faster than PCR (which can take hours to several days).
Comparative Table of Diagnostic Methods
| Method | Turnaround Time | Cost | Accuracy |
|---|---|---|---|
| DFA | 1-2 hours | Moderate | High (for targeted pathogens) |
| Culture | 2-5 days | Low | High (for broader range) |
| PCR | 2-4 hours to several days | High | Very high |
| Rapid Antigen Tests | Minutes | Low | Moderate |
Quality Control and Safety Precautions
Sputum direct fluorescent antibody (DFA) testing is a crucial diagnostic tool, but its accuracy relies heavily on meticulous quality control and adherence to strict safety protocols. This section Artikels the essential steps to ensure reliable results and prevent potential hazards during the testing process. Proper handling of specimens and reagents is paramount to maintain the integrity of the test and protect laboratory personnel.
Quality Control Measures for DFA Testing
Ensuring the accuracy and reliability of DFA results requires rigorous quality control measures. These measures are essential for minimizing errors and maintaining the validity of the test.
- Positive and Negative Controls: Running positive and negative controls with each batch of tests is a critical quality control step. These controls verify the functionality of the reagents and the proper performance of the test procedure. Positive controls should demonstrate a clear and easily visible fluorescence, while negative controls should remain negative. Any deviation from these expected results necessitates immediate investigation and re-testing.
- Reagent Validation: Regular validation of reagents is critical. This involves verifying the potency and stability of the reagents used in the test, checking the expiration dates of reagents and ensuring that reagents are stored properly to maintain their efficacy. This validation is performed according to the manufacturer’s instructions.
- Calibration and Maintenance of Equipment: The fluorescence microscope, a crucial piece of equipment in DFA testing, requires regular calibration and maintenance. This ensures that the microscope consistently provides accurate readings and avoids discrepancies in fluorescence intensity readings. Calibration and maintenance schedules are established and followed diligently to prevent any inaccuracies.
Safety Precautions During DFA Testing
Adhering to strict safety precautions is crucial to prevent the transmission of pathogens during DFA testing. These measures protect laboratory personnel and the surrounding environment.
- Personal Protective Equipment (PPE): Appropriate PPE, such as gloves, gowns, and eye protection, should be worn at all times during specimen handling and testing. This minimizes exposure to potentially infectious materials.
- Biosafety Practices: Working surfaces should be decontaminated after each use to eliminate the possibility of cross-contamination. Specimens should be handled with utmost care to avoid splashing or aerosolization. All procedures should be conducted in a designated biosafety cabinet, if available, to limit the spread of infectious agents.
- Proper Specimen Handling: Specimens should be handled carefully to prevent spillage. Any potential contamination should be treated as a biohazard. Thorough hand washing and decontamination of work areas are essential to prevent the spread of infections.
Proper Disposal of Reagents and Contaminated Materials
Disposal of reagents and contaminated materials is crucial to prevent environmental contamination and maintain a safe laboratory environment.
- Reagent Disposal: Expired or unused reagents should be disposed of according to the manufacturer’s instructions and local regulations. Hazardous waste containers are used for proper disposal. This includes following the designated guidelines for chemical waste disposal.
- Specimen Disposal: Contaminated specimens should be disposed of in biohazard containers to prevent the spread of infection. Proper labeling of biohazard containers is mandatory. Disposal methods should be in accordance with local regulations and guidelines.
Importance of Proper Laboratory Practices
Adherence to strict laboratory practices is vital to achieve accurate results and maintain a safe working environment. These practices minimize errors, enhance test reliability, and ensure patient safety.
- Adherence to Standard Operating Procedures (SOPs): All laboratory personnel should strictly adhere to the established standard operating procedures (SOPs) for DFA testing. This ensures consistency in the test procedure and minimizes errors.
- Documentation: Thorough documentation of all test procedures, including quality control results, is essential for troubleshooting and quality assurance. This includes recording the date, time, specimen identification, and results.
- Continuous Monitoring and Evaluation: Continuous monitoring of test performance and evaluation of results are crucial to identify potential problems and ensure the accuracy and reliability of the test. Regular audits and performance assessments should be conducted to ensure compliance with established guidelines.
Detailed Procedure for Handling and Disposing of Specimens and Reagents
| Step | Action | Safety Considerations |
|---|---|---|
| 1 | Specimen Collection | Wear appropriate PPE (gloves, gown, eye protection). Ensure proper labeling of specimen containers. |
| 2 | Specimen Preparation | Handle specimens in a designated biosafety cabinet, if available. Avoid splashing or aerosolization. |
| 3 | Reagent Preparation | Follow manufacturer’s instructions carefully. Store reagents according to the recommended conditions. |
| 4 | Testing Procedure | Follow SOPs meticulously. Maintain a sterile environment during the testing process. |
| 5 | Result Interpretation | Document results accurately and clearly. Compare results to positive and negative controls. |
| 6 | Reagent Disposal | Dispose of reagents in designated containers according to manufacturer’s instructions and local regulations. |
| 7 | Specimen Disposal | Dispose of contaminated specimens in biohazard containers. Ensure proper labeling and adherence to local regulations. |
Recent Advances and Future Trends

The field of sputum direct fluorescent antibody (DFA) testing is continuously evolving, driven by advancements in technology and the increasing need for rapid and accurate diagnostic tools. This evolution reflects a broader trend in diagnostics, moving towards more sophisticated and integrated systems. DFA testing, while established, is not static; it is adapting to meet the evolving demands of clinical practice.
Recent innovations have significantly improved the efficiency and reliability of DFA testing, leading to enhancements in both laboratory workflows and clinical application. This is particularly important in settings where rapid results are crucial for timely treatment decisions. Emerging trends demonstrate a movement towards integrating DFA testing into broader diagnostic panels, highlighting its potential as a valuable component in a comprehensive approach to patient care.
Recent Advances in DFA Technology
Improvements in fluorescent labeling techniques have resulted in more sensitive and specific detection of pathogens. The development of novel probes, conjugated with enhanced fluorescent markers, allows for more efficient binding to target antigens, leading to improved signal amplification. This translates to higher diagnostic accuracy, especially in cases where pathogen detection is challenging. Automated instrumentation has also played a role in streamlining the DFA testing process, reducing manual handling and improving consistency in results.
Emerging Trends in DFA Testing
DFA testing is increasingly integrated into larger diagnostic panels, providing a more comprehensive view of patient conditions. The combination of DFA with other molecular diagnostic methods, such as polymerase chain reaction (PCR), provides a powerful diagnostic synergy. This approach can confirm preliminary findings and offer additional insights into the nature and severity of infections. The integration of DFA results into electronic health records (EHRs) is also becoming more prevalent, facilitating data sharing and analysis across different healthcare settings.
Integration into Broader Diagnostic Workflows
The integration of DFA testing into broader diagnostic workflows is exemplified by its use in conjunction with other rapid diagnostic tests (RDTs). For instance, in a respiratory infection outbreak investigation, DFA results can be rapidly combined with other clinical and epidemiological data to pinpoint the source and severity of the outbreak. This integrated approach enables quicker identification of infectious agents, leading to more effective control measures.
In other cases, DFA testing may be employed as a preliminary screening tool, followed by confirmation with PCR for higher confidence in diagnosis.
Potential of DFA Testing in Point-of-Care Settings
The portability and relative simplicity of DFA testing suggest its potential for use in point-of-care (POC) settings. Miniaturized instruments and pre-packaged reagents are being developed to facilitate rapid, on-site testing. This capability is especially valuable in resource-limited settings or when rapid turnaround times are crucial, such as in emergency departments or remote clinics. The integration of DFA testing into POC systems will improve the accessibility of diagnostic services and accelerate treatment initiation.
Future Directions for Research and Development in DFA Testing
Future research should focus on the development of more sensitive and specific DFA assays for detecting a wider range of pathogens. This includes the development of probes targeting emerging pathogens, ensuring that the testing remains relevant in the face of evolving microbial threats. The exploration of new fluorescent labeling strategies and innovative detection methods will also play a critical role in enhancing the sensitivity and speed of the test.
Finally, research in developing automated and portable DFA systems for POC applications will be essential for expanding access to rapid and reliable diagnostic testing globally.
Epilogue: Sputum Direct Fluorescent Antibody Dfa
In conclusion, sputum DFA provides a valuable, rapid, and targeted approach to diagnosing respiratory infections. This method, encompassing meticulous specimen handling, precise interpretation of results, and a clear understanding of its limitations, empowers healthcare professionals to make informed decisions. The comparison with other diagnostic techniques highlights its strengths and weaknesses, while quality control measures and safety precautions ensure reliable results.
Future advancements and potential applications, particularly in point-of-care settings, further underscore the enduring importance of sputum DFA in modern clinical microbiology.
