Should fda approve super opioid thats stronger than fentanyl – Should FDA approve super opioid that’s stronger than fentanyl? This question sparks intense debate, weighing potential benefits against devastating risks. A super-opioid, theoretically more potent than fentanyl, could revolutionize pain management but carries a terrifying potential for overdose, addiction, and misuse, exacerbating the already dire opioid crisis. This exploration delves into the complex factors surrounding such a decision, examining the potential risks and benefits, public health implications, regulatory hurdles, ethical considerations, alternative treatments, and the scientific evidence.
The potential for a super-opioid to revolutionize pain management, while promising, is met with significant concern about the potential for increased addiction and overdose. This necessitates a thorough analysis of the various perspectives, from medical professionals and policymakers to patients and the general public.
Potential Risks and Benefits
The development of a super-opioid, significantly stronger than fentanyl, presents a complex ethical and public health dilemma. While potent analgesics can be crucial for managing severe pain, the potential for misuse and devastating consequences necessitates careful consideration of the risks and benefits. A thorough evaluation must weigh the potential medical advantages against the inherent dangers of such a powerful substance.
Potential for Overdose and Respiratory Depression
A super-opioid’s heightened potency drastically increases the risk of overdose, particularly given the already significant challenge posed by fentanyl. A smaller dose can lead to respiratory depression, a life-threatening condition where breathing becomes dangerously slow or stops. This heightened risk necessitates meticulous patient monitoring and stringent safety protocols, including the need for readily available naloxone to counteract the opioid’s effects.
The FDA’s decision on approving a super-opioid stronger than fentanyl is a complex one. While potent painkillers are crucial, the potential for misuse and addiction is a major concern. Considering the parallels to treating rabies symptoms with rabies, which, as explored in this insightful article ( can you treat rabies symptoms with rabies ), is unfortunately not a viable approach, a similar cautionary tale applies.
Ultimately, a balanced risk-benefit analysis is needed before approving such a powerful opioid.
The potential for accidental or intentional overdose increases significantly with the availability of a more potent substance.
Potential for Addiction and Dependence
The addictive nature of opioids is well-documented. A super-opioid, due to its enhanced potency, likely carries an even higher risk of addiction and dependence. The brain’s reward pathways are highly susceptible to stimulation by these drugs, potentially leading to compulsive drug-seeking behavior and a significant disruption of normal life functions. This poses a significant threat to individuals who are already vulnerable to addiction.
Potential for Adverse Health Effects
The long-term effects of super-opioids are largely unknown. While some potential benefits may exist in managing severe chronic pain, the potential for unforeseen and severe adverse health effects remains a serious concern. The increased potency may exacerbate existing health issues and potentially cause new, previously unobserved complications. A rigorous testing process is necessary to understand these effects before widespread use.
Potential Benefits (If Any) and Circumstances
Potential benefits of a super-opioid may lie in the precise and controlled management of severe chronic pain, particularly in cases where current treatments are ineffective. However, these benefits must be carefully weighed against the substantial risks. The development and implementation of a rigorous pain management protocol, coupled with close monitoring of patients, are essential. It’s crucial to understand that such a powerful drug should only be considered in situations where other options have failed and where the potential benefits clearly outweigh the immense risks.
Comparison to Existing Opioid Treatments, Should fda approve super opioid thats stronger than fentanyl
Existing opioid treatments, while effective in some cases, are associated with substantial risks. A super-opioid, with its increased potency, likely amplifies these risks. The crucial comparison lies in the balance between efficacy and safety. The risks of overdose, addiction, and adverse health effects must be weighed against the potential benefits for patients with intractable pain conditions.
Potential for Misuse and Abuse
The increased potency of a super-opioid significantly raises the potential for misuse and abuse. The black market’s interest in such a substance is undeniable, leading to a surge in illicit trafficking and potential diversion from legitimate medical use. This possibility must be considered and mitigation strategies must be implemented to prevent the substance from entering the illicit drug market.
Impact on the Current Opioid Crisis
The introduction of a super-opioid carries the potential to exacerbate the existing opioid crisis. The increased potency could further fuel overdose deaths and addiction rates, potentially making the crisis even more difficult to manage. Careful consideration must be given to the potential impact on the already fragile healthcare system.
Potential Risks and Benefits Table
| Risk Category | Description | Severity | Potential Mitigation Strategies |
|---|---|---|---|
| Overdose | Increased risk of respiratory depression and death due to a smaller dose. | High | Stricter prescribing guidelines, increased patient monitoring, readily available naloxone. |
| Addiction | Higher likelihood of addiction and dependence due to increased potency. | High | Robust addiction treatment programs, strict pain management protocols. |
| Adverse Health Effects | Potential for unknown long-term health complications. | High | Extensive pre-market testing and long-term follow-up studies. |
| Misuse and Abuse | Increased risk of diversion to the black market. | High | Stronger regulatory oversight, robust tracking systems, and international collaboration. |
| Impact on Opioid Crisis | Potential to worsen the current crisis. | High | Public health awareness campaigns, enhanced prevention strategies, and improved access to treatment. |
Public Health Implications
The potential approval of a super-opioid, a synthetic opioid significantly more potent than fentanyl, presents a profound and complex public health challenge. This heightened potency could drastically alter the current opioid crisis landscape, potentially leading to an even more devastating escalation in overdose deaths, addiction rates, and related societal costs. Understanding the potential implications is crucial for developing proactive strategies to mitigate the harm and support affected individuals and communities.
Potential Impact on Overdose Deaths
The increased potency of a super-opioid directly correlates with a heightened risk of accidental overdose. A single dose could prove fatal for individuals unknowingly exposed to the substance, even in low concentrations. This is exemplified by the rapid rise in fentanyl-related deaths, where even trace amounts can cause respiratory arrest. The super-opioid’s potency would exacerbate this risk, potentially leading to an unprecedented spike in overdose fatalities.
Impact on Addiction Rates
The high potential reward and rapid onset of euphoric effects associated with a super-opioid may significantly increase the likelihood of addiction. Individuals seeking pain relief or experiencing recreational drug use could rapidly develop dependence. This is further compounded by the potential for rapid tolerance development, driving individuals to seek higher doses and potentially leading to a vicious cycle of addiction.
The FDA’s decision on approving a super-opioid stronger than fentanyl is a tricky one. Weighing the potential for pain relief against the very real risk of overdose is crucial. Meanwhile, it’s important to remember that even with advanced genetic testing like the 23andMe breast cancer test, limits of 23andMe breast cancer test highlight the complexity of predicting and preventing disease.
Ultimately, the FDA needs to balance the benefits with the potential for harm, and that’s a tough call in any case.
The increased potency of the super-opioid may result in a faster and more profound physiological dependence, further complicating the recovery process.
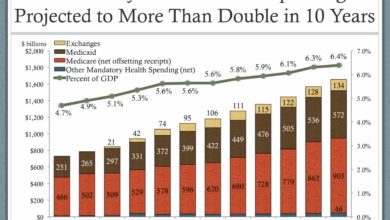
Healthcare Expense Increase
The surge in overdose deaths and addiction rates directly translates into substantial increases in healthcare expenses. Emergency room visits, intensive care unit stays, treatment programs, and long-term care for individuals struggling with addiction will strain healthcare systems and resources. This would necessitate significant investment in addiction treatment centers, specialized personnel training, and preventative care measures, leading to an enormous financial burden on society.
Similar scenarios can be observed in regions experiencing significant opioid crises, where healthcare costs skyrocket in response to increased demand for treatment and care.
Strategies to Address the Crisis
Addressing the potential public health crisis necessitates a multi-pronged approach. Enhanced public awareness campaigns are crucial to educate the public about the risks associated with the super-opioid and the importance of responsible drug use. Harm reduction strategies, such as the provision of naloxone, should be scaled up significantly. Increased access to comprehensive addiction treatment facilities, including counseling, therapy, and medication-assisted treatment (MAT), is vital to support individuals struggling with addiction.
Public Health Outcomes Comparison
A comparison of potential public health outcomes with and without the approval of the super-opioid highlights the critical need for careful consideration. Without the approval of the super-opioid, the current opioid crisis remains a significant concern. However, the approval of a super-opioid would significantly exacerbate the crisis, potentially leading to a catastrophic increase in overdose deaths, addiction rates, and associated healthcare costs.
Summary Table
| Potential Public Health Consequence | Suggested Countermeasures |
|---|---|
| Increased overdose deaths | Enhanced public awareness campaigns, increased access to naloxone, and improved emergency response protocols. |
| Higher addiction rates | Expanded access to comprehensive addiction treatment facilities, including counseling, therapy, and medication-assisted treatment (MAT). |
| Significant increase in healthcare costs | Increased funding for healthcare systems, development of specialized treatment protocols, and preventative care programs. |
Regulatory Considerations
Navigating the complex regulatory landscape is crucial for any new drug, especially one as potent as a super-opioid. The FDA’s rigorous approval process ensures that potential benefits are weighed against significant risks, protecting public health. This process, while demanding, is essential to prevent harm and ensure responsible introduction of novel therapies.The FDA’s evaluation process for a super-opioid will likely focus on several key areas, including its potential for misuse and addiction, and the severity of its side effects.
The agency’s commitment to safety and efficacy is paramount.
Regulatory Hurdles and Processes
The FDA approval process for a super-opioid will likely be considerably more demanding than for existing opioid medications. This stems from the heightened potential for abuse and addiction associated with a significantly stronger analgesic. The agency will rigorously scrutinize the drug’s mechanism of action, potential for respiratory depression, and risk of overdose. They will also need to demonstrate that the super-opioid offers a substantial clinical advantage over existing treatments.
Criteria for Safety and Efficacy Evaluation
The FDA will evaluate the super-opioid’s safety and efficacy based on rigorous scientific evidence. Crucial criteria include:
- Preclinical studies: Extensive animal studies will assess the drug’s potential for adverse effects, including respiratory depression, tolerance, and dependence.
- Phase I clinical trials: These trials will evaluate the drug’s safety in a small group of healthy volunteers, focusing on pharmacokinetics (how the body absorbs, distributes, metabolizes, and eliminates the drug) and potential side effects.
- Phase II clinical trials: These trials will assess the drug’s effectiveness and safety in a larger group of patients with the target condition, comparing it to existing treatments and placebos. Key metrics will include pain relief, duration of effect, and the occurrence of adverse events.
- Phase III clinical trials: Large-scale trials will further evaluate the drug’s efficacy and safety in a diverse patient population. This phase will include longer-term assessments of the risk of addiction, misuse, and overdose.
- Post-marketing surveillance: The FDA will continue to monitor the drug’s safety and efficacy after its approval, collecting data on long-term effects and potential adverse events in real-world settings.
Clinical Trials
The use of robust and well-designed clinical trials is crucial in assessing the risks and benefits of a super-opioid. The trials must adhere to stringent ethical guidelines, ensuring patient safety and informed consent. The results of these trials will inform the FDA’s decision-making process, enabling a balanced evaluation of the drug’s potential impact on public health. These trials must also compare the super-opioid to existing, established treatments to demonstrate its clinical superiority.
Comparison to Existing Opioids
The approval process for a super-opioid will differ from that of existing opioids in several key ways. The increased potency and potential for misuse necessitate more rigorous preclinical and clinical trials, including longer-term studies to assess addiction potential and overdose risk. The focus will be on demonstrating a significant clinical advantage over existing options, justifying the higher risk profile.
Impact on Future Drug Development
The approval process for a super-opioid will undoubtedly set a precedent for future drug development, particularly in the realm of pain management. The emphasis on stringent safety standards and comprehensive clinical trials will likely become the benchmark for evaluating other novel medications, influencing the way similar drugs are researched and developed.
Regulatory Path Flowchart
The following flowchart illustrates the regulatory path for a super-opioid, highlighting the key stages and considerations.
[Start]
--> Preclinical Studies
--> Phase I Clinical Trials
--> Phase II Clinical Trials
--> Phase III Clinical Trials
--> Safety and Efficacy Review by FDA
--> Risk/Benefit Assessment
--> Potential for Misuse and Addiction Evaluation
--> FDA Approval/Rejection
--> Post-Marketing Surveillance
--> [End]
Ethical and Societal Impacts

The approval of a super-opioid, a synthetic opioid potentially more potent than fentanyl, presents a complex web of ethical and societal challenges.
Beyond the obvious risks of increased overdose deaths, the potential for misuse and abuse, and the strain on healthcare systems, the very nature of such a powerful drug forces us to confront fundamental questions about societal responsibility and the limits of scientific advancement. This analysis delves into the ethical considerations surrounding this potent drug, its impact on vulnerable populations, and potential societal conflicts that may arise.
The ethical implications of a super-opioid extend beyond individual patients to encompass the entire societal fabric. Balancing the potential benefits, such as managing severe chronic pain, against the immense risks of addiction and death, requires a careful and nuanced approach. This requires a thorough evaluation of potential unintended consequences and a robust framework for mitigating them.
Ethical Considerations Surrounding Approval
The decision to approve a super-opioid necessitates a rigorous ethical evaluation. One crucial aspect is the potential for disproportionate harm to vulnerable populations, including the economically disadvantaged, individuals with mental health conditions, and marginalized communities. These groups often face systemic barriers to accessing healthcare and support systems, increasing their susceptibility to opioid misuse. Therefore, the approval process must incorporate measures to protect these vulnerable populations and ensure equitable access to treatment and prevention strategies.
Potential Impact on Vulnerable Populations
Vulnerable populations are disproportionately affected by opioid crises. Increased opioid potency exacerbates existing societal vulnerabilities. Lower socioeconomic status, limited access to healthcare, and pre-existing mental health conditions make individuals more susceptible to addiction. A super-opioid would likely worsen this situation, increasing overdose risks and potentially leading to increased mortality rates within these groups. Specific interventions tailored to the unique needs of these populations, including targeted prevention campaigns and readily available treatment options, must be developed and prioritized.
Potential Societal Conflicts
The approval of a super-opioid could spark significant societal conflicts. Public health advocates might clash with pharmaceutical companies seeking to maximize profits. Different stakeholders – patients, healthcare providers, policymakers – will have varying perspectives and priorities. A crucial step in mitigating these conflicts is fostering open dialogue and consensus-building among all affected parties.
Stakeholder Perspectives
| Stakeholder | Perspective | Potential Consequences |
|---|---|---|
| Patients | May see a potential benefit for severe chronic pain management, but also a heightened risk of addiction. | Increased access to potentially life-saving pain relief, but also a higher risk of opioid use disorder. |
| Healthcare Professionals | Concerned about the potential for increased overdose rates and the challenge of treating patients with addiction. | Increased demand for treatment and resources, potentially overwhelming existing healthcare systems. |
| Policymakers | Balancing the potential benefits with the risks to public health, considering the economic impact and legal implications. | Need to create and enforce robust regulations, potentially facing pressure from various stakeholders. |
| Pharmaceutical Companies | Seeking to expand market share and potentially profit from the new drug. | Potential for ethical concerns regarding profit maximization over public health, as well as issues of accessibility and affordability. |
Strategies to Address Ethical Challenges
Addressing the ethical and societal challenges posed by a super-opioid necessitates a multifaceted approach. This includes robust pre-approval risk assessments, community engagement, and the development of tailored prevention and treatment programs. Furthermore, promoting education and awareness about the dangers of opioid misuse and the importance of seeking help are crucial. The creation of a dedicated support system for individuals at risk is also essential.
Ethical Perspectives and Potential Consequences
- Utilitarian Perspective: This perspective might justify approval if the benefits (managing severe pain) outweigh the potential harm (increased addiction). However, the potential for widespread harm and disproportionate impact on vulnerable populations must be carefully considered. This perspective might overlook the potential long-term consequences of widespread addiction.
- Deontological Perspective: This perspective emphasizes ethical duties and principles. A deontological approach would likely prioritize preventing harm, potentially leading to rejection of approval due to the anticipated increase in opioid-related harm. The potential for a duty to protect vulnerable populations could be a key consideration.
- Rights-Based Perspective: This perspective centers on individual rights, including the right to access pain management. However, it also acknowledges the rights of vulnerable populations to protection from harm. A rights-based approach might advocate for a conditional approval, coupled with strict regulations and access limitations.
Alternative Treatment Options
Navigating opioid use disorder (OUD) requires a multifaceted approach, and alternative treatments offer crucial pathways to recovery. These methods, often combined with behavioral therapies, aim to reduce reliance on opioids, manage withdrawal symptoms, and foster long-term well-being. Beyond medication-assisted treatment (MAT), various options exist, each with its own strengths and weaknesses.
Alternative treatments for opioid use disorder represent a spectrum of approaches, ranging from psychosocial interventions to holistic therapies. Their effectiveness and suitability vary significantly depending on individual needs and circumstances. Understanding the nuances of each option allows for a more informed and personalized treatment plan.
Medication-Assisted Treatment (MAT) Alternatives
MAT, while highly effective, isn’t the only avenue for OUD treatment. Alternative medications and therapies provide complementary approaches, especially when MAT isn’t suitable or isn’t working optimally. These alternatives aim to reduce the reliance on opioids while addressing underlying issues like mental health concerns or trauma.
- Buprenorphine-naloxone combination therapy, while a core component of MAT, can be supplemented by other medications to manage cravings or withdrawal symptoms more effectively. For instance, gabapentin or pregabalin can provide additional relief from nerve pain or anxiety often associated with opioid withdrawal.
- Clonidine, an alpha-2 adrenergic agonist, is often used to manage autonomic hyperactivity during opioid withdrawal. It can reduce the severity of symptoms like sweating, tremors, and hypertension, improving patient comfort and adherence to treatment.
- Naltrexone, while primarily used in MAT for opioid use disorder, can be paired with other medications or therapies for enhanced outcomes. Combining naltrexone with psychotherapy, for example, can address the underlying psychological factors contributing to opioid use.
Psychosocial Interventions
Psychosocial therapies are crucial components of comprehensive OUD treatment. They focus on addressing the psychological and social factors that contribute to opioid use, promoting healthier coping mechanisms, and improving overall well-being.
The FDA’s decision on approving a super-opioid stronger than fentanyl is a serious issue. While exploring stronger painkillers is necessary, it’s crucial to consider the potential for misuse and addiction. Perhaps exploring alternative therapies for pets, like acupuncture or herbal remedies, could offer a less risky approach to pain management for animals. This could provide a path toward a more holistic approach to treating pain, offering a valuable alternative to powerful opioids.
Ultimately, the FDA’s decision should prioritize safety and consider all options before approving such a potent opioid. alternative therapies for pets
- Cognitive Behavioral Therapy (CBT) is a widely recognized and effective therapeutic approach for OUD. CBT helps patients identify and modify negative thought patterns and behaviors related to opioid use, teaching coping skills for stress and cravings. For example, a patient might learn to identify triggers that lead to opioid use and develop strategies to manage those triggers.
- Motivational Interviewing (MI) is a patient-centered counseling technique that helps individuals explore their ambivalence towards change and build intrinsic motivation for recovery. This approach emphasizes collaboration and respect, empowering patients to take ownership of their treatment.
- Family therapy plays a significant role in supporting the recovery process for individuals with OUD. It helps family members understand the disorder, improve communication, and learn how to support the recovering individual effectively. This support system is critical for long-term recovery.
Holistic Approaches
Holistic approaches recognize the interconnectedness of physical, mental, and emotional well-being in OUD recovery. These treatments consider the whole person, incorporating lifestyle changes, mind-body practices, and social support.
- Mindfulness-based therapies, like mindfulness-based stress reduction (MBSR), can help individuals develop awareness of their thoughts and emotions, reducing cravings and improving emotional regulation. Mindfulness practices can be integrated into daily life to manage stress and promote well-being.
- Nutritional counseling can help identify and address nutritional deficiencies that may exacerbate opioid withdrawal symptoms or contribute to overall health concerns. Improving diet and nutritional intake can positively impact recovery.
- Exercise programs can enhance physical health and reduce stress, which are both crucial for recovery from OUD. Regular physical activity can improve mood, reduce anxiety, and enhance overall well-being.
Accessibility and Affordability
The accessibility and affordability of alternative treatment options vary considerably. Factors like insurance coverage, geographic location, and availability of specialized programs influence treatment access. Many communities lack sufficient resources for comprehensive OUD care, and equitable access remains a significant challenge.
Preventative Measures and Harm Reduction Strategies
Preventing opioid use disorder in the first place and mitigating harm associated with opioid use are essential components of a comprehensive public health strategy. Strategies such as promoting safe opioid prescribing practices, improving access to naloxone, and providing comprehensive education about opioid risks are vital.
Summary Table
| Treatment Type | Description | Strengths | Weaknesses |
|---|---|---|---|
| Medication-Assisted Treatment (MAT) Alternatives | Utilizes medications alongside behavioral therapies to manage withdrawal and cravings | Effective in reducing opioid use, managing withdrawal, and improving treatment adherence | Potential for side effects, requires ongoing monitoring, and may not address underlying issues |
| Psychosocial Interventions | Focuses on psychological and social factors influencing opioid use | Addresses underlying issues, builds coping skills, and promotes long-term recovery | Can be time-consuming, may not be effective for all individuals, and requires trained professionals |
| Holistic Approaches | Integrates mind-body practices and lifestyle changes into treatment | Promotes overall well-being, addresses physical and emotional factors, and fosters long-term lifestyle changes | May not be as readily available or affordable, may not be effective for all individuals |
Scientific Evidence: Should Fda Approve Super Opioid Thats Stronger Than Fentanyl

The development of a super-opioid, a potent synthetic opioid exceeding fentanyl’s strength, necessitates a robust foundation of scientific evidence. This evidence must rigorously demonstrate both the potential benefits and the inherent dangers of such a drug. However, the development of a super-opioid also raises critical ethical and societal concerns. Careful consideration of the potential risks and benefits, alongside rigorous scientific evaluation, is paramount.
The scientific evidence supporting the development of a super-opioid must encompass detailed pharmacological studies, toxicological assessments, and clinical trials. These studies should compare the drug’s efficacy and safety profile against existing opioid analgesics, including fentanyl. Furthermore, the studies must explore potential long-term health consequences, especially concerning addiction and overdose risk.
Summary of Supporting Scientific Evidence
The scientific community has extensive experience with opioid development and pharmacology. Existing research has established the mechanisms of action, efficacy, and potential adverse effects of various opioid analgesics. This knowledge base serves as a critical foundation for understanding the potential effects of a super-opioid. Data from preclinical studies, including animal models, can provide insights into the drug’s potential therapeutic applications and associated risks.
However, extrapolation from animal models to humans must be approached with caution, as there are often significant differences in physiological responses.
Potential Impact on Public Perception
The public perception of a super-opioid will likely be heavily influenced by the perceived benefits and risks. If the drug demonstrates a superior ability to manage severe pain while minimizing side effects, it could be perceived favorably. Conversely, concerns about potential increases in addiction rates and overdose deaths will undoubtedly lead to significant public skepticism and resistance. Public education campaigns will be crucial in managing these perceptions.
For instance, the public perception of fentanyl, despite its medical applications, has been overwhelmingly negative due to its misuse and associated overdose crisis.
Limitations of Current Scientific Evidence
Current scientific evidence regarding super-opioids is limited by several factors. The long-term effects of these potent drugs are not fully understood. Furthermore, the potential for abuse and misuse is a major concern, requiring extensive research to predict and mitigate such behaviors. The development of tolerance and dependence is another key area requiring further investigation. A robust body of evidence must address these limitations before the drug is considered for widespread use.
Comparison with Existing Data on Similar Medications
Comparing the scientific evidence for a super-opioid with existing data on similar medications is crucial. This comparison should focus on potency, efficacy, side effect profiles, and potential for abuse. Direct comparisons with fentanyl and other potent opioids will highlight potential similarities and differences in terms of risk and reward. For example, a direct comparison of the potential for respiratory depression between the super-opioid and existing opioids is critical.
Areas for Future Research
Future research should focus on long-term safety assessments, including the development of tolerance and dependence, as well as the exploration of novel strategies for mitigating the risk of abuse. Detailed studies on the impact of super-opioids on various organ systems over extended periods are essential. Research into potential alternative treatment options, including non-opioid pain management strategies, will be crucial.
For example, further research should examine the potential role of behavioral therapies and other non-opioid pain management strategies in combination with super-opioids.
Summary Table of Key Scientific Findings and Limitations
| Key Scientific Finding | Limitations |
|---|---|
| Potent analgesic effects in preclinical studies | Extrapolation to humans may not fully reflect the human response. |
| Potential for reduced side effects compared to existing opioids | Long-term effects and potential for abuse/misuse are not fully understood. |
| Established mechanisms of action for similar opioids | Specific interactions and consequences of the super-opioid’s unique chemical structure need further study. |
Conclusive Thoughts
Ultimately, the decision of whether to approve a super-opioid stronger than fentanyl is fraught with ethical and public health dilemmas. Balancing the potential for improved pain management against the very real risk of exacerbating the opioid crisis demands careful consideration of all factors. Alternative treatment options, robust regulatory oversight, and public awareness campaigns are crucial to mitigate the potential negative consequences.
The discussion necessitates a nuanced approach, recognizing the multifaceted nature of this critical issue.