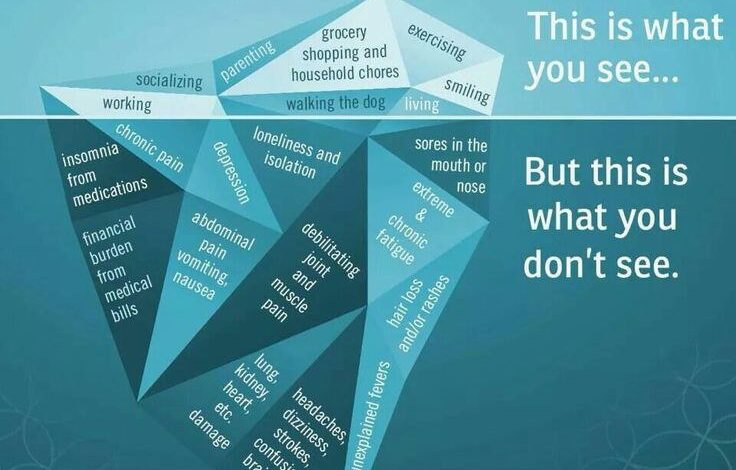
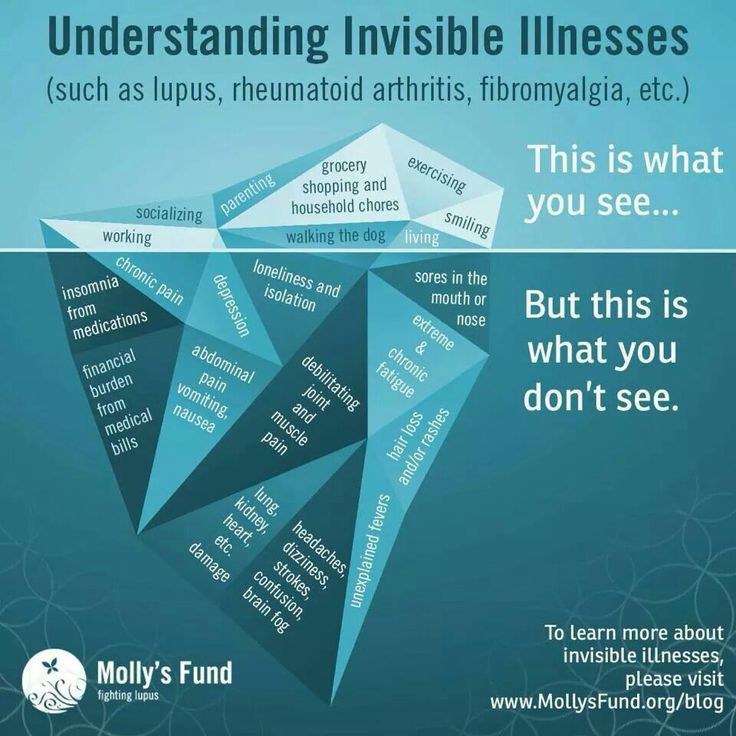
What you should know about invisible illness is crucial for understanding the often-hidden struggles of those affected. These conditions, unlike visible ailments, present unique challenges in diagnosis and recognition, often leading to misinterpretations and delayed care. This post delves into the complexities of invisible illnesses, exploring their diverse types, symptoms, and the profound impact they have on daily life.
From defining invisible illness and exploring its various forms, to understanding the diagnostic process, treatment options, and the importance of societal awareness, this comprehensive guide provides a clear picture of the realities faced by those living with these conditions. It emphasizes the need for empathy, compassion, and accurate information to combat stigma and promote inclusivity.
Defining Invisible Illness

Invisible illnesses, unlike visible ones, are medical conditions that aren’t outwardly apparent. This often leads to significant challenges in diagnosis and societal understanding. Individuals experiencing these conditions may face skepticism, lack of empathy, and a struggle to gain access to appropriate care.These conditions are characterized by a range of symptoms, often internal and difficult to objectively measure. This makes it hard for both patients and healthcare professionals to definitively pinpoint the cause and effect, and consequently, to develop effective treatments.
This inherent difficulty underscores the importance of awareness and understanding.
Defining Invisible Illness
Invisible illnesses encompass a broad spectrum of medical conditions, including chronic fatigue syndrome, fibromyalgia, lupus, multiple sclerosis, and chronic pain syndromes. These conditions frequently present with a multitude of symptoms that are not readily visible, such as fatigue, pain, cognitive dysfunction, and digestive issues. The absence of visible symptoms can make diagnosis more challenging. Furthermore, invisible illnesses can have a significant impact on an individual’s ability to function in daily life.
Challenges in Diagnosis and Recognition
Diagnosing invisible illnesses often requires a combination of patient history, physical examination, and potentially specialized testing. Subjectivity in reporting symptoms and the lack of readily apparent physical indicators can make it harder to establish a definitive diagnosis. This is frequently compounded by the often lengthy process of ruling out other conditions and the need for multiple appointments and specialist consultations.Furthermore, healthcare professionals may not be fully equipped to recognize and manage the complex symptoms associated with invisible illnesses.
This lack of awareness and training can lead to delayed diagnosis and inadequate treatment.
Impact of Societal Misconceptions
Societal misconceptions surrounding invisible illnesses can have a profound impact on individuals experiencing these conditions. These misconceptions frequently lead to feelings of isolation, distrust, and a lack of understanding from family, friends, and even healthcare providers. The societal perception that these conditions are “imagined” or “not real” can cause significant emotional distress and hinder access to appropriate care and support.
Common Characteristics of Invisible Illnesses
Invisible illnesses share several common characteristics that contribute to the challenges of diagnosis and management. These include:
- Variability in symptoms: Symptoms can fluctuate in intensity and frequency, making consistent diagnosis and treatment challenging.
- Subjectivity of symptoms: Many symptoms are subjective, relying on the patient’s self-reporting of pain, fatigue, or cognitive difficulties.
- Lack of objective markers: Unlike visible illnesses, there are often no clear objective markers (such as visible lesions or lab values) to confirm a diagnosis.
- Potential for misdiagnosis: The lack of clear markers can lead to misdiagnosis or delayed diagnosis.
- Impact on daily functioning: Invisible illnesses can significantly impact a person’s ability to perform daily tasks and participate in social activities.
Comparing Invisible and Visible Illnesses
| Characteristic | Invisible Illness | Visible Illness |
|---|---|---|
| Symptoms | Often internal, subjective, and variable in intensity | Usually external, objective, and relatively consistent |
| Diagnosis | Can be challenging, often requiring multiple specialists and extensive testing | Often easier to diagnose based on observable symptoms and physical examinations |
| Treatment | Often involves managing symptoms and addressing the underlying causes | Often involves addressing the physical manifestation of the illness |
| Societal Perception | Can face skepticism and lack of understanding | Generally met with greater societal awareness and understanding |
Types of Invisible Illnesses
Invisible illnesses encompass a vast spectrum of conditions impacting various body systems. These conditions are often challenging to diagnose and manage due to their hidden nature, frequently leading to delayed or misdiagnosis. Understanding the diverse types of invisible illnesses and their associated symptoms is crucial for promoting awareness and improving healthcare outcomes for those affected.
Categorization by Body System, What you should know about invisible illness
Invisible illnesses can be categorized based on the specific body system they affect. This categorization helps in understanding the underlying mechanisms and potential symptoms. For example, neurological conditions often manifest with cognitive impairments or motor dysfunction, while gastrointestinal conditions might involve chronic pain or digestive issues.
- Neurological Conditions: Neurological conditions are often characterized by disruptions in the brain and nervous system, leading to a wide range of symptoms. Examples include multiple sclerosis (MS), Parkinson’s disease, and epilepsy. Symptoms can range from cognitive impairments, such as memory loss or difficulty concentrating, to motor dysfunction, including tremors, weakness, or difficulty with coordination. These conditions often require specialized diagnostic testing, including MRI scans and neurological examinations.
- Gastrointestinal Conditions: Gastrointestinal (GI) conditions can involve various organs in the digestive tract, resulting in chronic discomfort and pain. Examples include irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and celiac disease. Symptoms frequently include abdominal pain, bloating, diarrhea, or constipation. Diagnosis often relies on a combination of patient history, physical examination, and endoscopic procedures.
- Endocrine Conditions: Endocrine conditions relate to hormonal imbalances within the body. Examples include hypothyroidism and diabetes. Symptoms can be diverse and often subtle, ranging from fatigue and weight changes to mood swings and skin issues. Diagnosis involves blood tests to measure hormone levels.
- Mental Health Conditions: Mental health conditions, although often perceived as invisible, are crucial to acknowledge. Examples include anxiety disorders and depression. Symptoms may include persistent sadness, fear, or worry, impacting daily functioning. Diagnosis often involves psychological evaluations and assessments.
Symptoms Associated with Each Type
The symptoms associated with invisible illnesses can vary significantly depending on the specific condition. A comprehensive understanding of the symptoms can assist in early diagnosis and appropriate management.
- Neurological Conditions: Symptoms can include memory problems, difficulty concentrating, tremors, muscle weakness, numbness, or tingling sensations. The severity of symptoms can fluctuate over time.
- Gastrointestinal Conditions: Symptoms may include chronic abdominal pain, bloating, nausea, vomiting, diarrhea, or constipation. These symptoms can significantly impact a person’s quality of life.
- Endocrine Conditions: Symptoms may include fatigue, weight changes, mood swings, hair loss, or skin dryness. These symptoms can sometimes be subtle and easily overlooked.
- Mental Health Conditions: Symptoms may include persistent sadness, feelings of hopelessness, anxiety, panic attacks, difficulty concentrating, or changes in sleep patterns.
Prevalence of Invisible Illnesses
Unfortunately, precise prevalence data for many invisible illnesses is not readily available. Gathering such data can be challenging due to the variable nature of symptoms and the difficulties in accurate diagnosis.
| Condition | Estimated Prevalence (Note: Varies by region and specific subtype) | Diagnostic Process |
|---|---|---|
| Multiple Sclerosis (MS) | Approximately 2.5 million people worldwide | Neurological examination, MRI scans, evoked potentials |
| Irritable Bowel Syndrome (IBS) | Estimated to affect 10-20% of the population | Patient history, physical examination, and possibly endoscopy or colonoscopy |
| Anxiety Disorders | Affects a significant portion of the population, often undiagnosed | Psychological evaluations, symptom assessment, and potentially diagnostic tools |
| Depression | Affects a substantial portion of the population | Psychological evaluations, symptom assessment, and potentially diagnostic tools |
Diagnostic Processes for Invisible Illnesses
Diagnostic processes for invisible illnesses often involve a combination of approaches. It is crucial to consider that the diagnostic path can be lengthy and challenging.
- Patient History: A thorough understanding of the patient’s medical history, symptoms, and lifestyle is a crucial initial step.
- Physical Examination: A physical examination by a healthcare professional can provide valuable insights into potential underlying causes and associated symptoms.
- Diagnostic Tests: Specific diagnostic tests, such as blood tests, imaging scans, or psychological evaluations, can help identify the specific condition.
- Exclusionary Process: Often, the process of ruling out other conditions is equally important.
Symptoms and Experiences
Living with an invisible illness can be incredibly isolating. The invisible nature of the condition often makes it difficult for others to understand the profound impact it has on daily life. This can lead to feelings of frustration, misunderstanding, and even social isolation. This section delves into the diverse symptoms, emotional toll, and practical challenges faced by those living with these conditions.The experience of invisible illness is highly variable, depending on the specific condition and the individual’s response.
Understanding invisible illnesses can be tricky, but it’s important to remember that they’re very real. Finding ways to stay active, like practicing stay fit in the winter months yoga , can be a powerful tool for managing symptoms and boosting overall well-being. Even small steps towards a healthier lifestyle can make a big difference, and that’s crucial for anyone navigating the complexities of these conditions.
Symptoms can manifest in subtle ways, making it challenging to pinpoint the cause of discomfort and fatigue. Furthermore, the fluctuating nature of symptoms can make it difficult to manage daily activities and maintain a sense of normalcy.
Diverse Range of Symptoms
Invisible illnesses encompass a wide spectrum of conditions, each with its own unique set of symptoms. These can range from fatigue and pain to cognitive impairments and digestive issues. Often, the symptoms are subtle and easily dismissed, making it difficult to receive proper diagnosis and treatment. For example, chronic fatigue syndrome can manifest as extreme tiredness, impacting the ability to perform even basic tasks.
Fibromyalgia often presents as widespread musculoskeletal pain, accompanied by sleep disturbances and cognitive difficulties.
Emotional and Psychological Impact
Living with an invisible illness takes a significant emotional toll. The constant struggle with symptoms, the lack of visible signs, and the challenges in receiving validation can lead to feelings of isolation, anxiety, and depression. The uncertainty surrounding the condition and the difficulty in managing symptoms can contribute to feelings of frustration and helplessness. This can also strain relationships with family and friends who may not fully understand the experience.
Moreover, the constant need to explain and advocate for oneself can be emotionally draining.
Personal Anecdotes
One individual, struggling with a chronic neurological condition, found themselves increasingly isolated as their symptoms progressed. Initially, their condition manifested as mild headaches and occasional fatigue. However, as time went on, these symptoms intensified, impacting their ability to work and engage in social activities. The lack of visible signs led to skepticism and a feeling of not being believed, compounding the emotional distress.
Another individual, living with a chronic digestive disorder, found it challenging to maintain a social life due to unpredictable symptoms. The fear of experiencing embarrassing symptoms in public or the need to plan around potential flare-ups impacted their social interactions.
Challenges in Managing Daily Activities
Managing daily activities with invisible illnesses can be extraordinarily difficult. Fluctuating symptoms can disrupt routines and make even simple tasks feel overwhelming. The unpredictability of symptoms often leads to missed appointments, reduced productivity at work, and strained relationships. For example, an individual with a chronic pain condition might experience severe pain flares that prevent them from attending work or social events.
Individuals with cognitive impairments may struggle with concentration and memory, impacting their ability to complete tasks efficiently.
Common Symptoms and Potential Causes
| Symptom | Potential Causes (Examples) |
|---|---|
| Fatigue | Chronic fatigue syndrome, anemia, thyroid issues, certain medications |
| Pain | Fibromyalgia, arthritis, lupus, musculoskeletal issues |
| Cognitive difficulties | Multiple sclerosis, brain fog, certain mental health conditions |
| Digestive issues | Irritable bowel syndrome, celiac disease, inflammatory bowel disease |
| Headaches | Migraines, tension headaches, neurological conditions |
Diagnosis and Treatment
Navigating the path to diagnosis and treatment for invisible illnesses can be a challenging and often frustrating journey. The very nature of these conditions, where symptoms are not always visible, often leads to delays and misdiagnosis, leaving individuals feeling unheard and unsupported. This can have a significant impact on their quality of life and access to appropriate care.
Understanding the complexities involved in diagnosing and treating these conditions is crucial for both patients and healthcare professionals.The process of diagnosing invisible illnesses is multifaceted and requires a collaborative effort between patients, family members, and healthcare providers. The lack of objective markers often makes the diagnostic process lengthy and convoluted. A thorough understanding of the specific condition and its potential symptoms is essential to avoid misinterpretations.
Complexities of Diagnosis
Diagnosing invisible illnesses is often a process of elimination and careful observation. Healthcare professionals must consider various factors, including the patient’s medical history, family history, and lifestyle. The absence of readily apparent physical indicators can lead to delays in diagnosis, which can have a negative impact on the patient’s well-being. Misdiagnosis is also a significant concern, as it can lead to inappropriate treatments and further complications.
Diagnostic Methods
A variety of methods are employed in diagnosing invisible illnesses. These methods often include detailed medical interviews, physical examinations, and laboratory tests. Specialized tests and assessments tailored to the specific suspected condition are crucial. For example, in cases of chronic fatigue syndrome, neuropsychological testing can be essential to evaluate cognitive function. Furthermore, mental health assessments are frequently integral, especially when mental health conditions overlap with or exacerbate invisible illnesses.
Importance of Patient Advocacy
Patient advocacy plays a critical role in the diagnostic process. Patients are often the best source of information regarding their symptoms and experiences. Actively participating in the diagnostic journey, documenting symptoms meticulously, and researching potential conditions can greatly assist healthcare providers in reaching an accurate diagnosis. Advocating for specialized care is essential in cases where a standard medical approach is insufficient.
Sharing personal experiences with other individuals facing similar challenges can be a powerful tool for support and understanding.
Treatment Approaches
Effective management of invisible illnesses often involves a multifaceted approach, encompassing both medical and non-medical strategies. Medical treatments may include medications, therapies, or other interventions tailored to the specific condition. Non-medical strategies may include lifestyle modifications, such as dietary changes, stress management techniques, and regular exercise. For example, a patient with fibromyalgia might benefit from physical therapy, cognitive behavioral therapy (CBT), and a balanced diet.
Patient education and self-management strategies are crucial components in effective treatment.
Table of Medical Specialists
| Invisible Illness | Primary Specialist | Potential Secondary Specialists |
|---|---|---|
| Chronic Fatigue Syndrome | Internal Medicine Physician | Neurologist, Psychiatrist, Physical Therapist |
| Fibromyalgia | Rheumatologist | Pain Management Specialist, Physical Therapist, Psychologist |
| Multiple Chemical Sensitivities (MCS) | Allergist/Immunologist | Environmental Medicine Specialist, Occupational Therapist |
| Irritable Bowel Syndrome (IBS) | Gastroenterologist | Nutritionist, Psychologist |
This table provides a general overview and should not be considered exhaustive. The specific specialists involved may vary depending on the individual’s needs and the complexity of the condition. It’s crucial to consult with healthcare professionals to determine the most appropriate course of treatment.
Living with an Invisible Illness
Living with an invisible illness presents unique challenges beyond the physical symptoms. It often impacts relationships, social interactions, and daily life in ways that can be difficult to understand for those without personal experience. Navigating healthcare, managing symptoms, and maintaining a sense of well-being require specific strategies and support systems.
Impact on Relationships and Social Life
Invisible illnesses can strain relationships with friends, family, and partners. Misunderstandings arise when loved ones struggle to comprehend the constant fatigue, pain, or cognitive impairment experienced. Social situations can become daunting, as individuals may fear judgment or a lack of understanding. This can lead to social isolation and feelings of loneliness, impacting emotional well-being significantly. Open communication and education are crucial for fostering understanding and support within relationships.
Importance of Self-Care and Support Systems
Self-care is paramount for individuals living with invisible illnesses. Regular routines, including healthy eating, sufficient sleep, and stress-reducing activities, are vital for managing symptoms and maintaining overall well-being. A robust support system, whether comprised of family, friends, or support groups, provides emotional and practical assistance during challenging times. These systems can offer encouragement, understanding, and a sense of belonging.
Challenges in Navigating Healthcare Systems
Diagnosis and treatment of invisible illnesses can be significantly delayed or misdiagnosed due to the absence of visible symptoms. Patients may face skepticism from healthcare providers or difficulty in obtaining appropriate testing and care. The need for ongoing monitoring, specialized care, and frequent follow-ups can create additional stress and administrative burdens. Developing a strong relationship with a knowledgeable and empathetic healthcare team is essential.
Strategies for Managing Symptoms and Improving Quality of Life
Effective symptom management is crucial for maintaining a high quality of life. Individuals should explore strategies such as medication, alternative therapies, lifestyle adjustments, and assistive technologies. Developing coping mechanisms for stress and fatigue, practicing relaxation techniques, and establishing a structured daily routine can significantly enhance well-being. Utilizing assistive technologies, such as ergonomic tools or software for managing tasks, can be very beneficial.
Common Support Groups and Resources
This table Artikels various support groups and resources available to individuals with invisible illnesses. These resources offer invaluable emotional and practical support.
| Support Group/Resource | Description | Contact Information (Example) |
|---|---|---|
| National Alliance on Mental Illness (NAMI) | Provides support and education for mental health conditions. | (Phone number, website) |
| Chronic Illness Support Groups (Local Chapters) | Offer peer support and understanding from individuals with similar experiences. | (Website, contact information varies by location) |
| Online Forums and Communities | Provide a space for individuals to connect, share experiences, and seek advice. | (Example: specific forum website) |
| Patient Advocacy Organizations | Work to improve healthcare access and understanding of invisible illnesses. | (Example organization website) |
| Mental Health Professionals | Offer professional guidance, therapy, and support for mental health conditions. | (Local directory or online search) |
Societal Awareness and Understanding
Invisible illnesses often go unnoticed, misunderstood, and stigmatized by society. This lack of awareness creates a significant barrier for individuals struggling with these conditions, impacting their access to support, treatment, and even basic acceptance. Promoting societal understanding is crucial for fostering empathy, compassion, and inclusivity.
The Importance of Empathy and Compassion
Empathy and compassion are fundamental to building a supportive society for individuals with invisible illnesses. Understanding that these illnesses are real and impactful is paramount. When we show empathy, we acknowledge the struggles and experiences of those living with invisible conditions, validating their pain and challenges. Compassion extends beyond empathy, involving a genuine desire to help and support.
This includes offering practical assistance, actively listening to concerns, and promoting a sense of belonging.
The Role of Education in Combating Stigma and Misinformation
Education plays a vital role in dismantling stigma and addressing misinformation surrounding invisible illnesses. Raising awareness about these conditions, including their symptoms, causes, and treatments, helps to dispel myths and misconceptions. Education initiatives can target various groups, from the general public to healthcare professionals and policymakers. Accessible and accurate information is key to empowering individuals and fostering understanding.
Examples of Promoting Inclusivity and Understanding
Several strategies can foster inclusivity and understanding of invisible illnesses. These include:
- Promoting open and honest conversations about invisible illnesses in schools, workplaces, and communities. These conversations can help normalize these conditions and foster empathy and understanding.
- Creating support groups and networks specifically for individuals with invisible illnesses and their families. These groups provide opportunities for connection, sharing experiences, and receiving support from others facing similar challenges.
- Implementing inclusive policies and practices in healthcare settings. This includes ensuring that individuals with invisible illnesses are treated with respect and dignity and that their needs are adequately addressed.
- Promoting media representation that accurately portrays individuals with invisible illnesses. Accurate portrayals can help challenge stereotypes and foster a more nuanced understanding of these conditions.
Common Misconceptions and the Facts
Misunderstandings about invisible illnesses can lead to isolation and discrimination. Clearing up these misconceptions is essential for promoting understanding and acceptance.
| Common Misconception | Fact |
|---|---|
| Invisible illnesses are not real or are simply a form of malingering. | Invisible illnesses are real medical conditions with demonstrable physical and psychological impacts on the individual’s life. They often require significant effort and coping mechanisms. |
| Individuals with invisible illnesses are simply seeking attention. | Individuals with invisible illnesses are experiencing real pain and suffering. Seeking support and treatment is a necessary step in managing their condition, not a way to gain attention. |
| There are easy cures or quick fixes for invisible illnesses. | Invisible illnesses often require ongoing management and treatment. There is no one-size-fits-all solution, and treatment plans may vary depending on the individual’s specific needs. |
| Invisible illnesses only affect certain demographics. | Invisible illnesses affect people of all ages, backgrounds, and socioeconomic statuses. They are not limited to specific groups. |
Resources and Support
Navigating an invisible illness can feel isolating. Understanding the available resources and support networks is crucial for managing the condition and improving quality of life. Finding the right support can make a significant difference in coping with the challenges and fostering a sense of community.Many individuals with invisible illnesses face challenges accessing the support they need. Lack of understanding from healthcare professionals, family, or friends can exacerbate feelings of isolation and make it harder to advocate for oneself.
Recognizing the importance of support systems, both formal and informal, is vital for successful management and well-being.
Understanding invisible illnesses can be tough, but it’s crucial. A lot of people are affected, and unfortunately, risky behaviors like the recent rise in flavored tobacco use among teens ( flavored tobacco use rising again among teens ) can exacerbate existing health conditions or create new ones. Ultimately, knowledge and awareness are key to supporting those navigating these complex health journeys.
Reputable Organizations and Resources
Finding reliable organizations and resources is key to getting the right support. These organizations often offer valuable information, advocacy, and direct assistance. They can connect individuals with necessary services and provide a sense of community. Reputable organizations usually have a proven track record and transparent processes.
- National Alliance on Mental Illness (NAMI): NAMI is a prominent organization dedicated to mental health awareness, advocacy, and support. They offer a wealth of information, resources, and support groups for individuals with mental health conditions and their families. They provide educational materials, workshops, and online forums, fostering a supportive environment for those facing mental health challenges.
- The Chronic Illness Network: This network offers a vast array of resources and support for individuals experiencing chronic illnesses, including those with invisible illnesses. They provide access to information, support groups, and advocacy initiatives, connecting individuals with similar experiences. This includes comprehensive information on navigating the healthcare system, advocacy strategies, and coping mechanisms.
- The Invisible Illness Network: This network is a community-driven initiative dedicated to supporting individuals living with invisible illnesses. It provides a platform for sharing experiences, connecting with others, and advocating for better recognition and understanding of these conditions.
Support Groups and Online Communities
Support groups and online communities provide invaluable opportunities for connection and shared experience. They offer a space to share stories, offer advice, and gain insights from others facing similar challenges. These networks can be especially helpful in navigating the complexities of living with an invisible illness.
- Support groups, whether in-person or online, can provide a safe and understanding environment for sharing experiences and finding support. These groups can offer practical advice, emotional support, and a sense of community, which is vital in navigating the challenges of an invisible illness.
- Online communities and forums dedicated to specific invisible illnesses can connect individuals with a shared understanding and experience. These online platforms offer a space to connect with others, ask questions, and share personal stories. This can be a valuable resource for finding practical advice and support in managing the condition.
Professional Guidance and Medical Support
Seeking professional guidance is a critical component of managing an invisible illness. Healthcare professionals play a pivotal role in diagnosis, treatment, and overall well-being. Open communication and collaboration between patients and medical professionals are essential for effective management.
- Medical professionals can play a significant role in diagnosing and treating invisible illnesses. They can offer guidance on symptom management, treatment options, and strategies for managing the condition effectively.
- Seeking professional guidance is vital for accurate diagnosis and effective management of an invisible illness. This often involves working with specialists, therapists, and other healthcare providers.
Helpful Resources
| Website | Support Group | Hotline |
|---|---|---|
| The National Institute of Neurological Disorders and Stroke (NINDS) | Local support groups for Fibromyalgia | The National Suicide Prevention Lifeline |
| The Mayo Clinic | Online Crohn’s and Colitis Support Groups | The Crisis Text Line |
| The Centers for Disease Control and Prevention (CDC) | Online Multiple Sclerosis Support Groups | The Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline |
Case Studies and Examples: What You Should Know About Invisible Illness
Understanding invisible illnesses requires more than just definitions and statistics. It demands a look at the lived experiences of those affected. Real-life case studies provide valuable insight into the challenges and triumphs of managing these conditions, illuminating the impact on daily life and the effectiveness of various treatment approaches. This section explores individual journeys to highlight the importance of personal narratives in fostering empathy and understanding.
Individual Journeys and Experiences
Chronic fatigue syndrome (CFS), fibromyalgia, and multiple chemical sensitivities are just a few examples of invisible illnesses that significantly impact daily life. Each individual’s experience is unique, yet common themes emerge, such as the struggle to be believed, the emotional toll of fluctuating symptoms, and the need for consistent support.
- Sarah’s Story: Sarah, diagnosed with fibromyalgia, initially faced skepticism from healthcare professionals. The pain, fatigue, and cognitive difficulties made it challenging to maintain employment and social connections. Through advocacy, she found a supportive community and discovered a holistic approach combining medication, physical therapy, and mindfulness practices. This allowed her to manage symptoms effectively and regain a sense of normalcy.
- David’s Experience: David, living with multiple chemical sensitivities (MCS), navigated a world of environmental triggers. His journey involved meticulous avoidance strategies, including specific dietary restrictions and carefully curated living spaces. Despite the limitations, David discovered a strong sense of resilience and a deep understanding of his body’s needs. He became an advocate for others with MCS, sharing his experiences and empowering others to manage their conditions.
- Emily’s Perspective: Emily, diagnosed with chronic fatigue syndrome (CFS), highlights the significant emotional burden of invisible illness. The unpredictability of symptoms, the frequent misunderstandings, and the struggle to communicate her needs took a toll on her mental health. However, joining a support group and developing coping mechanisms helped her build a sense of community and navigate the challenges with greater resilience.
Impact of Treatment Approaches
The effectiveness of treatment varies greatly depending on the individual and the specific condition. A multidisciplinary approach often yields the best results, combining medical interventions with lifestyle adjustments.
- Medication Management: While medication can help manage symptoms, it’s crucial to acknowledge that there is no one-size-fits-all approach. Some individuals find relief through specific medications, while others require a combination of drugs. The journey often involves trial and error to discover what works best.
- Alternative Therapies: Many individuals find comfort and symptom relief through alternative therapies like acupuncture, massage therapy, or mindfulness practices. These approaches can complement conventional medicine and help improve overall well-being.
- Lifestyle Adjustments: Making adjustments to daily routines, including dietary changes, stress management techniques, and regular exercise, can significantly impact symptom management. However, these adjustments must be tailored to the individual’s specific needs and tolerances.
Importance of Individual Experiences
Recognizing the individuality of each experience is critical to fostering empathy and understanding. By listening to personal narratives, we gain a deeper appreciation for the complexities of invisible illness and the challenges faced by those living with these conditions.
Understanding invisible illnesses is crucial, as symptoms aren’t always visible. For example, a recent study highlights that a low dose aspirin daily use could increase cancer risk for seniors, a low dose aspirin daily use could increase cancer risk for seniors. This underscores the importance of personalized medical advice and the need to discuss potential risks and benefits with your doctor, regardless of the condition.
Ultimately, knowing what to expect and seek professional help is key to managing invisible illnesses effectively.
Case Study Summary Table
| Case Study | Invisible Illness | Challenges | Successes |
|---|---|---|---|
| Sarah | Fibromyalgia | Skepticism from healthcare professionals, difficulty maintaining employment and social life | Found a supportive community, discovered a holistic approach combining medication, physical therapy, and mindfulness |
| David | Multiple Chemical Sensitivities | Environmental triggers, limitations in daily life, dietary restrictions | Developed resilience, understanding of his body’s needs, became an advocate for others |
| Emily | Chronic Fatigue Syndrome | Unpredictable symptoms, frequent misunderstandings, struggle to communicate needs, emotional burden | Joined a support group, developed coping mechanisms, built a sense of community |
Illustrative Examples
Understanding invisible illnesses requires more than just definitions; it demands empathy and a glimpse into the lived experiences of those affected. This section provides concrete examples to illustrate the challenges and complexities of living with conditions like fibromyalgia and chronic fatigue syndrome, while highlighting the impact of societal biases.
A Day in the Life with Fibromyalgia
Imagine Sarah, a 35-year-old woman living with fibromyalgia. The chronic pain, widespread and often unpredictable, impacts every aspect of her life. Morning brings a wave of aching muscles, making even simple tasks like getting out of bed excruciating. Throughout the day, subtle but persistent pain radiates from her joints, interfering with her work as a teacher. Her energy levels fluctuate dramatically; some days she can barely make it through a class, while others leave her exhausted and needing rest.
Even seemingly insignificant activities, like carrying groceries or climbing stairs, can trigger intense pain and exhaustion. The constant struggle with pain and fatigue affects her relationships and social life, as she often needs to cancel plans or withdraw from social activities. Treatment options, including medication and physical therapy, often provide only partial relief, and managing the unpredictable nature of the illness is a daily battle.
Symptoms, Impact, and Treatment Approaches for Fibromyalgia
Fibromyalgia is characterized by widespread pain, fatigue, sleep disturbances, and cognitive difficulties. The pain is often described as a deep, aching pain, affecting multiple areas of the body. This constant pain can lead to significant emotional distress and anxiety. The fatigue associated with fibromyalgia is often debilitating, impacting daily functioning and productivity. Sleep disturbances, including difficulty falling asleep, staying asleep, and experiencing restless sleep, exacerbate the symptoms.
Cognitive difficulties, such as difficulty concentrating, remembering, and processing information, can further complicate daily life. Treatment approaches for fibromyalgia often involve a multidisciplinary approach, including medication, physical therapy, cognitive behavioral therapy (CBT), and lifestyle modifications. Medication may include pain relievers, antidepressants, or anti-seizure medications. Physical therapy can help manage pain and improve mobility. CBT can help manage stress and improve coping mechanisms.
Lifestyle modifications, such as regular exercise, a healthy diet, and stress management techniques, are crucial in managing the condition.
Chronic Fatigue Syndrome: A Detailed Description
Chronic fatigue syndrome (CFS) is characterized by extreme and persistent fatigue that is not relieved by rest. It’s a debilitating condition that significantly impacts a person’s ability to carry out daily tasks. Common symptoms include profound fatigue, sleep disturbances, cognitive difficulties, muscle pain, headaches, and a heightened sensitivity to light and sound. These symptoms can fluctuate in severity, sometimes worsening after physical or mental exertion.
The debilitating fatigue can significantly restrict daily activities, making work, school, and social interactions difficult or impossible. Treatment approaches for CFS often involve a combination of therapies, including medication to address specific symptoms, and lifestyle changes aimed at improving overall health and well-being. Support groups and counseling can also be invaluable in managing the emotional and psychological toll of the condition.
Societal Biases Affecting Individuals with Invisible Illnesses
Societal biases against invisible illnesses often manifest as skepticism, disbelief, or lack of understanding from family, friends, employers, and even healthcare providers. This lack of understanding can lead to isolation, discrimination, and a diminished quality of life for those affected. For example, individuals may be dismissed as “faking” their illness, or their symptoms may be attributed to laziness or a lack of willpower.
This can result in difficulty obtaining necessary support or treatment, and it can lead to feelings of isolation and hopelessness. These biases contribute to the significant challenges faced by individuals living with invisible illnesses. Accurate information and increased societal awareness are critical in fostering understanding and empathy.
Misunderstandings and the Need for Accurate Information
Misunderstandings about invisible illnesses can arise from a lack of awareness and empathy. For instance, a person with chronic fatigue syndrome might be told to “just get over it” or “try harder.” Such statements not only invalidate their experience but also contribute to feelings of isolation and stigmatization. The need for accurate information and support cannot be overstated.
Educating others about the complexities of invisible illnesses is crucial in fostering understanding and empathy, and in helping to reduce the stigma and isolation experienced by those affected.
Conclusion
In conclusion, understanding invisible illness requires a shift in perspective, moving beyond assumptions and misconceptions. This exploration highlights the importance of accurate information, empathy, and support for those living with these conditions. By fostering greater awareness and understanding, we can create a more inclusive and supportive environment for everyone.