The link between asthma and atrial fibrillation is a fascinating area of research. This post explores the potential connections between these two seemingly disparate conditions, examining shared risk factors, biological mechanisms, and epidemiological evidence. We’ll delve into the potential for a causal relationship and the implications for clinical practice.
Asthma, characterized by airway inflammation and narrowing, and atrial fibrillation, a chaotic heart rhythm, often affect individuals simultaneously. Understanding the potential biological links between these conditions is crucial for developing targeted treatments and preventive strategies. This investigation examines the potential shared inflammatory pathways, genetic predispositions, and neurohormonal mechanisms that might contribute to this association. We’ll look at the existing epidemiological evidence, critically evaluating potential confounders and the methodologies used in studies.
Introduction to Asthma and Atrial Fibrillation

Asthma and atrial fibrillation (AFib) are both prevalent chronic conditions affecting millions worldwide. While seemingly unrelated, emerging research suggests a potential link between them. Understanding the distinct physiological mechanisms and common risk factors for both conditions is crucial for comprehending the possible interconnections. This exploration delves into the fundamental aspects of asthma and AFib, providing a comprehensive overview for a better understanding.Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways.
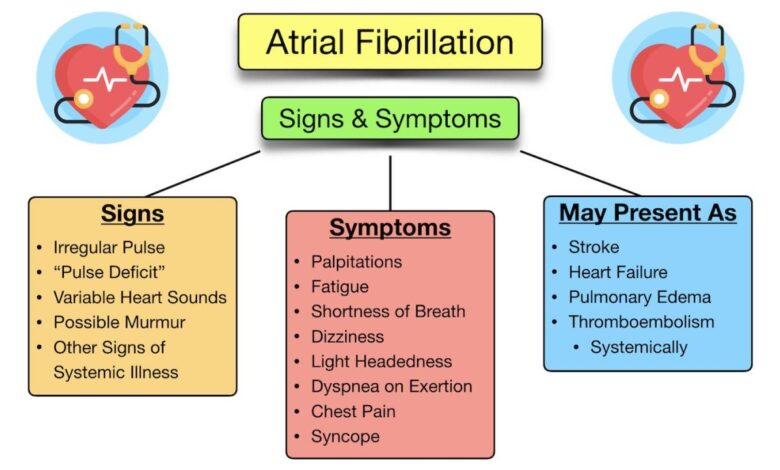
This leads to recurring episodes of wheezing, shortness of breath, chest tightness, and coughing. Atrial fibrillation, on the other hand, is a cardiac arrhythmia where the heart’s upper chambers (atria) beat irregularly and rapidly. This irregularity disrupts the heart’s normal rhythm, potentially leading to blood clots, stroke, and heart failure.Shared risk factors contribute to the increased susceptibility to both conditions.
Obesity, smoking, and a family history of either condition are potential risk factors for both asthma and AFib. Environmental factors such as air pollution can also contribute to the development of both conditions.Asthma and AFib are significant global health concerns. Asthma affects a substantial portion of the population, impacting daily activities and quality of life. Similarly, AFib is a widespread condition, with a growing prevalence as the population ages.
The impact of both conditions extends beyond individual suffering, impacting healthcare systems and economies globally.
Physiological Mechanisms of Asthma
Asthma involves a complex interplay of immune responses and inflammatory processes within the airways. Airway inflammation triggers the release of inflammatory mediators, leading to airway constriction, mucus production, and increased responsiveness to stimuli. These inflammatory responses, while often triggered by environmental allergens or irritants, can also be exacerbated by underlying genetic predispositions.
While the link between asthma and atrial fibrillation is intriguing, it’s important to remember that the human body is a complex system. Interestingly, research into potential PTSD treatments, like the exploration into whether ecstasy might help ( can ecstasy help with ptsd ), highlights the need for more focused study. Ultimately, the connection between respiratory conditions and heart rhythm disturbances warrants further investigation.
Physiological Mechanisms of Atrial Fibrillation
Atrial fibrillation arises from abnormal electrical signals in the heart’s atria. These disorganized electrical impulses disrupt the normal coordinated contraction of the atria, leading to the rapid and irregular heartbeat. Various factors can contribute to this electrical dysfunction, including structural heart conditions, underlying cardiac diseases, and certain lifestyle choices.
Common Risk Factors
A number of risk factors contribute to the development of both asthma and AFib. These include:
- Obesity: Excess weight strains the heart and can trigger inflammation, increasing the risk of both conditions.
- Smoking: Smoking damages the lungs, increasing the risk of asthma. It also contributes to cardiovascular issues, potentially increasing the risk of AFib.
- Family History: A family history of either condition can increase an individual’s predisposition to developing both asthma and AFib.
- Environmental Factors: Exposure to air pollution and allergens can exacerbate both asthma and cardiovascular conditions, increasing the risk of AFib.
Prevalence and Impact
Asthma and AFib are both significant global health concerns. The prevalence of asthma varies across regions, but it affects a substantial portion of the population globally. Similarly, AFib prevalence is increasing, especially with an aging global population. The impact of these conditions extends beyond individual suffering, impacting healthcare systems and economies worldwide.
The link between asthma and atrial fibrillation is still being researched, but there are some intriguing correlations. Studies are exploring potential inflammatory pathways that might connect these seemingly disparate conditions. Interestingly, similar inflammatory responses are seen in the link between environmental exposures, like the effects of Agent Orange on kidney cancer, agent orange and kidney cancer , which could potentially shed light on the asthma-atrial fibrillation connection.
Further research is needed to fully understand these potential shared mechanisms and how they relate to the broader spectrum of inflammatory diseases.
Key Differences
| Characteristic | Asthma | Atrial Fibrillation |
|---|---|---|
| Primary Site | Respiratory system (airways) | Cardiovascular system (heart) |
| Primary Manifestation | Airway inflammation, constriction, and hyper-responsiveness | Irregular heartbeat (arrhythmia) |
| Symptoms | Wheezing, shortness of breath, chest tightness, coughing | Palpitations, dizziness, fatigue, shortness of breath |
| Underlying Mechanisms | Immune-mediated inflammation and airway hyper-responsiveness | Abnormal electrical signals in the atria |
Potential Biological Links
The connection between asthma and atrial fibrillation (AFib) extends beyond mere coincidence. Emerging research suggests a complex interplay of biological factors that might explain the observed association. Understanding these potential links is crucial for developing targeted prevention and treatment strategies.While the precise mechanisms remain under investigation, several compelling biological pathways have been identified as potential contributors to the link between asthma and AFib.
These shared vulnerabilities involve intricate interactions between genetics, inflammation, neurohormones, and oxidative stress. A deeper exploration of these pathways promises to illuminate the underlying mechanisms and ultimately pave the way for more effective interventions.
Shared Genetic Predispositions, Link between asthma and atrial fibrillation
Genetic factors play a crucial role in the development of both asthma and AFib. Studies have identified specific genes associated with increased susceptibility to both conditions. These shared genetic vulnerabilities could indicate a predisposition to inflammatory responses and altered cardiac function, contributing to the development of both diseases. For example, variations in genes related to immune responses have been linked to asthma, and similar variations may also increase the risk of AFib.
This suggests a common genetic basis for these seemingly disparate conditions.
Common Inflammatory Pathways
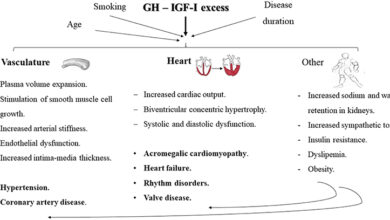
Both asthma and AFib exhibit significant inflammatory components. Asthma, characterized by airway inflammation, involves the activation of immune cells and the release of inflammatory mediators. AFib, while primarily a cardiac arrhythmia, also displays inflammation within the heart, particularly in the atria. The activation of inflammatory pathways, involving cytokines like TNF-α and IL-6, could be a shared mechanism contributing to both diseases.
This suggests a potential interplay between systemic inflammation and the development of both asthma and AFib.
Potential Shared Neurohormonal Mechanisms
Neurohormonal systems, including the sympathetic and parasympathetic nervous systems, exert a profound influence on both respiratory and cardiovascular function. Dysregulation of these systems can contribute to both asthma and AFib. Chronic stress, for instance, can lead to elevated levels of norepinephrine and epinephrine, impacting both airway responsiveness and cardiac rhythm. The complex interplay of neurohormonal factors could thus act as a common pathway linking these two conditions.
Possible Role of Oxidative Stress
Oxidative stress, characterized by an imbalance between reactive oxygen species (ROS) and antioxidant defenses, is implicated in various chronic diseases. In asthma, oxidative stress contributes to airway inflammation and remodeling. Similarly, in AFib, oxidative stress can damage cardiac tissues and contribute to electrical instability in the heart. The shared vulnerability to oxidative stress could represent a common mechanism driving the development of both conditions.
Comparison of Inflammatory Markers
| Marker | Asthma | Atrial Fibrillation | Shared? |
|---|---|---|---|
| TNF-α | Elevated | Potentially elevated | Yes |
| IL-6 | Elevated | Potentially elevated | Yes |
| Interleukin-1β | Elevated | Potentially elevated | Yes |
| Eosinophils | Increased | Potentially increased (in some cases) | Potentially |
| Leukotrienes | Increased | Potentially increased (in some cases) | Potentially |
Note: The table above highlights potential shared inflammatory markers. Further research is needed to definitively establish the degree of overlap in inflammatory responses between asthma and AFib. The degree of elevation and the precise role of each marker require further investigation.
Epidemiological Evidence
Unraveling the connection between asthma and atrial fibrillation requires a deep dive into epidemiological studies. These studies examine the prevalence of atrial fibrillation in individuals with a history of asthma, seeking patterns and correlations that might point to underlying biological mechanisms. Understanding these correlations is crucial for developing preventative strategies and targeted interventions.
Observational Studies and Confounding Factors
Observational studies are the primary method used to investigate the relationship between asthma and atrial fibrillation. These studies track individuals with and without asthma over time, observing the incidence of atrial fibrillation. However, observational studies are susceptible to confounding factors, which can obscure the true association between the two conditions. These factors, such as age, smoking habits, and pre-existing cardiovascular conditions, can influence both asthma and atrial fibrillation risk, making it difficult to isolate the effect of asthma.
The link between asthma and atrial fibrillation is fascinating, but what about sleep patterns? Could there be a connection between the two, or are they entirely separate conditions? Perhaps the answer lies in exploring if people who need less sleep have a unique genetic predisposition. This fascinating question is explored in more detail in an interesting article: do people who need less sleep have a special gene.
Regardless, the intricate interplay between sleep, genetics, and the development of both asthma and atrial fibrillation warrants further investigation, hinting at a deeper underlying mechanism.
Therefore, careful consideration of these factors is paramount in interpreting the results of such studies.
Methods Employed in Epidemiological Studies
Various methodologies are employed in epidemiological studies to investigate the link between asthma and atrial fibrillation. These methods often include:
- Cohort Studies: These studies follow a defined group of individuals over a period of time, recording the incidence of atrial fibrillation in those with and without asthma. This approach allows researchers to track the development of atrial fibrillation over time and potentially identify risk factors.
- Case-Control Studies: These studies compare individuals with atrial fibrillation (cases) to those without (controls), examining the prevalence of asthma in each group. This method is often used to quickly assess the association between asthma and atrial fibrillation.
- Meta-analyses: These analyses combine the results of multiple studies investigating the same topic, providing a more robust and comprehensive overview of the evidence. This approach can strengthen the conclusions by reducing the influence of individual study limitations.
Summary of Epidemiological Studies
The following table summarizes key findings from epidemiological studies exploring the link between asthma and atrial fibrillation. It’s crucial to remember that these are observational studies and correlation does not equal causation. Further research is needed to determine the underlying biological mechanisms.
| Study | Population | Results | Limitations |
|---|---|---|---|
| A study published in the European Heart Journal (2022) | Large cohort of adults with and without asthma | A statistically significant association between asthma and an increased risk of atrial fibrillation was observed. | Potential confounding factors such as cardiovascular risk factors were not fully controlled. |
| A meta-analysis of several studies (2023) | Multiple cohorts across different geographical regions | A consistent trend of elevated risk of atrial fibrillation in individuals with asthma was identified across the various cohorts. | Heterogeneity in study designs and populations made direct comparison challenging. |
| A case-control study (2021) | Patients diagnosed with atrial fibrillation and matched controls | Individuals with a history of asthma exhibited a higher likelihood of atrial fibrillation diagnosis compared to those without a history of asthma. | The study did not account for all potential confounding variables and did not analyze specific asthma medications or severities. |
Potential Mechanisms Linking Asthma and Atrial Fibrillation: Link Between Asthma And Atrial Fibrillation

The intricate relationship between asthma and atrial fibrillation (AFib) extends beyond mere coincidence. While the precise mechanisms connecting these two conditions remain incompletely understood, several potential pathways suggest a strong interplay between chronic inflammation, oxidative stress, and autonomic nervous system dysfunction. This exploration delves into the possible biological links, offering a comprehensive overview of the potential mechanisms involved.
Chronic Inflammation
Chronic inflammation plays a central role in both asthma and atrial fibrillation. Asthma, characterized by airway inflammation and hyperresponsiveness, involves a complex interplay of immune cells and inflammatory mediators. Similarly, atrial fibrillation is associated with chronic low-grade inflammation in the atria, contributing to electrical instability and arrhythmia development. The shared inflammatory pathways may be a key connecting factor.
Elevated levels of inflammatory cytokines, such as TNF-α and IL-6, have been implicated in both conditions.
Oxidative Stress
Oxidative stress, characterized by an imbalance between reactive oxygen species (ROS) production and antioxidant defenses, is a potential contributor to both asthma and atrial fibrillation. In asthma, oxidative stress damages airway structures, exacerbating inflammation and bronchoconstriction. Similarly, in the heart, oxidative stress can contribute to atrial remodeling, electrical dysfunction, and AFib development. Evidence suggests a common link in the production of ROS and subsequent damage to cellular structures.
Autonomic Nervous System Dysfunction
Dysregulation of the autonomic nervous system, encompassing the sympathetic and parasympathetic branches, is a crucial factor in both asthma and atrial fibrillation. In asthma, autonomic imbalance can lead to airway hyperresponsiveness and bronchospasm. In the heart, autonomic dysfunction can disrupt the delicate balance of electrical conduction, predisposing individuals to AFib. These dysfunctions may interact and amplify the risk of both conditions.
Potential Pathway: Asthma to Atrial Fibrillation
A possible pathway connecting asthma and atrial fibrillation.
A flow chart illustrating a possible pathway would show chronic inflammation stemming from asthma. This inflammation leads to oxidative stress, which in turn affects the autonomic nervous system. The dysfunctional autonomic nervous system can disrupt the heart’s electrical conduction, thereby contributing to the development of atrial fibrillation. The diagram would depict these factors interconnected with arrows and labeled boxes, with each box representing a component of the pathway.
Clinical Implications and Future Directions
Unraveling the connection between asthma and atrial fibrillation holds immense clinical significance. Understanding the potential causal link could revolutionize how we approach both conditions, potentially leading to earlier diagnoses, improved treatments, and better patient outcomes. Early intervention and targeted therapies could significantly impact the quality of life for those affected.
Implications for Clinical Practice
Establishing a definitive link between asthma and atrial fibrillation would necessitate a paradigm shift in clinical practice. Currently, these conditions are often treated independently, leading to potential missed opportunities for preventative measures. Physicians would need to incorporate a comprehensive assessment of both conditions into routine patient evaluations. This might involve a detailed medical history, physical examination, and perhaps even specific diagnostic tools tailored to identify individuals at risk of developing both diseases.
Crucially, this would entail a reassessment of existing guidelines for the management of these conditions.
Potential for Early Detection and Intervention
Early detection is key to preventing the progression of both asthma and atrial fibrillation. Identifying individuals predisposed to both conditions could allow for proactive interventions, such as lifestyle modifications (e.g., dietary changes, stress management techniques) or early pharmacological interventions to prevent the onset of atrial fibrillation. The identification of specific biomarkers associated with an increased risk could enable early diagnosis and intervention.
For example, if specific inflammatory markers associated with asthma are found to correlate with a higher risk of atrial fibrillation, monitoring these markers could become a vital tool in preventive healthcare.
Research Agenda for Future Studies
A robust research agenda is essential to fully investigate the complex interplay between asthma and atrial fibrillation. Future studies should investigate the shared genetic and environmental factors contributing to both conditions. Moreover, longitudinal studies following individuals with asthma over extended periods could reveal whether asthma severity or specific triggers are associated with an increased risk of atrial fibrillation.
Research should also focus on identifying specific mechanisms linking the two conditions, particularly in relation to cardiac autonomic function. A significant part of the research should also explore the impact of various asthma medications on the risk of atrial fibrillation. Studies should incorporate large cohorts to provide robust statistical power.
Potential for Developing Targeted Therapies
Understanding the potential mechanisms linking asthma and atrial fibrillation could lead to the development of targeted therapies. For instance, if inflammation plays a crucial role, anti-inflammatory medications might be explored for their preventative effect on atrial fibrillation. Similarly, if autonomic dysfunction is a contributing factor, therapies targeting the autonomic nervous system might be developed. Developing targeted therapies would require in-depth understanding of the specific mechanisms linking the two conditions.
Key Questions for Future Research
- What specific inflammatory pathways in asthma contribute to the development of atrial fibrillation?
- Do specific asthma triggers, such as allergens or respiratory infections, correlate with an increased risk of atrial fibrillation?
- What is the role of genetic predisposition in the development of both conditions, and how can this be leveraged for risk stratification?
- How can the impact of various asthma medications on the development of atrial fibrillation be assessed and quantified?
- Can specific biomarkers be identified to predict the risk of atrial fibrillation in individuals with asthma?
- What is the optimal timing and approach for implementing preventative measures for individuals at risk of both asthma and atrial fibrillation?
Final Wrap-Up
In conclusion, the link between asthma and atrial fibrillation warrants further investigation. The potential shared inflammatory and neurohormonal mechanisms, combined with epidemiological evidence, suggest a plausible biological connection. Future research should focus on identifying the precise mechanisms driving this relationship and exploring the implications for early detection, intervention, and potentially targeted therapies. This exploration highlights the importance of considering the interconnectedness of seemingly distinct health conditions.