Depression the growing american mental health storm – Depression: The growing American mental health storm is a complex issue affecting millions across the country. This article delves into the multifaceted nature of depression, exploring its prevalence, causes, and impact on various demographics. From defining the phenomenon and analyzing historical trends, to examining access to treatment and potential solutions, we aim to shed light on this pressing concern.
The rising rates of depression within the American population are alarming, highlighting the urgent need for comprehensive understanding and effective interventions. We will examine the social, economic, psychological, and environmental factors that contribute to this growing mental health crisis, using data and real-world examples to illustrate the severity and scope of the problem.
Defining the Phenomenon
Depression, a pervasive mental health challenge, significantly impacts the American population. It’s characterized by persistent sadness, loss of interest in activities, and a range of other emotional and physical symptoms. Understanding the nuances of this experience within the American context, including historical trends, contributing factors, and demographic variations, is crucial for effective intervention and support.The experience of depression in America is multifaceted, shaped by a complex interplay of social, economic, psychological, and environmental factors.
While the core symptoms remain consistent, the manifestation and impact of depression can differ based on an individual’s background and circumstances. Recognizing these variations is essential for tailoring appropriate support and treatment strategies.
Defining Depression in the American Context
Depression in America is broadly defined as a mood disorder characterized by persistent feelings of sadness, hopelessness, and loss of interest in activities. This encompasses a spectrum of severity, from mild to severe, and can significantly impair daily functioning. Crucially, this definition acknowledges the American cultural context, where societal pressures, economic anxieties, and unique personal experiences can all contribute to the expression of depressive symptoms.
Key Characteristics and Symptoms
Depression manifests in various ways, affecting individuals differently. Common symptoms include persistent sadness, loss of interest in previously enjoyed activities, changes in appetite or sleep patterns, fatigue, feelings of worthlessness or guilt, difficulty concentrating, and recurrent thoughts of death or suicide. In the American context, these symptoms can be further nuanced by the pressures of a fast-paced, achievement-oriented society, potentially leading to feelings of inadequacy or failure.
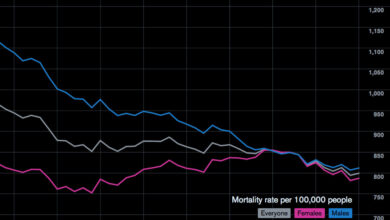
Historical Trends in Depression Rates
Historical data reveals fluctuations in depression rates within the US. While precise figures vary depending on the era and methodology of measurement, studies suggest an upward trend in recent decades. This trend aligns with increasing societal stressors and evolving diagnostic criteria. The rise of social media and its potential impact on self-perception and mental well-being is a factor worth noting.
Contributing Factors to Rising Rates
The rising rates of depression in America are a complex issue with multiple contributing factors. These factors include economic instability, social isolation, increasing pressure to conform to societal ideals, and evolving cultural norms. The increasing emphasis on productivity and achievement in American culture can contribute to feelings of inadequacy and pressure. The influence of social media on self-esteem and mental well-being is another significant area for consideration.
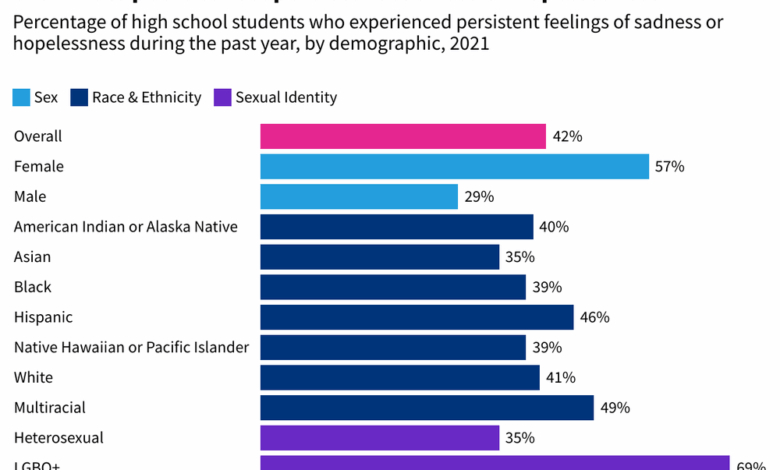
Demographic Variations in Depression Experience
The experience of depression varies significantly across different demographics within the US. Factors like race, ethnicity, socioeconomic status, and geographic location can all influence the presentation and impact of depressive symptoms. For example, marginalized communities may face additional stressors related to systemic discrimination, further exacerbating the risk of depression. Studies show disparities in access to mental health care across these groups, which can further complicate treatment and recovery.
Factors Contributing to Depression
| Social | Economic | Psychological | Environmental |
|---|---|---|---|
| Social isolation, pressure to conform, societal expectations, lack of social support | Financial insecurity, unemployment, economic hardship, job loss | Low self-esteem, negative self-talk, anxiety, trauma, lack of coping mechanisms | Exposure to violence, natural disasters, climate change impacts, environmental toxins |
Prevalence and Impact
Depression, a pervasive mental health challenge, significantly impacts individuals, families, and society. Understanding its prevalence across different demographics and its far-reaching consequences is crucial for developing effective interventions and support systems. The economic burden of depression is substantial, affecting productivity, healthcare costs, and the overall well-being of the nation.The current landscape of depression in America reveals a complex picture of varying prevalence across age groups and socioeconomic strata.
Depression is a growing concern in the US, impacting countless lives. While it’s a serious mental health issue, sometimes physical discomfort can also overlap with emotional struggles. For example, understanding when round ligament pain starts during pregnancy can be crucial for expectant mothers when does round ligament pain start , but it’s important to remember that these physical symptoms don’t negate the serious impact of depression on overall well-being.
The mental health crisis demands our attention and resources, and we need to support those struggling with these conditions.
Factors like access to mental health care, cultural influences, and individual experiences all play a role in shaping the experience of depression. The societal impact of depression is multi-faceted, affecting not only the individuals struggling with the illness but also their families and communities.
Prevalence Rates by Age Group
Understanding the age-specific prevalence of depression helps tailor interventions and support strategies to meet the needs of different populations. Different age groups experience depression with varying rates and manifestations. For example, adolescents face unique challenges in navigating their emotional landscape, often leading to a higher risk of depression compared to younger children. Conversely, older adults may experience depression in conjunction with other health concerns, potentially masking its symptoms.
- Adolescents (ages 13-18): Studies suggest a significant prevalence rate, often linked to social pressures, academic demands, and identity formation.
- Young Adults (ages 19-25): Transitioning to adulthood can be a stressful time, contributing to higher rates of depression in this age group.
- Adults (ages 26-64): While prevalence may vary depending on life circumstances, this group encompasses a diverse range of experiences, from career challenges to family responsibilities.
- Older Adults (ages 65+): Depression in older adults often co-occurs with other health conditions, potentially leading to underdiagnosis or misdiagnosis.
Socioeconomic Disparities in Prevalence
Economic factors significantly influence the experience and prevalence of depression. Individuals from lower socioeconomic backgrounds may face increased risk due to factors like limited access to resources, job insecurity, and exposure to chronic stress. Addressing these disparities is essential to promoting equitable mental health care.
- Lower Socioeconomic Status: Individuals with lower incomes and fewer resources often experience higher rates of depression due to financial stress, limited access to healthcare, and lack of social support.
- Higher Socioeconomic Status: While not immune, individuals with higher incomes may face different stressors, such as career pressures and maintaining a demanding lifestyle, which can also contribute to depression.
Societal and Economic Impact
Depression has profound societal and economic implications, impacting individuals, families, and the overall American workforce. Lost productivity, increased healthcare costs, and the strain on social support systems are all significant concerns. These costs are not simply monetary but also encompass the human toll of suffering and diminished quality of life.
Depression is a growing storm in American mental health, affecting millions. The interplay between our mental well-being and physical health is increasingly clear, and factors like gut bacteria and liver health are now understood to play a critical role. Recent research has shown a strong correlation between imbalances in gut bacteria and potential liver damage, which could indirectly impact mental health.
This raises the critical question of whether addressing issues like gut bacteria liver damage could be a part of the solution to the growing mental health crisis. Ultimately, understanding the intricate connections between our bodies and minds is key to tackling depression effectively.
- Lost Productivity: Depression significantly impacts work performance, resulting in absenteeism, presenteeism (attending work but not being productive), and reduced job satisfaction. This lost productivity directly affects businesses and the overall economy.
- Increased Healthcare Costs: Depression often necessitates treatment with medication, therapy, and other medical interventions, driving up healthcare expenditures. This places a burden on both individuals and the healthcare system.
- Strain on Families: Depression affects family dynamics, relationships, and overall well-being. The emotional toll on family members can be substantial, requiring significant support and understanding.
Impact on Education and Healthcare Systems
Depression can significantly disrupt the educational experience for individuals, impacting academic performance, attendance, and overall well-being. Similarly, the healthcare system faces a significant challenge in addressing the growing need for mental health services.
- Education: Students experiencing depression may struggle with concentration, motivation, and attendance, hindering their academic progress. Early intervention and support systems are critical to minimizing the impact on educational outcomes.
- Healthcare: The increasing prevalence of depression necessitates enhanced mental health services within the healthcare system. This includes expanding access to mental health professionals, increasing awareness among primary care physicians, and promoting preventative measures.
Economic Costs of Depression
The economic burden of depression is substantial, encompassing lost productivity and healthcare expenses. These costs vary depending on factors like treatment duration and the severity of the condition. Quantifying these costs is crucial for allocating resources and developing effective strategies for prevention and intervention.
| Category | Estimated Cost (in USD billions) |
|---|---|
| Lost Productivity | ~100-150 |
| Healthcare Expenses | ~70-100 |
| Total Estimated Cost | ~170-250 |
Regional Variations in Depression Prevalence
The prevalence of depression varies across different regions of the US, reflecting diverse social, economic, and environmental factors. This variation underscores the need for region-specific strategies to address mental health disparities.
Depression is a growing storm in American mental health, impacting countless lives. It’s a serious issue, and unfortunately, sometimes intertwined with addiction. Finding support and resources is crucial, and for me personally, suboxone helped me overcome addiction , demonstrating that recovery is possible. This underscores the importance of open conversations and accessible resources for those struggling with mental health challenges.
| Region | Estimated Prevalence Rate (percentages) |
|---|---|
| Northeast | ~6-8% |
| Midwest | ~7-9% |
| South | ~6-8% |
| West | ~7-10% |
Causes and Risk Factors

Depression is a complex mental health condition, and its origins are rarely a single, isolated cause. Instead, a multitude of factors, interacting in intricate ways, contribute to its development. Understanding these factors is crucial for prevention and effective treatment. This section delves into the potential interplay of genetics, environment, and lifestyle choices, as well as societal influences and their impact on depression rates.A comprehensive understanding of the interplay between various factors, such as genetics, environment, and lifestyle choices, is essential for developing effective strategies to prevent and treat depression.
It’s not merely about identifying risk factors but also about recognizing the complex web of interactions that contribute to the development of this condition.
Genetic Predisposition
Genetic factors play a significant role in vulnerability to depression. Research indicates that individuals with a family history of depression are more likely to experience the condition themselves. This doesn’t mean that genetics dictate destiny; rather, it highlights a predisposition that can be influenced by environmental and lifestyle factors. For example, a person with a genetic predisposition might not develop depression if they have a supportive social network and healthy coping mechanisms.
Environmental Influences
Environmental stressors significantly impact mental well-being. Traumatic events, such as abuse, loss, or significant life changes, can increase the risk of developing depression. Furthermore, chronic stress from challenging environments, including poverty, discrimination, or exposure to violence, can also contribute to the development of depressive symptoms.
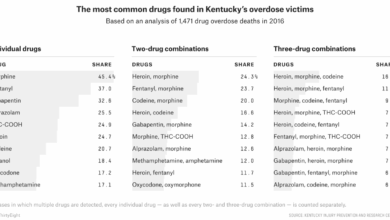
Lifestyle Choices and Behaviors
Lifestyle choices and behaviors, such as poor diet, lack of exercise, and substance abuse, can exacerbate mental health issues. For example, individuals with unhealthy lifestyle choices might find themselves more vulnerable to stress and less equipped to cope with life’s challenges, potentially leading to depression.
Risk Factors Categorized
Understanding the diverse risk factors for depression is crucial for early intervention and prevention. The following factors are categorized for clarity.
- Biological Factors: These include genetic predisposition, brain chemistry imbalances, and chronic medical conditions. For instance, individuals with certain hormonal imbalances, such as those experienced during menopause or postpartum, might experience increased vulnerability to depressive episodes.
- Environmental Factors: Traumatic experiences, chronic stress, exposure to violence, and challenging living conditions are prominent examples of environmental stressors that can contribute to the development of depression. A child growing up in an unstable home environment, for example, might develop coping mechanisms that increase their risk for depression in adulthood.
- Psychological Factors: These encompass factors like low self-esteem, negative thought patterns, and a history of mental health issues. An individual who consistently views themselves negatively and lacks confidence might be more susceptible to depression when faced with adversity.
- Social Factors: Social isolation, lack of social support, and difficult interpersonal relationships can all contribute to a higher risk of depression. For example, individuals experiencing significant social isolation during a period of transition or grief might struggle to cope, increasing their vulnerability to depressive symptoms.
Societal Factors
Societal factors are increasingly recognized as influential factors in the rising rates of depression. Economic hardship, social inequalities, and lack of access to mental health resources are crucial contributors.
Socioeconomic Disparities
Socioeconomic disparities significantly impact mental health outcomes. Individuals from lower socioeconomic backgrounds often face greater stressors, including poverty, unemployment, and limited access to healthcare, increasing their vulnerability to depression.
Social Media and Technology
The increasing prevalence of social media and technology has introduced new avenues for both connection and disconnection. While social media can provide a sense of community, it can also contribute to feelings of inadequacy, comparison, and social isolation, potentially increasing the risk of depression, especially among vulnerable populations.
Correlation Between Life Events and Likelihood of Depression
| Life Event | Likelihood of Depression |
|---|---|
| Death of a loved one | High |
| Job loss | Moderate |
| Major relationship problems | Moderate |
| Financial difficulties | Moderate |
| Moving to a new city | Low |
| Graduation | Low |
Access to Treatment and Support

Navigating the complexities of mental health, especially depression, often hinges on access to effective treatment and supportive resources. Unfortunately, the American landscape presents significant disparities in this area, impacting individuals’ ability to seek help and recover. The challenges extend beyond affordability, encompassing cultural stigmas, geographical limitations, and a shortage of trained professionals. This necessitates a deeper look into the available options and their effectiveness.The current system faces a formidable task in ensuring equitable access to mental healthcare.
Barriers like insurance coverage, lack of awareness about resources, and geographical isolation prevent many from receiving the care they need. Moreover, the stigma surrounding mental illness often discourages individuals from seeking help, perpetuating a cycle of untreated suffering.
Current Access to Mental Healthcare Services in America
Access to mental healthcare in America is unevenly distributed, with significant disparities across demographics and geographic locations. Rural areas often lack sufficient mental health professionals, leading to longer wait times and limited options for treatment. Financial limitations also pose a significant barrier, as insurance coverage for mental health services can be inadequate or nonexistent for many. Cultural stigmas further hinder individuals from seeking help, as mental health issues are sometimes viewed with shame and judgment.
This can lead to individuals delaying or avoiding treatment altogether.
Treatment Options for Depression
Various treatment options are available for depression, ranging from psychotherapy to medication. The effectiveness of these approaches can vary depending on the individual and the severity of their condition.
Effectiveness of Different Therapeutic Approaches
Different therapeutic approaches demonstrate varying degrees of effectiveness in treating depression. Cognitive Behavioral Therapy (CBT) is a widely used and often highly effective method. It helps individuals identify and challenge negative thought patterns and behaviors, leading to improved mood and coping mechanisms. Other evidence-based therapies, such as interpersonal therapy (IPT) and dialectical behavior therapy (DBT), also offer valuable strategies for managing depression.
The selection of a specific approach often depends on the individual’s specific needs and preferences, as well as the expertise of the therapist.
Role of Support Systems
Strong support systems play a crucial role in mitigating the impact of depression. Family, friends, and support groups provide invaluable emotional and practical assistance, reducing feelings of isolation and loneliness. These systems can offer encouragement, understanding, and a sense of belonging, which can be vital in the recovery process.
Mental Health Professionals
| Type of Professional | Description |
|---|---|
| Psychiatrist | Medical doctors specializing in mental health, able to prescribe medication. |
| Psychologist | Trained in the assessment, diagnosis, and treatment of mental health conditions through therapy. |
| Licensed Clinical Social Worker (LCSW) | Trained in social work and mental health, providing therapy and support. |
| Licensed Marriage and Family Therapist (LMFT) | Specializes in family and relationship issues, providing therapy for individuals and couples. |
| Psychiatric Nurse Practitioner (PNP) | Registered nurses with advanced training in psychiatry, able to diagnose and treat mental health conditions. |
Public Awareness and Policy
Public awareness of mental health issues, particularly depression, is a critical factor in destigmatizing the condition and encouraging help-seeking behavior. However, despite increasing recognition, significant gaps remain in understanding the nuances of depression and its impact on individuals and society. This lack of comprehensive understanding often hinders the development and implementation of effective mental health policies.Current mental health policies in the United States aim to improve access to care, but their effectiveness varies significantly.
Existing legislation often focuses on specific populations, like children or veterans, or addresses particular aspects of mental healthcare, such as insurance coverage. However, a holistic approach that considers the needs of all individuals and communities is still lacking. The effectiveness of these policies is often measured by factors such as the rate of mental health diagnoses, the availability of mental health professionals, and the overall satisfaction of individuals accessing services.
These metrics are not always easily comparable, making it difficult to assess the true impact of existing policies.
Current Public Awareness of Depression and Mental Health
Public awareness of depression and mental health issues in America has significantly increased in recent years. Increased media coverage, celebrity endorsements of mental health initiatives, and open conversations in social media have all contributed to this rise in awareness. However, stigma remains a significant barrier to seeking help, with many individuals still feeling ashamed or embarrassed to admit they are struggling with mental health issues.
This can manifest as a reluctance to seek professional help, or a hesitancy to talk about personal experiences with mental illness with friends and family.
Existing Mental Health Policies and Their Effectiveness
A variety of mental health policies are in place across the US, but their effectiveness varies widely. Federal and state-level legislation impacts insurance coverage, funding for mental health services, and access to care in different sectors. Examples include provisions mandating mental health coverage in health insurance plans, funding initiatives for early intervention programs, and support for community-based mental health services.
Potential Strategies for Increasing Public Awareness and Promoting Mental Well-being
Education campaigns targeting diverse communities and demographics are crucial. These campaigns can focus on dispelling myths about mental illness, promoting early intervention, and providing accurate information about available resources. Collaboration with community leaders, influencers, and organizations dedicated to mental health awareness can amplify the reach of these campaigns. For example, incorporating mental health awareness into school curricula, workplace training, and community events can contribute to creating a supportive and understanding environment for individuals facing mental health challenges.
Potential Policy Changes to Improve Access to Mental Healthcare
Expanding access to affordable mental healthcare is paramount. This includes addressing the shortage of mental health professionals, especially in underserved communities. Policy changes could include funding for training programs for mental health professionals, scholarships for graduate programs in psychology and related fields, and incentivizing mental health professionals to practice in underserved areas. Increasing insurance coverage for mental health services, lowering out-of-pocket costs, and promoting telemedicine options can also significantly improve access to care.
Table of Current Mental Health Policies and Their Effectiveness
| Policy Area | Policy Description | Effectiveness (Qualitative Assessment) |
|---|---|---|
| Insurance Coverage | Mandates mental health coverage in insurance plans. | Mixed. Coverage varies significantly by plan type and state regulations. |
| Funding for Services | Allocates funds for mental health programs at the state and federal level. | Dependent on specific program. Some show positive results in targeted areas, while others have limited reach or effectiveness. |
| Early Intervention Programs | Support programs for identifying and addressing mental health issues early in life. | Generally promising, but needs more robust evaluation and widespread implementation. |
| Telemedicine Access | Increased accessibility of mental health services via telehealth platforms. | Showed positive results in terms of reaching geographically isolated populations and increasing convenience for patients. |
Illustrative Case Studies
Depression, a pervasive mental health challenge, profoundly impacts individuals and their families. Understanding its manifestations and the journeys toward recovery is crucial for fostering empathy and effective support systems. These case studies offer glimpses into the diverse experiences of those affected, highlighting the complexity of the condition and the importance of personalized interventions.
Impact of Depression on Individuals and Families
Depression’s effects extend beyond the individual, impacting family dynamics and overall well-being. The following cases illustrate this.
- Sarah, a young professional, experienced a significant downturn in her mood and motivation following a job loss. Her once vibrant social life waned, and she withdrew from family gatherings. The weight of financial stress added to her emotional burden, creating a strain on her relationship with her supportive but increasingly worried parents. This situation highlights how depression can create a ripple effect within families, leading to feelings of isolation and frustration for everyone involved.
- Mark, a middle-aged man, struggled with depression masked by irritability and anger. His outbursts at home led to escalating conflicts with his wife and children. This resulted in a strained family environment, impacting his children’s emotional development and creating a cycle of negativity. The family dynamics became increasingly fractured, underscoring how untreated depression can erode relationships and create a difficult home environment.
- Anya, a teenager, experienced a profound shift in her demeanor and academic performance. Her previously optimistic outlook darkened, and she developed feelings of hopelessness and worthlessness. Her once close relationship with her friends fractured, and her once-enjoyed hobbies became sources of anxiety. This example illustrates how depression can manifest in seemingly isolated individuals, affecting their relationships and future prospects.
Successful Treatment and Recovery from Depression
Recovery from depression is possible, and the journey often involves a combination of professional support and personal resilience.
- David, a software engineer, sought professional help after experiencing persistent sadness and lack of motivation. Through therapy and medication, he learned coping mechanisms and strategies to manage his symptoms. He regained his passion for his work and reconnected with friends, marking a significant turning point in his life. This demonstrates how early intervention and ongoing support can facilitate a successful recovery journey.
- Emily, a stay-at-home mother, underwent a multifaceted treatment plan combining therapy, lifestyle changes, and support groups. She developed coping strategies for managing stress and learned to prioritize her own well-being. This enabled her to reconnect with her children and re-engage in her personal interests, ultimately fostering a healthier family dynamic.
- A case study of a young adult who successfully navigated the challenges of depression through a holistic approach encompassing therapy, medication, and support from family and friends, ultimately regaining a sense of purpose and optimism in life. This illustrates the vital role of a support network in the healing process.
Challenges Faced by Individuals Seeking Treatment
Barriers to seeking and accessing treatment for depression can vary widely depending on individual circumstances and societal factors.
- Financial constraints can be a significant obstacle to accessing mental health services. The cost of therapy and medication can be prohibitive for many individuals, particularly those with limited financial resources.
- Stigma surrounding mental illness often prevents individuals from seeking help. Fear of judgment or discrimination can create significant barriers, leading to delayed or avoided treatment.
- Geographic limitations can restrict access to mental health professionals, particularly in rural areas. The distance to treatment centers can pose a significant barrier, leading to delayed or incomplete treatment.
Impact of Social Support on a Person with Depression
Strong social support networks play a vital role in the recovery process for individuals experiencing depression.
- A case study of a person with depression who found significant comfort and encouragement from a close-knit group of friends and family members. Their unwavering support and understanding played a pivotal role in motivating the individual to seek professional help and adhere to the treatment plan.
Summary of Common Themes in Case Studies, Depression the growing american mental health storm
| Theme | Description |
|---|---|
| Impact on Relationships | Depression can strain relationships with family, friends, and partners. |
| Importance of Treatment | Early intervention and ongoing support are crucial for recovery. |
| Barriers to Treatment | Financial constraints, stigma, and geographic limitations can hinder access to care. |
| Role of Social Support | Strong social support networks significantly contribute to recovery. |
Potential Solutions and Interventions
The growing mental health crisis in America demands multifaceted solutions, encompassing individual support, community resilience, and systemic changes. Addressing this crisis requires a proactive approach, moving beyond reactive measures to foster environments that promote mental well-being. Effective interventions must be tailored to the unique needs of individuals and communities, recognizing the diverse factors contributing to mental health disparities.A crucial step in tackling this issue is understanding that mental health is not separate from physical health or social well-being.
Solutions must be comprehensive, addressing not only the immediate symptoms but also the underlying causes and risk factors. Early intervention, prevention, and accessible treatment are paramount in mitigating the long-term impact of mental health challenges.
Early Detection and Intervention Strategies
Early identification of individuals at risk is critical to prevent mental health conditions from escalating. Effective screening tools and protocols can aid in identifying individuals exhibiting early warning signs. These tools can be integrated into primary care settings, schools, and community centers, making early intervention more accessible. Training healthcare providers, educators, and community leaders in recognizing and responding to early warning signs is essential.
By fostering a culture of openness and understanding, individuals can feel comfortable seeking help without fear of judgment. This proactive approach will help create a supportive environment that encourages help-seeking behavior.
Promoting Mental Wellness and Resilience in Communities
Building mental wellness and resilience within communities is a crucial aspect of long-term solutions. This involves implementing programs that foster emotional regulation skills, stress management techniques, and social support networks. Community-based programs that promote positive coping mechanisms, such as mindfulness practices, stress reduction workshops, and support groups, can create a stronger foundation for individuals. These programs can be tailored to specific demographics, ensuring that they meet the unique needs of different communities.
For example, culturally sensitive programs can help bridge cultural gaps and ensure equitable access to support.
Comparing Preventative Measures and Interventions
| Preventative Measure/Intervention | Description | Target Population | Potential Impact | Challenges |
|---|---|---|---|---|
| School-based mental health programs | Integrating mental health services into schools to provide counseling, support groups, and stress-management techniques. | Children and adolescents | Early detection and intervention, improved academic performance, reduced behavioral problems. | Funding limitations, lack of trained professionals, parental resistance. |
| Community-based support groups | Creating support networks for individuals with mental health conditions and their families. | Individuals with mental health conditions and their families | Increased social support, reduced isolation, improved coping skills. | Accessibility issues, stigma, lack of culturally appropriate resources. |
| Mental health awareness campaigns | Raising public awareness about mental health conditions and promoting help-seeking behavior. | General public | Reduced stigma, increased understanding, improved help-seeking rates. | Reaching diverse communities, combating misinformation, sustaining long-term impact. |
| Universal mental health screening | Implementing routine mental health screenings in healthcare settings. | General population | Early detection of mental health issues, prompt intervention, improved access to care. | Privacy concerns, time constraints, need for skilled personnel. |
“Investing in mental health is an investment in the future. By supporting early intervention, community resilience, and accessible treatment, we can create a healthier and more equitable society.”
Conclusive Thoughts: Depression The Growing American Mental Health Storm
In conclusion, depression: The growing American mental health storm demands immediate attention and comprehensive solutions. Addressing the root causes, improving access to treatment, and fostering a culture of mental wellness are crucial steps towards mitigating this crisis. The future of mental health in America hinges on our collective ability to recognize the problem, support those affected, and advocate for systemic change.
Ultimately, understanding the complexities of depression and its devastating impact on individuals and society is paramount in combating this critical issue.