Services lacking for mental health are a critical issue impacting individuals across various demographics. Geographical barriers, financial constraints, and a lack of specialized care create significant hurdles to accessing vital mental health services. This blog post explores the multifaceted challenges surrounding mental health care, examining issues like accessibility, affordability, and the quality of existing services.
From the uneven distribution of mental health professionals across different regions to the exorbitant costs of therapy and medication, the systemic deficiencies in our mental health infrastructure are strikingly apparent. This deep dive delves into the specific gaps in care, highlighting the need for culturally competent professionals, specialized services for diverse populations, and innovative solutions to address long waiting lists and delays.
Accessibility and Affordability of Mental Health Services
Mental health is just as crucial as physical health, yet disparities in access and affordability persist across the globe. These barriers significantly impact individuals’ well-being and hinder the effective treatment of mental illnesses. This exploration delves into the multifaceted challenges surrounding mental health service provision, examining geographical limitations, financial constraints, and the crucial role of insurance.Geographical variations in mental health service provision often reflect broader societal inequalities.
Rural communities frequently experience a shortage of qualified therapists and counselors, while urban areas might face overcrowding and long wait times. This disparity in resources creates a significant hurdle for those in underserved locations, potentially delaying or preventing necessary treatment.
Geographical Disparities in Mental Health Service Provision
Mental health services are often concentrated in urban areas, leaving rural and underserved populations with limited access to care. This lack of access can be attributed to factors like the distance to facilities, limited transportation options, and a shortage of qualified professionals in rural areas. For instance, individuals living in remote Alaskan villages may face significant travel times and costs to reach mental health providers, impacting their ability to receive timely support.
Financial Barriers to Accessing Mental Health Services
Financial constraints represent a substantial barrier to accessing mental health services for various demographics. The cost of therapy, medication, and crisis intervention can be prohibitive for individuals with limited incomes or those without insurance coverage. Low-income individuals and families often struggle to afford even basic mental health services, perpetuating a cycle of unmet needs.
Comparison of Mental Health Service Costs
| Service | Approximate Cost (per session/treatment) | Notes |
|---|---|---|
| Therapy (Individual/Couples) | $50-$200+ | Dependent on therapist’s experience and location |
| Medication Management | $25-$50+ (prescription fee) | Includes doctor’s visit and medication costs |
| Crisis Intervention (emergency room visit) | Variable, potentially high | Costs can vary depending on the severity of the crisis and location. |
| Psychiatric Hospitalization | Very high | Includes medical care, medication, and accommodation costs. |
The table above provides a general overview of potential costs. Actual costs can fluctuate based on various factors such as location, insurance coverage, and the specific type of service needed.
Impact of Insurance Coverage on Access to Mental Health Services
Insurance coverage plays a critical role in determining access to mental health services. Individuals with comprehensive insurance plans often have better access to therapists, medications, and other forms of care. Conversely, those without insurance or with limited coverage may face significant financial hurdles, potentially delaying or preventing treatment altogether. Many insurance plans have limitations on the number of sessions or types of providers covered, further restricting access for those in need.
Strategies for Increasing Affordability and Accessibility
Addressing the affordability and accessibility issues in mental health requires a multi-pronged approach. Increased government funding for mental health services, subsidies for low-income individuals, and partnerships between healthcare providers and community organizations can create more equitable access to care. Expanding telehealth options can make mental health services more accessible to those in rural areas or those facing transportation challenges.
Community-Based Mental Health Initiatives
Community-based mental health initiatives can offer valuable support and resources. These programs may include peer support groups, community outreach programs, and mobile mental health clinics that bring services directly to underserved populations.
- Peer Support Groups: These groups provide a safe space for individuals to share experiences, receive emotional support, and develop coping mechanisms. They are crucial in fostering a sense of community and belonging for those struggling with mental health issues.
- Community Outreach Programs: These programs aim to increase awareness of mental health issues and resources in a specific community. They typically involve educating the public, promoting early intervention, and reducing stigma.
- Mobile Mental Health Clinics: Mobile clinics bring mental health services directly to underserved areas, overcoming geographical barriers and providing timely support to those in need. They provide critical support to remote or underserved communities that often lack access to traditional healthcare facilities.
Availability of Specialized Services

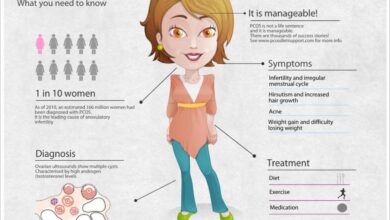
Mental health services are crucial for well-being, but access to specialized care isn’t uniform across all populations. This lack of availability can significantly impact individuals’ ability to receive timely and appropriate treatment, potentially leading to worsened mental health outcomes. This section delves into the specific types of mental health services that are often lacking, highlighting the need for culturally competent professionals and examining disparities in service provision across different demographics.The need for specialized mental health services extends beyond general support.
Individuals facing complex challenges, such as co-occurring disorders or unique cultural needs, often require tailored interventions that address the multifaceted nature of their difficulties. Addressing these gaps is essential to ensure equitable access to care and foster better mental health outcomes for all.
Types of Lacking Mental Health Services
Many individuals struggle to find appropriate and accessible mental health services. A critical gap involves specialized programs tailored to specific populations and needs. This includes children, adolescents, seniors, and individuals from diverse cultural backgrounds. Moreover, services for individuals with co-occurring disorders are often insufficient, leaving these individuals with unmet needs.
- Children and Adolescents: Specialized services for this age group are vital for early intervention and prevention of mental health issues. Programs focused on play therapy, family therapy, and school-based counseling are often limited, leading to delays in diagnosis and treatment. Early intervention can significantly improve outcomes and prevent long-term difficulties. For example, early detection and treatment of anxiety or depression in children and adolescents can prevent the development of more severe mental health issues in adulthood.
- Seniors: Mental health services for seniors often lack adequate resources and support. Geriatric-specific mental health professionals are less common, and programs focused on age-related mental health concerns, such as dementia and grief, are insufficient. This can result in seniors experiencing mental health issues without receiving appropriate care.
- LGBTQ+ Individuals: Mental health services that are sensitive to the unique experiences and challenges faced by LGBTQ+ individuals are often unavailable or inadequate. A lack of culturally competent therapists who understand the specific stressors and discrimination faced by this population can lead to delayed or ineffective treatment.
- Individuals with Co-occurring Disorders: Many individuals experience mental health issues alongside substance use disorders or other physical health conditions. Specialized programs for co-occurring disorders are essential for addressing the interwoven nature of these issues. Without integrated care, these individuals may receive fragmented treatment that fails to address the complex interplay of their conditions.
Culturally Competent Mental Health Professionals
Cultural competence is paramount in mental health services. Therapists who understand and respect the diverse cultural backgrounds of their clients are crucial for effective treatment. A lack of culturally competent professionals can lead to misdiagnosis, ineffective treatment, and a lack of trust between the therapist and client.
- Importance of Cultural Sensitivity: Cultural sensitivity involves understanding the unique values, beliefs, and experiences of diverse communities. It’s essential for establishing rapport and trust with clients from various backgrounds. This approach ensures the treatment plan is tailored to the client’s specific needs and cultural context.
- Examples of Cultural Competence: A culturally competent therapist may incorporate culturally relevant coping mechanisms or utilize culturally sensitive language in therapy sessions. They may also seek to understand the client’s social and family support systems, recognizing their potential influence on the client’s mental health.
Availability of Services for Specific Populations
The availability of mental health services varies significantly for different populations. This disparity often stems from factors such as geographic location, socioeconomic status, and access to healthcare.
| Population | Challenges | Examples of Gaps |
|---|---|---|
| Children | Limited access to specialized programs, delayed diagnosis | Lack of play therapy, school-based counseling |
| Adolescents | Stigma, difficulty accessing care independently | Limited youth-focused mental health services |
| Seniors | Lack of geriatric-specific professionals, social isolation | Inadequate support for age-related conditions |
| LGBTQ+ Individuals | Lack of culturally competent therapists, discrimination | Limited resources for specific LGBTQ+ needs |
| Individuals with Co-occurring Disorders | Fragmented care, difficulty accessing integrated treatment | Lack of coordinated care for substance use and mental health issues |
Specialized Services Not Readily Available
Several specialized mental health services are not readily available, leading to unmet needs.
- Trauma-focused therapy: Trauma-informed care is increasingly recognized as essential for individuals who have experienced trauma. However, access to trauma-focused therapists and specialized programs remains limited.
- Dialectical Behavior Therapy (DBT): DBT is an evidence-based therapy for individuals with borderline personality disorder and other conditions. The availability of DBT-trained therapists is often insufficient.
Mental Health Specialists and Their Roles
A variety of mental health specialists contribute to the provision of care.
| Specialist | Role |
|---|---|
| Psychiatrist | Diagnoses and treats mental illness, prescribes medication |
| Psychologist | Provides therapy, conducts assessments, and researches mental health |
| Social Worker | Provides counseling, support, and advocacy for clients |
| Licensed Counselor | Provides counseling and therapy for a variety of mental health concerns |
| Psychiatric Nurse Practitioner | Provides comprehensive mental health care, including medication management |
Quality and Effectiveness of Existing Services
Navigating the mental health landscape can be challenging, especially when considering the quality and effectiveness of available services. Many individuals experience frustration with aspects of current models, while maintaining high-quality care across a diverse population presents unique obstacles. Understanding the strengths and weaknesses of existing interventions is crucial for developing more effective and accessible support systems.The effectiveness of mental health services is not simply about providing access; it’s also about delivering care that resonates with the specific needs of each individual.
It’s frustrating how many services are lacking when it comes to mental health support. Finding the right resources can feel like searching for a needle in a haystack, especially during challenging times like menopause. Fortunately, there are simple ways to ease symptoms, like incorporating more walking into your routine. Check out this helpful guide on ways to ease menopause symptoms with walking for some practical tips.
Ultimately, accessible mental health resources are still a major need in our society.
This necessitates a deep understanding of the diverse range of mental health conditions and the varying approaches that may be most beneficial.
Common Complaints About Mental Health Services
A significant number of individuals express dissatisfaction with the quality of mental health services. Common complaints include lengthy wait times for appointments, a lack of culturally sensitive care, and a perceived lack of empathy from providers. Communication breakdowns, inadequate follow-up care, and the feeling of being rushed during sessions are also frequently cited issues. These factors contribute to a sense of disconnection and reduced effectiveness in treatment.
Challenges of Maintaining Quality in a Diverse Population
Serving a diverse population necessitates a nuanced approach to care. Mental health conditions and their presentation can vary across cultures and backgrounds. Providers need to be sensitive to these differences to ensure that their interventions are both culturally appropriate and effective. Linguistic barriers, differing communication styles, and varying levels of familiarity with mental health services can further complicate the provision of high-quality care.
Evaluating the Effectiveness of Mental Health Interventions
Evaluating the effectiveness of mental health interventions requires a multifaceted approach. Measuring outcomes through standardized assessments, patient self-reports, and clinician observations can offer valuable insights. Monitoring symptom reduction, improvement in functioning, and changes in overall well-being are key components in this process. Tracking these metrics over time can help determine the efficacy of specific treatments and tailor interventions for optimal results.
Potential Biases and Limitations in Current Models
Current mental health service models are not without limitations. Implicit biases within the system, whether conscious or unconscious, can influence the types of interventions offered and the quality of care received. These biases can stem from factors such as the clinician’s background, societal norms, or even the patient’s perceived socioeconomic status. The availability of resources, varying access to specialists, and the complexity of certain conditions are also crucial factors to consider.
Effective Strategies for Improving Quality
Several strategies can enhance the quality of mental health services. These include increased funding for mental health programs, improved training for healthcare professionals, and implementing patient-centered care models. Collaboration between mental health providers, community organizations, and policymakers is also essential. Promoting awareness campaigns and reducing stigma surrounding mental illness can also contribute to a more supportive and understanding environment.
Investing in research to develop new and innovative treatment approaches is also paramount.
Table: Contrasting Approaches to Mental Health Treatment
| Treatment Approach | Description | Potential Strengths | Potential Limitations |
|---|---|---|---|
| Cognitive Behavioral Therapy (CBT) | Focuses on identifying and changing negative thought patterns and behaviors. | Evidence-based, effective for various conditions, often time-limited. | May not be suitable for all individuals, requires active participation. |
| Psychodynamic Therapy | Explores unconscious motivations and patterns of behavior. | Can provide deeper understanding of underlying issues, long-term approach. | Requires significant investment of time, may not be suitable for all individuals. |
| Medication Management | Involves the use of prescribed medications to address specific symptoms. | Can provide rapid symptom relief for certain conditions, can be effective in combination with therapy. | Potential side effects, requires careful monitoring, may not address underlying issues. |
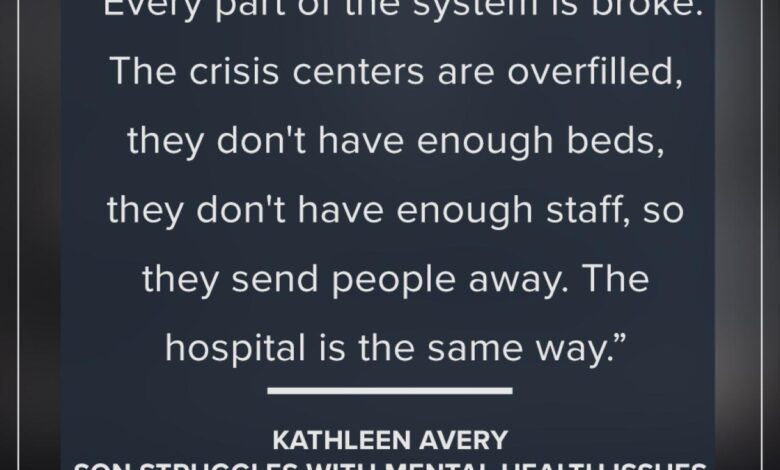
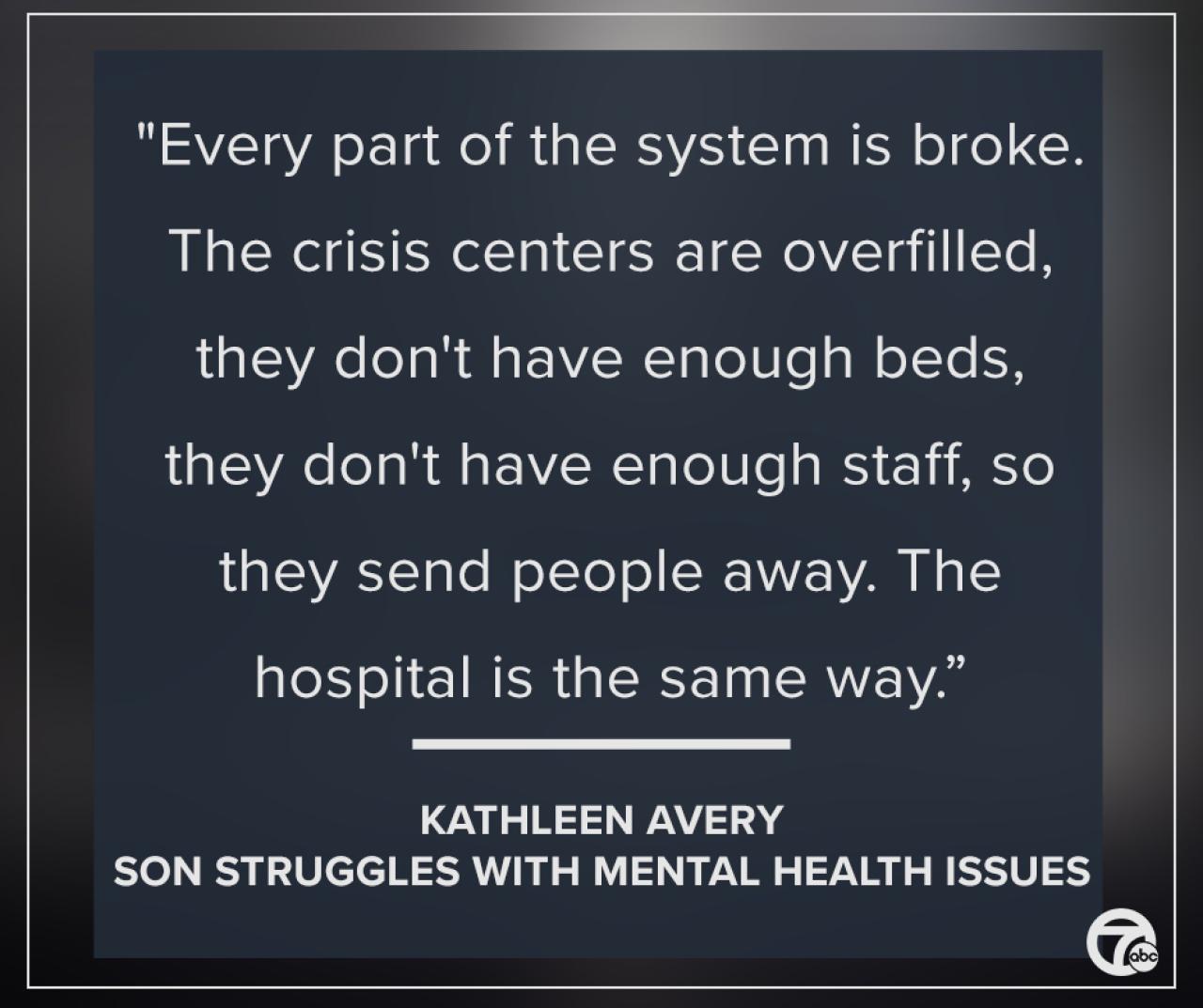
Waiting Lists and Delays in Service
Access to mental health services is crucial for well-being, but lengthy waiting lists and delays can significantly hinder effective treatment and recovery. Prolonged periods of waiting can exacerbate existing mental health conditions, potentially leading to increased symptoms, crisis situations, and decreased quality of life. Understanding the factors contributing to these delays and exploring potential solutions are essential for improving access to timely and effective care.
Impact of Long Waiting Lists on Mental Health Outcomes
Long waiting lists for mental health services can have detrimental effects on individuals’ mental and emotional well-being. Delayed access can lead to worsening symptoms, increased stress, and a decline in overall functioning. Studies have shown a correlation between longer wait times and poorer treatment outcomes, including slower recovery rates and a higher likelihood of relapse. Individuals experiencing acute mental health crises may face a heightened risk of harm when access to timely intervention is delayed.
Reasons for Delays in Accessing Mental Health Services
Several factors contribute to delays in accessing mental health services. Limited availability of mental health professionals, particularly specialists, is a significant constraint. Insufficient funding for mental health services can result in limited staffing and resources, thereby impacting service capacity. Furthermore, bureaucratic processes and administrative hurdles can create delays in scheduling appointments and initiating treatment plans. Demand for services often outstrips the available capacity, creating longer wait times.
It’s frustrating how many gaps exist in mental health services, especially for marginalized communities. We need to shine a light on inclusive wellness, like exploring the options at shining a light on inclusive wellness , to address these inequities and create more accessible pathways to care. Ultimately, the lack of comprehensive mental health support continues to be a major concern for so many.
Strategies for Reducing Waiting Times for Mental Health Services
Reducing waiting times for mental health services requires a multifaceted approach. Investing in increased funding for mental health services is paramount to expanding service capacity and hiring additional mental health professionals. Improving service delivery models, such as telehealth and online therapy options, can enhance accessibility and reach more individuals. Streamlining administrative processes and reducing bureaucratic hurdles can also significantly expedite the process of accessing care.
Collaborating with community organizations and outreach programs can help identify and connect individuals in need with available services.
Innovative Solutions to Address Delays in Care
Innovative approaches to address delays in mental health care include the implementation of mobile crisis teams and early intervention programs. These initiatives aim to provide immediate support and prevent escalation of crises, potentially reducing the need for lengthy hospitalizations. Another innovative solution is the utilization of peer support groups, which can provide valuable assistance and reduce wait times for individual therapy.
Developing more accessible and flexible appointment scheduling options, such as evening and weekend appointments, can improve convenience and increase access to services.
Consequences of Prolonged Waiting Periods for Mental Health Patients
Prolonged waiting periods for mental health services can have profound negative consequences for patients. Individuals experiencing severe mental health conditions may face a heightened risk of worsening symptoms, leading to increased distress, crisis situations, and potential harm. The delay in receiving appropriate care can also result in a decreased likelihood of successful treatment outcomes and recovery. Furthermore, prolonged waiting can contribute to a sense of hopelessness and despair, potentially leading to social isolation and decreased quality of life.
Average Waiting Times for Mental Health Services (Illustrative Data)
| Region | Therapy (General) | Psychiatric Evaluation | Crisis Intervention |
|---|---|---|---|
| North America (Selected Cities) | 6-8 weeks | 4-6 weeks | 1-2 days |
| Western Europe (Selected Countries) | 4-6 weeks | 2-4 weeks | 1-3 days |
| Developing Countries (Selected Regions) | 8-12+ weeks | 6-12+ weeks | 3-7 days |
Note: This table presents illustrative data and may not reflect all regions or specific services. Actual wait times can vary significantly based on local resources, demand, and service type.
Stigma and Discrimination Surrounding Mental Illness
The pervasive stigma surrounding mental illness acts as a significant barrier to individuals seeking help and support. This societal prejudice creates a climate of fear and shame, often discouraging those struggling with mental health conditions from reaching out for treatment. The fear of judgment, social isolation, and discrimination can lead to delayed or avoided treatment, ultimately hindering recovery and impacting overall well-being.
Negative Impact on Seeking Services
The stigma associated with mental illness often discourages individuals from seeking professional help. Fear of being labeled, judged, or ostracized by family, friends, or colleagues can be overwhelming. This fear can lead to self-stigma, where individuals internalize negative societal perceptions and doubt their worth. As a result, individuals may delay or avoid necessary treatment, potentially exacerbating their condition and hindering their ability to lead fulfilling lives.
It’s frustrating how many gaps there are in mental health services, especially for those facing complex challenges. While researching resources for supporting loved ones, I stumbled across a really helpful blog focusing on the best health blog early onset alzheimers best health blog early onset alzheimers. It highlighted the importance of early intervention and comprehensive care, which got me thinking about the lack of similar support systems for other mental health conditions.
The need for more accessible and specialized services remains critical.
Manifestations of Stigma in Social Contexts
Stigma manifests in various social contexts, affecting individuals in different ways. In the workplace, it can lead to discrimination, prejudice, and unfair treatment, potentially resulting in job loss or career stagnation. Within families, stigma can cause conflict and strained relationships, impacting the emotional well-being of both the individual and their loved ones. In communities, it can result in isolation and exclusion, impacting social participation and creating a sense of alienation.
Strategies for Reducing Stigma and Promoting Awareness
Combating the stigma surrounding mental illness requires a multifaceted approach. Open and honest conversations about mental health can help normalize these conditions and reduce the fear associated with them. Education and awareness campaigns can play a crucial role in challenging negative stereotypes and misconceptions. Public figures and celebrities sharing their personal experiences can help create empathy and understanding.
Promoting mental health literacy and encouraging early intervention are essential to breaking the cycle of stigma and empowering individuals to seek help.
Methods for Promoting Acceptance and Understanding
Promoting acceptance and understanding of mental health conditions requires a proactive approach. Community-based support groups can offer a safe space for individuals to connect with others who share similar experiences, fostering a sense of belonging and reducing isolation. Mentorship programs can connect individuals with positive role models who have successfully navigated their mental health challenges. Creating inclusive workplaces and communities can help ensure that individuals with mental health conditions feel safe and supported.
Impact Across Cultural Backgrounds
The impact of stigma on access to mental health services varies across different cultural backgrounds. Cultural norms, beliefs, and values can influence how individuals perceive and respond to mental health conditions. In some cultures, there may be a greater reluctance to seek professional help due to societal expectations or religious beliefs. Addressing cultural nuances and sensitivities is critical to developing culturally appropriate mental health interventions and services that effectively reach and support individuals from diverse backgrounds.
Common Misconceptions about Mental Illness
| Misconception | Reality |
|---|---|
| Mental illness is a sign of weakness or a character flaw. | Mental illness is a medical condition, like any other physical illness, that can affect anyone regardless of their personality or strength. |
| People with mental illness are unpredictable and dangerous. | The vast majority of people with mental illness are not violent or unpredictable. Mental illness is a complex condition, and violence is not inherent to it. |
| Mental illness can be cured by willpower or prayer alone. | Mental illness requires professional treatment, much like physical illnesses. A combination of therapy, medication, and lifestyle changes may be necessary for effective management. |
| Mental illness is a temporary condition. | Mental illnesses can be chronic conditions that require ongoing management and support. |
Gaps in Mental Health Support Systems
Mental health is crucial for overall well-being, and yet, many individuals struggle to access comprehensive support systems. Existing services often fall short in providing the holistic care needed for recovery and long-term well-being. This creates significant gaps in the support systems available to those with mental health conditions. Addressing these gaps requires a multifaceted approach that goes beyond traditional treatment models.The current mental health support landscape often lacks consistent and readily available resources, particularly in underserved communities.
This deficiency can lead to a cycle of worsening symptoms, delayed interventions, and diminished quality of life for those affected. A more robust and accessible support network is necessary to effectively address the needs of individuals with mental health conditions.
Identifying Gaps in Support Systems
Individuals with mental health conditions frequently experience challenges accessing appropriate and timely support. These challenges often stem from a lack of coordinated care between different service providers, inadequate community-based resources, and insufficient community outreach programs. Further exacerbating these issues are the lingering stigma and discrimination associated with mental illness. These factors contribute to the significant gaps in existing support systems.
Need for Community-Based Support Networks
Community-based support networks are essential for bridging the gap in mental health services. These networks provide a safe and supportive environment where individuals can connect with others facing similar challenges. They also offer a space for mutual learning and shared experiences. The support and encouragement offered within these networks contribute to a sense of belonging and empowerment, crucial for recovery.
Importance of Peer Support Groups in Mental Health Recovery
Peer support groups play a vital role in the recovery process. They offer a unique opportunity for individuals to share their experiences, learn from each other, and build a sense of community. Peer support can provide valuable insights and coping strategies that professionals might not always address. This supportive environment fosters a sense of hope and resilience, facilitating recovery and improved well-being.
Role of Family and Social Support in Mental Health
Family and social support play a crucial role in the journey of mental health recovery. Strong family and social connections can provide emotional stability, practical assistance, and a sense of belonging. A supportive environment encourages individuals to seek help and participate in treatment, while also promoting overall well-being. This support is vital for both the individual and the family unit.
Creating a Supportive Environment
Creating a supportive environment for individuals with mental health conditions involves several key strategies. It necessitates fostering open communication, empathy, and understanding. It also requires creating a safe space for individuals to express their needs and concerns without judgment. Education and awareness about mental health conditions are also critical components in creating such an environment.
Effective Support Strategies for Individuals with Severe Mental Illness
Effective support strategies for individuals with severe mental illness require a personalized and comprehensive approach. Strategies should focus on building resilience, promoting self-management skills, and facilitating access to resources. This includes providing access to evidence-based treatments, peer support networks, and community-based programs that address the specific needs of the individual.
Examples of Effective Support Strategies
Examples of effective support strategies include:
- Providing resources for self-care: Strategies like stress management techniques, relaxation exercises, and healthy lifestyle choices can improve overall well-being and reduce the impact of symptoms.
- Promoting social connections: Facilitating opportunities for social interaction and engagement can combat feelings of isolation and promote a sense of belonging.
- Offering practical assistance: Assistance with daily tasks, such as transportation, errands, or household chores, can significantly reduce stress and improve the quality of life.
Technology and Mental Health Services: Services Lacking For Mental Health
Technology is rapidly transforming various aspects of healthcare, and mental health is no exception. The potential for technology to improve access, personalize care, and enhance the effectiveness of mental health services is immense. However, alongside this potential, there are limitations and ethical considerations that must be carefully addressed. This exploration delves into the multifaceted role of technology in modern mental healthcare.Technology offers unprecedented opportunities to break down barriers to mental health services.
From remote consultations to personalized support tools, digital platforms can extend access to individuals in underserved areas or those facing logistical challenges. This expanded reach is particularly significant for individuals experiencing social isolation or limited mobility.
Potential for Improved Access
Technology is revolutionizing how mental health services are delivered, creating new pathways to care. Telehealth platforms, mobile apps, and online resources are making mental health support more accessible, especially for those in geographically isolated locations or with limited mobility. These advancements allow for more frequent check-ins and reduce the burden of travel and scheduling constraints, potentially leading to quicker interventions.
Examples of such technology include virtual therapy sessions via video conferencing, self-help apps offering guided exercises and coping strategies, and online support groups providing a sense of community.
Limitations and Ethical Considerations, Services lacking for mental health
While technology holds immense promise, it’s crucial to acknowledge its limitations and ethical considerations. Digital divides remain a significant challenge, as not everyone has equal access to technology or the digital literacy needed to utilize these tools effectively. Furthermore, maintaining the confidentiality and security of sensitive patient data is paramount, requiring robust cybersecurity measures. Concerns regarding the potential for misdiagnosis or inaccurate self-reporting also need careful consideration.
The digital environment must also be mindful of potential biases in algorithms and ensure equitable access for all.
Improving Effectiveness of Care
Technology can play a vital role in enhancing the effectiveness of mental health care. Monitoring tools can track patient progress, allowing for more personalized interventions. This continuous feedback loop enables clinicians to adjust treatment strategies as needed, leading to more effective outcomes. Examples include mobile apps that track mood fluctuations and sleep patterns, allowing for early detection of potential relapses, and digital platforms that facilitate adherence to treatment plans.
Personalizing Mental Health Support
Technology allows for a more personalized approach to mental health support. Tailored interventions, based on individual needs and preferences, are increasingly possible. Algorithms and data analytics can help identify patterns and predict potential issues, enabling proactive interventions. For instance, apps offering personalized exercises, cognitive behavioral therapy (CBT) techniques, and relaxation exercises based on individual strengths and weaknesses can lead to more tailored and effective treatment.
Role of Telehealth in Expanding Access
Telehealth is proving to be a crucial tool in expanding access to mental health services. Virtual consultations, therapy sessions, and support groups are making mental health care more accessible to a wider range of individuals. Telehealth can bridge geographical gaps and reduce the barriers of time and transportation, making care more convenient and accessible. It is particularly important in reaching rural communities and individuals who may face challenges in accessing traditional healthcare settings.
Comparison of Telehealth Platforms
| Platform | Features | Pros | Cons |
|---|---|---|---|
| Platform A | Video conferencing, secure messaging, progress tracking | Easy to use, wide range of features | Potential for technical issues, privacy concerns |
| Platform B | Mobile app with CBT exercises, mood tracking | Convenient, personalized approach | Limited scope, potential for data overload |
| Platform C | Online support groups, peer-to-peer interaction | Community-focused, cost-effective | Moderation challenges, limited professional oversight |
Note: This table provides a general comparison. Specific features and limitations may vary among different telehealth platforms.
Final Conclusion
In conclusion, the lack of adequate mental health services creates a vicious cycle of unmet needs, perpetuating stigma and hindering recovery. Addressing these gaps requires a multi-pronged approach that considers accessibility, affordability, and quality of care. This includes fostering community-based support systems, reducing stigma, and utilizing technology to improve access. Only by tackling these issues head-on can we begin to build a more supportive and equitable mental health system for all.