Interest in vasectomies increases after abortion ruling what to know about the procedure. This surge in interest raises important questions about the procedure, its implications, and the factors influencing this decision. We’ll explore the reasons behind this connection, delve into the procedure itself, and examine the considerations involved in choosing permanent contraception. From the surgical details to the long-term effects, this comprehensive guide aims to equip readers with the knowledge to make informed decisions.
The recent abortion ruling has undeniably sparked a significant conversation surrounding reproductive choices. This has led to a renewed focus on vasectomy as a viable and permanent birth control option for men. While vasectomies have always been an option, the recent surge in interest highlights the complex interplay of societal, personal, and medical factors driving this trend. This article will address the concerns and misconceptions surrounding this procedure, ensuring a clear understanding for those considering it.
Introduction to Vasectomies
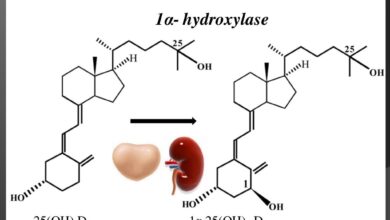
A vasectomy is a surgical procedure for permanent male contraception. It involves severing or blocking the vas deferens, the tubes that carry sperm from the testicles to the ejaculatory ducts. This effectively prevents sperm from mixing with semen during ejaculation, rendering a man infertile. The procedure is generally considered safe and highly effective, but it’s crucial to understand the implications before undergoing it.Vasectomies are a significant choice, altering a man’s reproductive capacity permanently.
Understanding the process, potential side effects, and common misconceptions surrounding the procedure is essential for making an informed decision. Recovery times and potential complications should also be considered.
Understanding the Vasectomy Procedure
A vasectomy is a relatively straightforward surgical procedure. A surgeon makes small incisions in the scrotum and then cuts, ties, or cauterizes the vas deferens. This prevents sperm from traveling to the ejaculate. Local anesthesia is typically used, minimizing discomfort during the procedure. Post-operative care is crucial to ensure proper healing and avoid complications.
Vasectomy Recovery Process
The recovery from a vasectomy is generally quick and straightforward. Most men experience minimal discomfort, often managed with over-the-counter pain relievers. Light activity can resume within a few days, and heavier activities may take a week or two. Full recovery typically takes about a couple of weeks. Pain and swelling are common, and ice packs can help manage these symptoms.
Proper wound care and adherence to post-operative instructions are essential for a smooth recovery.
Potential Side Effects of a Vasectomy, Interest in vasectomies increases after abortion ruling what to know about the procedure
While vasectomies are generally safe, potential side effects can occur. These include pain, swelling, bruising, and infection at the incision site. In rare cases, bleeding or hematomas can develop. Some men experience persistent discomfort or pain in the scrotum, which can be managed with medication or further medical attention. The risk of these complications is relatively low, but individuals should be aware of the possibilities.
Common Misconceptions about Vasectomy
Some common misconceptions about vasectomies include concerns about reduced libido or sexual performance. However, vasectomies do not affect hormone production or sexual function. It’s also important to note that vasectomy does not protect against sexually transmitted infections (STIs). A vasectomy only addresses fertility; protection from STIs requires proper condom use. Another common misconception is that the procedure is irreversible.
While vasectomy is considered permanent, some reversal procedures exist, but they are not always successful.
Vasectomy vs. Other Permanent Contraception Methods
| Feature | Vasectomy | Tubal Ligation (Female) |
|---|---|---|
| Procedure | Surgical severing or blocking of vas deferens | Surgical severing or blocking of fallopian tubes |
| Recovery Time | Generally short, a few days to a couple of weeks | Similar to vasectomy, usually a few days to a couple of weeks |
| Potential Side Effects | Pain, swelling, infection | Pain, swelling, infection |
| Cost | Variable depending on location and insurance | Variable depending on location and insurance |
| Effectiveness | Extremely effective, but not immediate | Extremely effective, but not immediate |
This table provides a concise comparison of vasectomy and tubal ligation, highlighting key aspects of each procedure. Careful consideration of individual circumstances, recovery expectations, and cost factors is essential when choosing a permanent contraception method.
So, vasectomy interest is up after the recent abortion ruling. It’s a big decision, and understanding the procedure is key. This rise in interest highlights the importance of informed choices, but it’s also important to remember that proactive healthcare goes beyond just reproductive options. For example, consider the significant dangers of delaying or skipping vaccinations for children, as discussed in more detail here: the danger in delaying or skipping vaccinations for children.
Ultimately, making thoughtful decisions about your health and the health of your family is crucial, whether it’s a vasectomy or routine check-ups.
Increased Interest Following Abortion Ruling
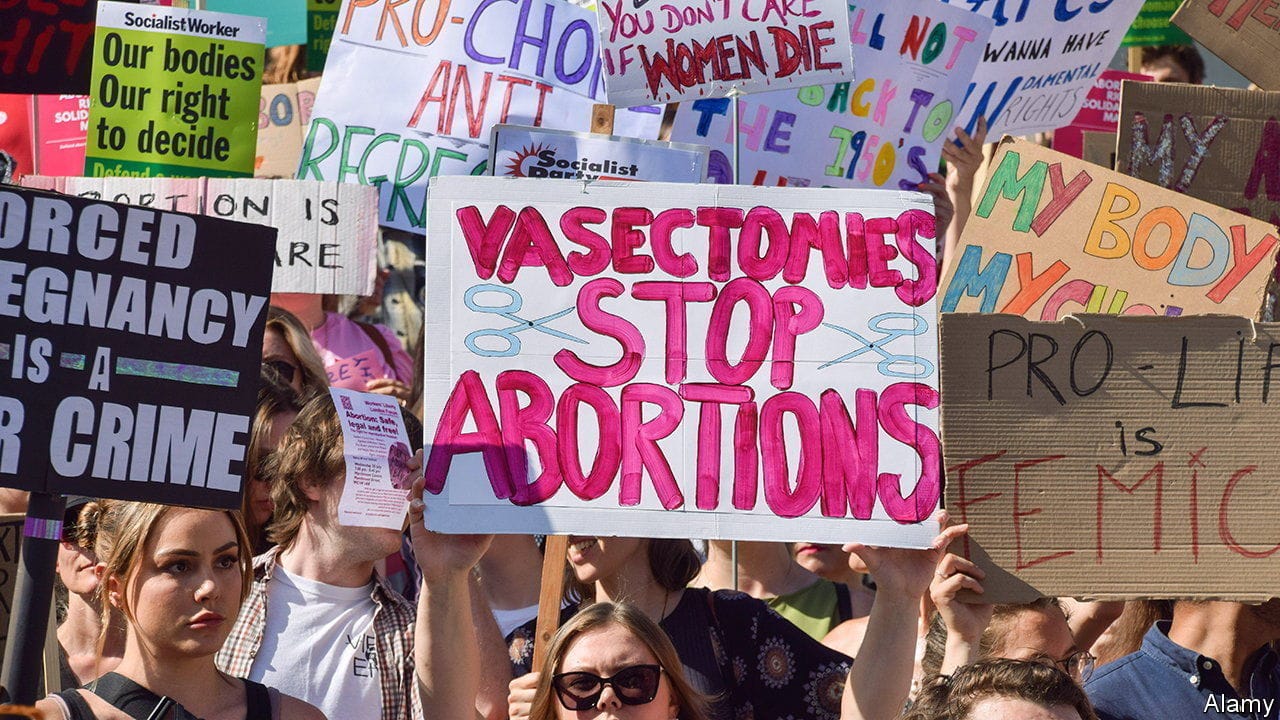
The recent legal changes regarding abortion access have sparked a noticeable ripple effect, including a surge in interest surrounding vasectomies. This isn’t a simple coincidence; a complex interplay of societal shifts and personal choices is driving this trend. Understanding the motivations and potential anxieties associated with this increase is crucial for a nuanced perspective.The correlation between the abortion ruling and the rising interest in vasectomies isn’t straightforward.
It’s more accurate to say that the ruling has highlighted the complex choices facing individuals regarding family planning. Many couples are reassessing their reproductive strategies, and vasectomies, as a permanent form of male contraception, are becoming a more prominent option for some.
Factors Contributing to Increased Interest
The recent legal changes regarding abortion have led many to re-evaluate their reproductive choices. This reevaluation includes a deeper consideration of long-term family planning strategies, with vasectomies potentially emerging as a more permanent contraceptive option for some. Personal values and beliefs play a significant role in this decision-making process, influencing the perceived risks and benefits of each reproductive method.
Societal pressures and conversations surrounding the topic can also contribute to the heightened interest in vasectomies.
Potential Concerns and Anxieties
The increased interest in vasectomies is not without potential concerns. For some, the permanence of the procedure can be a significant factor. Concerns about future changes in desires or circumstances are valid considerations. Furthermore, access to accurate information and support from healthcare providers is crucial to ensure informed decisions. Discussions surrounding the procedure’s potential impact on relationships, financial considerations, and the individual’s personal values need to be addressed.
Comparison to Historical Trends
While precise data on historical trends in vasectomy procedures is needed, the current surge in interest can be contrasted with general trends. Historically, vasectomies have been a viable option for contraception, but the recent increase suggests a significant shift in how the procedure is perceived and accessed. A comparison of current interest levels with historical trends will help provide a clearer understanding of the scale and significance of this increase.
Role of Media and Public Discourse
Media coverage and public discourse play a significant role in shaping public perception. Increased visibility and discussion of vasectomies can contribute to a more open and informed conversation around reproductive health. However, it’s essential to ensure that the information presented is accurate and does not contribute to misconceptions or misinterpretations of the procedure. Public discourse can also highlight important considerations, such as the ethical and social implications of reproductive choices.
Procedure Details and Considerations
Understanding the vasectomy procedure is crucial for anyone considering this permanent birth control method. This section delves into the surgical details, potential risks, and post-operative care, equipping you with the knowledge to make an informed decision.The vasectomy procedure is a relatively straightforward surgical process, typically performed under local anesthesia. It involves a small incision to access the vas deferens, the tubes that carry sperm from the testicles.
The vas deferens are then sealed or cut, preventing sperm from mixing with the semen.
Surgical Procedure Steps
The vasectomy procedure is generally performed in a doctor’s office or clinic, with the patient fully conscious and under local anesthesia. The surgeon will make a small incision in the scrotum, identify the vas deferens, and carefully separate it from surrounding tissue. Next, a small segment of the vas deferens is either cut or sealed with a special technique, such as cauterization or ligation, to prevent sperm from traveling through it.
The incision is then closed with sutures, and a dressing is applied.
Potential Risks and Complications
While vasectomies are generally safe, potential risks and complications include bleeding, infection, and hematoma formation at the incision site. Pain and swelling are also common, though usually mild and temporary. Rarely, the vas deferens may reconnect, negating the effectiveness of the procedure. A small percentage of men may experience persistent pain or discomfort. Thorough discussion with a healthcare professional can help assess the potential risks in individual cases.
Post-Operative Care
Proper post-operative care is essential for a smooth recovery. Patients are typically instructed to wear supportive undergarments, such as athletic support or a scrotal support, to reduce swelling and discomfort. Ice packs can also be applied to the affected area for the first 24-48 hours. It’s important to avoid strenuous activity for several days to allow the incision to heal.
Following the doctor’s instructions for pain management and wound care is critical.
Follow-up Appointments and Monitoring
Regular follow-up appointments are essential to ensure the procedure’s success and to monitor for any complications. The doctor will typically examine the incision site, assess the patient’s recovery, and conduct semen analysis to confirm the absence of sperm in the ejaculate. These analyses confirm the effectiveness of the vasectomy. A follow-up appointment may be scheduled 4-6 weeks after the procedure to verify that the vas deferens are completely sealed.
Factors Influencing Decision-Making
Choosing to undergo a vasectomy is a significant personal decision. It’s not just about preventing pregnancy; it’s about considering long-term implications for family planning, personal lifestyle, and overall well-being. This decision should be made thoughtfully, with a thorough understanding of the procedure, its potential effects, and personal circumstances.Understanding the motivations behind a vasectomy helps in appreciating the diverse factors that play a crucial role in a person’s choice.
These range from health concerns to personal values, and ultimately, a comprehensive understanding of these factors will guide individuals toward making an informed decision that aligns with their individual circumstances.
Personal Circumstances and Lifestyle Considerations
Personal circumstances significantly influence a person’s decision. These include the desire for permanent birth control, the current and anticipated family size, and the individual’s overall lifestyle. Couples who have completed their family planning or who choose not to have children might opt for vasectomy as a permanent solution. Conversely, individuals who may change their minds later need to carefully weigh the irreversible nature of the procedure.
Health Considerations and Medical Advice
Health considerations are an integral part of the decision-making process. Pre-existing medical conditions, such as certain blood clotting disorders or conditions affecting the scrotum, can affect the feasibility and potential risks of the procedure. Open communication with a healthcare professional is crucial to assess any potential risks or complications specific to the individual. Discussing family history of similar issues is also important.
Importance of Open Communication and Counseling
Thorough discussions and counseling are essential before undergoing a vasectomy. Open communication between partners, if applicable, helps in shared decision-making and understanding of the procedure’s long-term implications. A discussion about potential regret, the irreversible nature of the procedure, and the alternative options, such as using condoms, can be crucial. These conversations facilitate a clear understanding of the implications for both partners.
The recent abortion ruling has sparked a noticeable rise in interest in vasectomies. Understanding the procedure is key, but it’s also important to remember that, while some people might look for extra vitamins to support their health, researchers are finding that multivitamins don’t necessarily offer significant health advantages (check out multivitamins don’t provide many health benefits researchers say ).
Ultimately, focusing on a balanced diet and lifestyle choices is likely more beneficial than relying on supplements when considering options like vasectomy.
Role of Medical Professionals in Guiding Patients
Medical professionals play a vital role in guiding patients through the decision-making process. They provide information about the procedure, potential risks and benefits, and answer questions in a clear and unbiased manner. Physicians should also help patients evaluate their individual circumstances and personal values, guiding them towards the best choice that aligns with their needs. This includes addressing potential anxieties and concerns.
Potential Advantages and Disadvantages of Vasectomy
| Aspect | Advantages | Disadvantages |
|---|---|---|
| Personal Well-being | Reduced stress and anxiety related to unwanted pregnancies. Increased freedom and flexibility in life choices. | Potential for regret in the future, especially if there’s a significant change in family planning. |
| Financial Implications | Eliminates the cost and hassle of contraception. | Initial cost of the procedure itself. |
| Relationship Impact | Allows for open communication and shared decision-making about family planning. | Potential for disagreements or misunderstandings if the decision isn’t thoroughly discussed. |
| Long-term Effects | Permanent form of birth control, eliminating the need for ongoing contraception. | Irreversible nature of the procedure, potentially leading to regret. |
Accessibility and Affordability
Vasectomy, a safe and effective permanent birth control option, has seen a surge in interest. However, equitable access and affordability remain critical factors in its widespread adoption. Understanding the barriers and potential solutions is crucial for ensuring this procedure is accessible to all who desire it.Many factors contribute to the accessibility and affordability of vasectomies, ranging from geographic location to individual insurance coverage.
This section delves into these key aspects, providing insights into the realities of accessing this procedure.
Geographic Accessibility
Vasectomy availability varies significantly across different regions. Rural areas often have fewer providers offering the procedure, leading to longer travel times and potentially higher costs. Urban centers, on the other hand, might have a greater concentration of qualified surgeons, but even there, appointment scheduling and wait times can be a factor. The availability of qualified professionals and the prevalence of healthcare facilities directly influence the accessibility of the procedure.
Financial Considerations
Vasectomy procedures can have associated costs, including the surgeon’s fees, facility charges, and potential follow-up appointments. Patients must factor these expenses into their overall healthcare budget. The lack of insurance coverage can be a significant financial burden for some individuals, potentially deterring them from pursuing the procedure.
Insurance Coverage
Insurance coverage for vasectomies varies considerably based on the specific plan and the provider. Some plans may cover the procedure in full, while others might only cover a portion or nothing at all. It’s crucial for individuals to review their policy details to understand the extent of their coverage. Furthermore, pre-authorization or referrals might be necessary in certain cases.
Cost Comparison Table
The cost of vasectomy procedures can fluctuate widely depending on location, the surgeon’s experience, and the facility’s fees. The following table provides a simplified comparison, highlighting the potential variation.
| Location | Estimated Cost (USD) | Notes |
|---|---|---|
| Urban Major City (US) | $500 – $1500 | Higher concentration of surgeons and facilities. |
| Rural County (US) | $700 – $2000 | Potential for longer travel distances and fewer providers. |
| Urban City (Europe) | €400 – €1200 | Healthcare systems and pricing models can vary. |
| Rural Area (Developing Country) | $100 – $500 | Dependent on local costs and availability. |
Note: These are estimated ranges and actual costs may differ. It is essential to contact specific providers for precise pricing information.
Low-Cost or Subsidized Options
Some organizations and healthcare facilities might offer low-cost or subsidized vasectomy options. These programs are often targeted at specific demographics or communities facing financial hardship. Researching local healthcare providers and community programs can uncover such opportunities. These programs often aim to make the procedure more accessible to those who may not otherwise be able to afford it.
Long-Term Effects and Reversibility
Choosing a vasectomy is a significant decision, demanding careful consideration of its permanent nature. While the procedure offers a reliable method of male contraception, understanding the long-term implications, including the possibility of reversal, is crucial for informed consent. This section delves into the potential effects of a vasectomy and the intricacies of reversal procedures.Vasectomy is a surgical procedure that permanently blocks the vas deferens, the tubes that carry sperm from the testicles.
This interruption prevents sperm from mixing with semen, effectively rendering the man infertile. The immediate and short-term effects are generally minimal, with most men experiencing only mild discomfort and swelling. However, the long-term effects are primarily related to the absence of sperm in the ejaculate.
Long-Term Health Effects
A vasectomy does not typically cause any significant long-term health problems. It doesn’t impact hormone production, sexual function, or libido. The absence of sperm in the semen does not lead to any discernible health risks. However, it’s essential to recognize that the procedure’s irreversibility is a critical aspect of the decision-making process.
Vasectomy Reversal
Vasectomy reversal, also known as vasovasostomy, is a surgical procedure aimed at reconnecting the vas deferens. This process is intended to restore fertility, allowing sperm to once again travel through the vas deferens to the ejaculate. The success rate of vasectomy reversal varies significantly, with factors like the surgeon’s experience, the duration since the vasectomy, and the extent of damage to the vas deferens playing a role.
The recent abortion ruling has understandably sparked a surge in interest in vasectomies. It’s a significant procedure, and understanding the details is crucial. While this is a personal decision, it’s important to be aware of the potential long-term implications. This surge in interest contrasts with the recent news about young adults with high cholesterol not being given statins, a completely different health consideration.
Young adults with high cholesterol not given statins raises important questions about preventative healthcare. Ultimately, the rise in vasectomy inquiries highlights the need for comprehensive information and support when considering such a significant life decision.
Success Rates and Associated Costs
Success rates for vasectomy reversal typically range from 30-80%. A crucial point to remember is that no guarantee of success can be provided, and individual outcomes may differ. The success rates are contingent on various factors, and a consultation with a qualified urologist is essential to understand the specific prognosis. Reversal procedures can involve extensive surgical techniques and carry a substantial financial burden.
Costs vary depending on the complexity of the procedure and the location of the medical facility. Furthermore, the success of the reversal is not guaranteed, and the cost of the reversal is not typically covered by insurance.
Potential Complications
Vasectomy reversal, like any surgical procedure, carries the risk of complications. These may include bleeding, infection, damage to surrounding tissues, and the formation of scar tissue, which can potentially hinder the success of the reversal procedure. It is crucial to discuss the potential complications with the surgeon and weigh the risks against the potential benefits.
Importance of Understanding Irreversibility
The fundamental aspect of a vasectomy is its irreversibility. This permanent nature significantly alters the reproductive status and future options. Understanding the procedure’s irreversible nature is vital to ensure the decision aligns with the patient’s long-term goals and aspirations. The implications of this irreversibility must be weighed carefully against the desire for contraception. Thorough counseling with a healthcare provider is recommended before making a final decision.
Addressing Concerns and Misconceptions

Vasectomies, while a safe and effective form of male sterilization, are sometimes shrouded in myths and misconceptions. Understanding the facts can help dispel anxieties and encourage informed decision-making. This section aims to address common concerns and misconceptions surrounding the procedure.
Common Misconceptions about Vasectomies
Vasectomies are often associated with myths and inaccurate beliefs. It’s crucial to separate fact from fiction to ensure individuals are making well-informed choices.
- Vasectomies are irreversible.
- Vasectomies lead to significant pain and discomfort.
- Vasectomies negatively impact sexual function or libido.
- Vasectomies are a complex and risky surgical procedure.
Concerns Regarding Pain, Recovery Time, and Sexual Function
Many individuals harbor concerns about the pain, recovery time, and potential impact on sexual function following a vasectomy. Addressing these concerns is vital for a positive experience.
- Pain: While some mild discomfort is expected, significant pain is rare. Most men report only a moderate level of pain manageable with over-the-counter pain relievers. Post-operative pain is typically temporary and subsides within a few days. Modern surgical techniques and local anesthesia contribute to a less painful experience.
- Recovery Time: Recovery from a vasectomy is generally swift. Most men can resume normal activities within a week or two. Light activities can be resumed sooner, while strenuous activities might need a slightly longer recovery period.
- Sexual Function: Vasectomies do not affect sexual desire (libido) or the ability to achieve an erection. Ejaculation will no longer contain sperm, but the sensation and pleasure associated with sexual activity remain unchanged. It’s important to remember that sexual function is a complex interplay of physical and psychological factors, and vasectomy does not impact these fundamental aspects.
Frequently Asked Questions (FAQ)
Addressing common questions directly helps alleviate anxieties and provides clear answers.
| Question | Answer |
|---|---|
| Is a vasectomy a major surgical procedure? | No. It’s a relatively minor surgical procedure, often performed under local anesthesia. |
| How long does the recovery take? | Most men can resume normal activities within a week or two, but it varies. |
| Will my sex life be affected? | No. Sexual desire, erections, and sensation remain unaffected. |
| What are the potential long-term risks of a vasectomy? | While rare, potential complications include infection, bleeding, and chronic pain. |
| Can a vasectomy be reversed? | Yes, but the success rate of vasectomy reversal is not guaranteed and varies between individuals. |
Ethical Considerations
Vasectomy, a common and effective form of male birth control, raises important ethical considerations. The decision to undergo this procedure is deeply personal, but it also impacts broader societal views on family planning, reproductive rights, and the responsibility of parenthood. These considerations extend beyond the individual and touch upon societal norms, potential unintended consequences, and the potential for misuse.The procedure itself is generally considered safe and effective, but the ethical implications of its use as a form of birth control are multifaceted.
Different viewpoints and values influence the perception of its ethical standing, reflecting the diverse moral and philosophical frameworks within society.
Different Viewpoints on Vasectomy
Various perspectives exist regarding the ethical implications of vasectomy, often tied to underlying beliefs about individual autonomy, societal responsibility, and the role of contraception. Some individuals may view vasectomy as a straightforward personal choice, aligning with their values regarding family planning. Others may view it through a broader lens, considering its impact on societal demographics or potential for misuse.
Ethical Dilemmas Surrounding Vasectomy
The ethical dilemmas surrounding vasectomy often stem from its potential impact on individuals and society. For example, the decision to undergo a vasectomy can have implications for a couple’s future family planning. Furthermore, societal views on contraception and family planning may influence the perception of vasectomy as a responsible or irresponsible choice. Some ethical concerns might arise regarding the potential for regret, especially in the case of a future desire to have children, although this is a concern shared with many forms of birth control.
Vasectomy in Different Contexts
The ethical considerations of vasectomy vary depending on the specific context. For instance, in cases of medical necessity, such as conditions where pregnancy poses significant health risks, the ethical considerations may differ from those in cases of voluntary contraception. In certain cultural contexts, religious or traditional views on reproduction may influence the acceptance or rejection of vasectomy. Furthermore, the availability and accessibility of the procedure, as well as the potential impact on broader societal demographics, should be considered.
Potential for Misuse and Abuse
The potential for misuse and abuse, though less common, is a valid ethical concern surrounding any medical procedure. For example, the use of vasectomy as a coercive or discriminatory practice against certain groups or individuals could raise ethical concerns. This underscores the importance of access to information, education, and equitable access to the procedure, as well as the need for responsible implementation.
This is a factor to consider, although not necessarily the most prevalent concern.
Conclusion: Interest In Vasectomies Increases After Abortion Ruling What To Know About The Procedure
In conclusion, the increased interest in vasectomies following the abortion ruling underscores a critical moment in reproductive healthcare discussions. Understanding the procedure, potential risks, and personal considerations is crucial. Ultimately, the decision to undergo a vasectomy is a deeply personal one, requiring careful consideration of individual circumstances, medical advice, and ethical implications. We hope this guide provides valuable insight and empowers informed choices.