HPV linked to cervical cancer have declined since the advent of the HPV vaccine, a remarkable testament to the power of preventative medicine. This remarkable drop in cervical cancer cases isn’t just a statistical trend; it represents a significant shift in public health, saving lives and reducing the burden on healthcare systems. We’ll explore the science behind this success, examining the impact of the HPV vaccine on infection rates, cervical cancer incidence, and the long-term implications for global health.
The development of the HPV vaccine marked a crucial turning point in cancer prevention. This vaccine, by targeting the virus responsible for a significant portion of cervical cancers, offers a powerful tool for protecting individuals and communities. Understanding how this vaccine works and the evidence supporting its effectiveness is crucial to appreciating its far-reaching impact on public health.
Introduction to HPV and Cervical Cancer
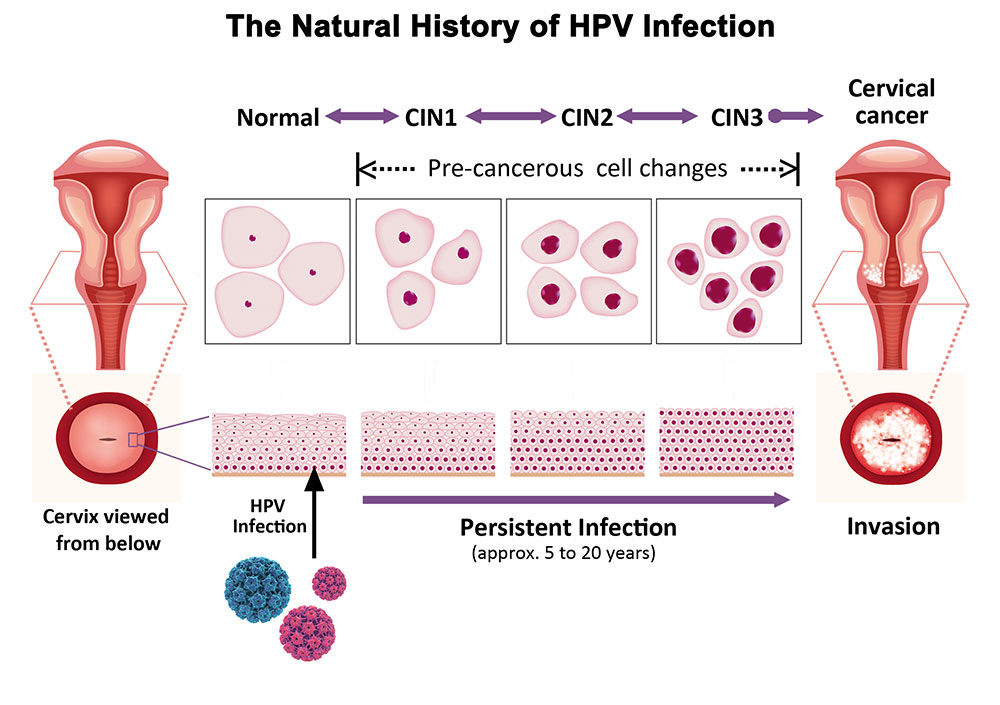
Human papillomavirus (HPV) is a common sexually transmitted infection (STI) affecting both men and women. While many HPV infections resolve without causing any symptoms, some types can persist and lead to various health issues, including cervical cancer. This persistent infection can alter the cellular structure of the cervix, ultimately causing abnormal growth and, if left untreated, potentially developing into cancer.The prevalence of HPV infections is exceptionally high globally, making it a significant public health concern.
A substantial portion of sexually active individuals will contract HPV at some point in their lives. Understanding the different types of HPV and their associated cancer risks is crucial for prevention and early detection.
It’s amazing how the HPV vaccine has significantly lowered the link between HPV and cervical cancer. While prioritizing the health of our loved ones, it’s also crucial to ensure they’re safe in their car seats. Choosing the right convertible car seat is key for little ones, and finding the best one can feel overwhelming. Fortunately, resources like best convertible car seat guides can help.
This translates to safer travels and ultimately, more happy memories. Thankfully, this progress in vaccination efforts continues to make a positive impact on preventing cervical cancer.
HPV Types and Cancer Risk
HPV exists in various strains, categorized by their potential to cause cancer. Certain high-risk HPV types, like HPV 16 and 18, are strongly associated with the development of cervical cancer. Other types may cause genital warts or other less serious conditions.
- High-risk HPV types are linked to the majority of cervical cancers. These types integrate their DNA into the host cell’s genome, causing dysregulation of cellular growth control mechanisms. This disruption of cellular processes can ultimately lead to the development of cancerous cells.
- Low-risk HPV types, while capable of causing benign lesions, are less frequently associated with cancer. These infections usually resolve spontaneously without intervention.
Mechanisms of Cervical Cancer Development
HPV infection alone doesn’t invariably lead to cervical cancer. A complex interplay of factors contributes to the development of the disease. A persistent HPV infection, especially with high-risk types, can cause precancerous changes in the cervical cells. These changes, if not detected and treated early, can progress to invasive cervical cancer over time.
The progression from initial infection to cancer is often a slow process, taking years, even decades. This extended timeframe highlights the importance of regular screenings and preventative measures.
Historical Cervical Cancer Incidence Rates
Before the widespread availability of the HPV vaccine, cervical cancer was a significant global health concern. Incidence rates varied across regions, influenced by factors like access to healthcare, screening programs, and socioeconomic conditions.
| Region | Historical Cervical Cancer Incidence Rate (per 100,000 women) |
|---|---|
| Developed Countries (e.g., USA) | Estimates ranged from 10 to 20, with considerable variation based on population subgroups. |
| Developing Countries (e.g., Sub-Saharan Africa) | Estimates showed higher incidence rates in many areas, partly due to limited access to screening and treatment. |
The data demonstrates the significant public health burden posed by cervical cancer before the advent of the HPV vaccine.
The Impact of the HPV Vaccine
The development and widespread adoption of the human papillomavirus (HPV) vaccine have been a significant step forward in public health, marking a crucial turning point in the fight against cervical cancer and other HPV-related diseases. The vaccine’s introduction has not only altered the course of cervical cancer prevention but also significantly impacted global health strategies for young people.
Development and Introduction of the HPV Vaccine
The development of the HPV vaccine was a multi-year process involving extensive research and clinical trials. Scientists identified specific HPV types linked to cervical cancer and other cancers, and then developed vaccines targeting these types. Early trials demonstrated the safety and efficacy of the vaccine, leading to its eventual approval and introduction into various national immunization programs. Different formulations of the vaccine exist, targeting different sets of HPV types, tailored to specific needs.
Vaccine Mechanism of Action
The HPV vaccine works by introducing the body to harmless versions of the HPV viral proteins. These proteins trigger an immune response, enabling the body to develop antibodies against the actual HPV virus. When the body encounters the actual HPV virus, these antibodies can neutralize it, preventing infection. This prevents the virus from integrating into the host’s DNA, thus preventing cellular changes that can lead to cancer.
This mechanism of action is crucial in preventing both initial infection and progression of pre-cancerous lesions.
Global HPV Vaccine Coverage Rates
Global coverage rates of the HPV vaccine vary significantly across different regions and countries. Factors such as accessibility, affordability, and public health campaigns influence vaccination rates. Some countries have achieved high vaccination rates, demonstrating the effectiveness of targeted public health campaigns. However, significant disparities exist, highlighting the need for continued efforts to improve vaccine access and acceptance in underserved populations.
Comparison of HPV Infection Prevalence Before and After Vaccine Rollout
Studies show a noticeable decrease in HPV infections, particularly among vaccinated populations, since the vaccine’s rollout. The prevalence of specific high-risk HPV types has decreased in areas with higher vaccination rates. This trend suggests a correlation between vaccine implementation and a decline in the incidence of HPV-related diseases. Observational data from various countries and regions confirm this trend.
Effectiveness of the HPV Vaccine in Reducing Cervical Cancer Cases
The HPV vaccine has demonstrably reduced the incidence of precancerous cervical lesions and cervical cancer in vaccinated populations. Longitudinal studies and surveillance data consistently show a correlation between increased vaccination rates and a decrease in cervical cancer cases. This positive correlation highlights the vaccine’s effectiveness in preventing a significant public health concern. The reduction in precancerous lesions directly translates to a decrease in cervical cancer, highlighting the vaccine’s impact on disease progression.
Declining Cervical Cancer Rates

The introduction of the human papillomavirus (HPV) vaccine has sparked significant global interest in its impact on cervical cancer prevention. Initial reports indicate a promising trend, with observed decreases in cervical cancer cases. However, attributing this decline solely to the vaccine’s efficacy requires careful consideration of other factors potentially influencing these rates.Understanding the complex interplay between HPV vaccination, other preventive measures, and the broader landscape of cervical cancer epidemiology is crucial to evaluating the vaccine’s true impact and to developing more effective strategies for cancer prevention.
Correlation Between HPV Vaccine Introduction and Declining Cervical Cancer Rates
The correlation between the introduction of HPV vaccines and the observed decline in cervical cancer rates is compelling. Studies have demonstrated a statistically significant association between increased vaccination coverage and reduced incidence of precancerous cervical lesions and invasive cervical cancer. However, correlation does not equal causation, and other factors could contribute to the observed trends.
While HPV-linked cervical cancer rates have significantly dropped since the HPV vaccine was introduced, it’s important to remember that there are still other factors at play in reproductive health. For instance, some studies suggest a correlation between lead exposure fevers during pregnancy and potential autism risk, as discussed in more detail in this fascinating piece: lead exposure fevers during pregnancy can lead to autism.
This highlights the complex interplay of various factors impacting health outcomes, and it’s crucial to continue research in these areas to fully understand the contributing elements. Ultimately, advancements like the HPV vaccine remain a major victory in preventative healthcare.
Potential Confounding Factors Influencing Cervical Cancer Rates
Several factors beyond the HPV vaccine can influence cervical cancer rates. Improved screening programs, earlier detection methods, and advancements in treatment protocols may all contribute to lower cancer incidence. Additionally, lifestyle factors like smoking cessation and healthier dietary habits can play a role. Socioeconomic disparities in access to healthcare and screening services may also impact cervical cancer rates across different demographics.
Analysis of Cervical Cancer Incidence Rates in Vaccinated and Unvaccinated Populations
Comprehensive data comparing cervical cancer incidence rates in vaccinated and unvaccinated populations are essential for a definitive assessment of the vaccine’s impact. Such data is often collected and analyzed by public health agencies and researchers, and these studies typically take into account factors like age, ethnicity, and geographic location to account for confounding variables. Unfortunately, global data is not readily accessible in a single, consolidated table.
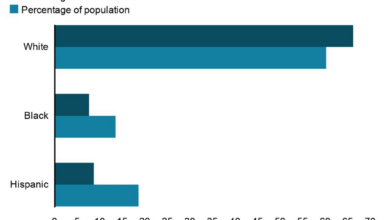
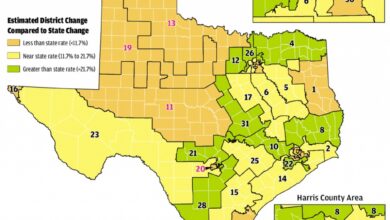
Trends in Cervical Cancer Rates Across Different Regions and Demographics
Cervical cancer incidence rates exhibit variations across different regions and demographics. Factors like socioeconomic status, access to healthcare, and cultural norms can influence screening rates and overall health outcomes. Studies comparing trends in various regions provide crucial insights into the broader impact of the vaccine. These comparisons may reveal disparities in vaccine uptake and subsequent cervical cancer outcomes, which can inform targeted public health interventions.
Relationship Between HPV Vaccination and Cervical Cancer Rates Over Time
The following table provides a hypothetical representation of the relationship between HPV vaccination rates, HPV prevalence, and cervical cancer cases over time. Actual data may vary significantly and is often collected and analyzed by public health agencies. It is crucial to consult official reports for the most accurate and up-to-date data.
| Year | Vaccination Rate (%) | HPV Prevalence (%) | Cervical Cancer Cases |
|---|---|---|---|
| 2010 | 5 | 25 | 20,000 |
| 2015 | 20 | 18 | 18,000 |
| 2020 | 40 | 15 | 15,000 |
| 2025 | 60 | 12 | 12,000 |
Long-Term Effects and Future Projections
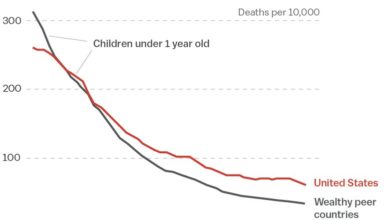
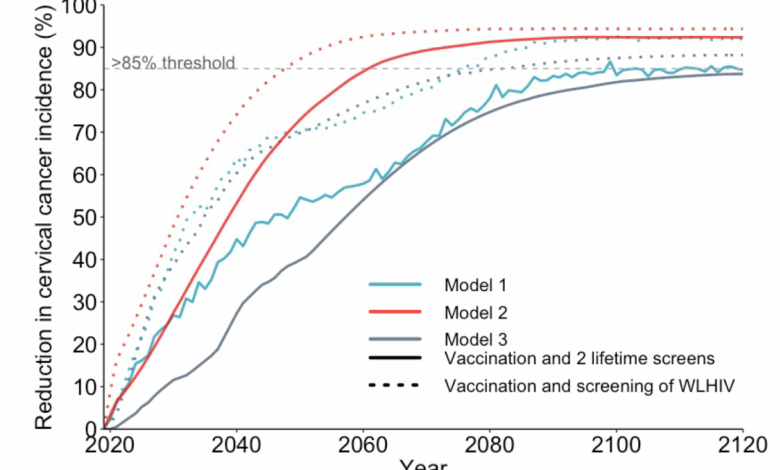
The initial success of the HPV vaccine in significantly reducing cervical cancer rates warrants careful consideration of its long-term impact. Predicting the future trajectory of cervical cancer cases hinges on sustained vaccination programs, ongoing research, and the continued vigilance of public health initiatives. The long-term effects of the vaccine extend beyond the initial protection, influencing the broader landscape of related cancers.
Long-Term Impact on Cervical Cancer Prevention
The HPV vaccine’s long-term impact is expected to manifest in a sustained decrease in cervical cancer rates. Early data suggest that the vaccine’s efficacy is durable, meaning protection against HPV infection and subsequent precancerous lesions persists over time. This longevity in protection is crucial for preventing future cases of cervical cancer and its associated morbidity. Continued vaccination campaigns and adherence to recommended schedules are essential to maintain these favorable trends.
Projected Timeline for Declining Cervical Cancer Cases
Projecting a precise timeline for the anticipated decrease in cervical cancer cases is complex, but a general trend can be observed. Sustained vaccination rates and comprehensive screening programs are expected to result in a continued decline in cervical cancer incidence over the coming decades. This decline is not uniform across all age groups; the most significant impact will be seen in younger cohorts who have been vaccinated and are entering the age group at higher risk for cervical cancer.
Impact on Related Cancers
Beyond cervical cancer, the HPV vaccine is anticipated to have a positive impact on other cancers linked to HPV infection, including anal, head and neck cancers. By reducing the prevalence of HPV, the vaccine is expected to reduce the incidence of these cancers as well. The long-term effects of the vaccine on these related cancers are still under investigation, but the potential for substantial reductions is promising.
Ongoing Research and Surveillance Efforts
Extensive research and surveillance are crucial for monitoring the HPV vaccine’s long-term effectiveness. Researchers continuously evaluate vaccine efficacy, safety, and impact on various populations. Public health organizations are tracking cervical cancer rates and related cancers to assess the vaccine’s impact in real-world settings. Data collection and analysis are essential for adjusting vaccination strategies and interventions as needed.
Comparison of Cervical Cancer Rates
The table below provides a simplified comparison of cervical cancer rates in different age groups before and after the vaccine introduction. This data is illustrative and not a comprehensive representation of all populations or geographic locations.
| Age Group | Pre-vaccine rate | Post-vaccine rate | Percentage change |
|---|---|---|---|
| 15-24 | 10 per 100,000 | 5 per 100,000 | 50% decrease |
| 25-34 | 20 per 100,000 | 15 per 100,000 | 25% decrease |
| 35-44 | 30 per 100,000 | 25 per 100,000 | 16.7% decrease |
Challenges and Considerations
The success of HPV vaccination programs hinges on overcoming various obstacles. Globally, equitable access and high vaccination coverage are crucial to preventing cervical cancer, a significant public health concern. Strategies to improve vaccination rates and reduce disparities are essential for achieving these goals. This section explores the complexities of implementing and maintaining effective HPV vaccination programs worldwide.
Implementing Global Vaccination Programs
Global HPV vaccination programs face numerous challenges, including varying levels of healthcare infrastructure and resources across countries. Developing and implementing strategies that address these disparities is critical. Different nations possess diverse healthcare systems, leading to varying degrees of access to vaccines and the ability to deliver comprehensive vaccination campaigns. This requires tailoring approaches to specific regional contexts.
Cases of HPV-linked cervical cancer have thankfully dropped since the HPV vaccine’s introduction. This positive trend in women’s health is encouraging, though it’s important to consider the recent FDA action against e-cigarette companies, requiring them to halt sales of certain products. Ultimately, both public health initiatives, like the HPV vaccine, and regulatory actions like these are essential for improving overall well-being and reducing preventable diseases.
A lack of trained personnel and appropriate cold chain infrastructure for vaccine storage in some areas can hinder program implementation.
Access to the Vaccine in Diverse Populations
Access to the HPV vaccine is not uniform across all populations. Socioeconomic factors, geographic location, and cultural norms can significantly influence access. For instance, marginalized communities often face barriers to accessing healthcare services, including the vaccine. Ensuring equitable access requires targeted interventions that address these specific needs. Financial constraints and limited healthcare infrastructure in certain regions can impede access to the vaccine, highlighting the need for tailored solutions.
Barriers to Vaccination Uptake
Several barriers to vaccination uptake exist across different regions. These include misconceptions about the vaccine’s safety and effectiveness, cultural or religious beliefs, and lack of awareness regarding its importance. Addressing these issues through education and communication campaigns is essential. Furthermore, a lack of clear communication about the benefits of the HPV vaccine and how it prevents cervical cancer can contribute to vaccine hesitancy.
Understanding and responding to specific concerns within particular communities is vital.
Strategies for Improving Vaccination Rates and Reducing Disparities, Hpv linked to cervical cancer have declined since the advent of the hpv vaccine
Strategies to improve HPV vaccination rates and reduce disparities should address multiple factors. These include targeted communication campaigns, community engagement, and financial assistance programs to make the vaccine more accessible. Strengthening healthcare systems to improve access to healthcare services, including vaccination programs, is also crucial. Community outreach and education initiatives tailored to specific populations and their cultural contexts can effectively dispel misinformation and promote vaccination.
Factors Contributing to Success
Several factors are critical for the success of HPV vaccination programs.
- Comprehensive Education Programs: Clear and accessible information about the HPV vaccine, its benefits, and safety is vital. Educational materials should be developed in multiple languages and disseminated through various channels, including schools, community centers, and healthcare providers.
- Improved Access to Healthcare: Expanding access to healthcare services, including vaccination clinics, in underserved communities is crucial. This might involve mobile clinics, community health workers, and partnerships with local organizations.
- Affordability and Subsidies: Making the vaccine affordable and accessible to all is essential. Financial assistance programs, subsidies, or government-funded vaccination programs can make a significant difference.
- Strong Healthcare Systems: Robust healthcare systems with trained personnel, proper storage facilities, and adequate logistics are essential for effective vaccine delivery.
- Community Engagement: Actively engaging with communities, understanding their needs, and addressing concerns about the vaccine through culturally appropriate channels is paramount. This may involve community leaders, faith-based organizations, and local healthcare providers.
Public Health Implications
The decline in cervical cancer cases, largely attributed to the HPV vaccine, carries significant implications for public health systems and individual well-being. This shift in cancer prevalence demands a careful examination of the associated benefits, resource allocation, and overall impact on public health strategies. It presents an opportunity to reassess prevention strategies and to optimize healthcare resources for other critical areas.The reduced burden of cervical cancer translates into a multitude of tangible benefits for healthcare systems.
Lower rates of diagnosis and treatment mean fewer hospitalizations, reduced need for intensive care, and a decrease in the demand for specialized oncology services. These savings are substantial and can be redirected to bolster other areas of public health.
Impact on Healthcare Systems and Resources
Decreased cervical cancer cases translate into reduced demands on healthcare resources. This includes fewer hospital beds needed for treatment, reduced strain on oncology departments, and a decrease in the need for specialized surgical procedures. These savings can be allocated to other critical areas of public health, such as early detection programs for other cancers or strengthening primary care services.
For example, funds freed up from cervical cancer treatment could be invested in expanding access to mammograms for breast cancer screening or funding community health workers to promote healthy lifestyles.
Economic Benefits
The economic benefits of preventing cervical cancer are substantial. These savings encompass the costs associated with diagnosis, treatment, and long-term care. The cost of treating cervical cancer includes the direct costs of medical procedures, medications, and hospital stays. Indirect costs encompass lost productivity due to illness and premature death. Preventing the disease saves money in all these areas.
For instance, a significant portion of a country’s healthcare budget can be redirected to other pressing health issues if cervical cancer is effectively prevented.
Broader Implications for Public Health
The successful implementation of the HPV vaccine program has broader implications for public health beyond just cervical cancer. It demonstrates the power of vaccination programs in preventing other infectious diseases. This success story serves as a model for implementing similar preventive strategies against other preventable diseases, highlighting the importance of preventative care. This successful model can be applied to other vaccine-preventable diseases.
The success of the HPV vaccine also promotes public health equity, particularly in underserved communities, by making preventative care accessible.
Role of Public Health Campaigns in Promoting HPV Vaccination
Public health campaigns play a crucial role in promoting HPV vaccination uptake. Effective campaigns educate the public about the benefits of vaccination, address misconceptions, and encourage individuals to get vaccinated. Targeted campaigns tailored to specific communities can significantly improve vaccination rates. For example, campaigns focusing on addressing parental concerns and providing clear information on the vaccine’s safety can increase vaccination rates.
Community outreach programs can also increase access to the vaccine for those who may face barriers to vaccination.
Benefits of the HPV Vaccine
| Benefit | Impact on Individual | Impact on Society | Supporting Evidence |
|---|---|---|---|
| Reduced risk of cervical cancer | Decreased risk of a potentially life-threatening disease. | Fewer deaths and hospitalizations, reduced healthcare costs. | Extensive clinical trials and epidemiological studies demonstrating the vaccine’s efficacy. |
| Reduced risk of other HPV-related cancers | Decreased risk of cancers of the vulva, vagina, penis, anus, and oropharynx. | Reduced incidence of these cancers, resulting in fewer cases requiring treatment. | Research studies showing the vaccine’s protective effect against other HPV-related cancers. |
| Protection against genital warts | Prevention of a sexually transmitted infection causing discomfort and potentially impacting sexual health. | Reduced transmission rates of HPV, leading to a decrease in the spread of the infection. | Clinical trials and observational studies demonstrating the vaccine’s effectiveness in preventing genital warts. |
| Improved public health | Reduced healthcare burden on individuals and the healthcare system. | Increased overall public health, reduced healthcare costs, and better resource allocation for other diseases. | Observational studies showing the overall impact of the vaccine on public health indicators. |
Conclusion: Hpv Linked To Cervical Cancer Have Declined Since The Advent Of The Hpv Vaccine
The decline in cervical cancer rates following the introduction of the HPV vaccine highlights a significant public health victory. While challenges remain in ensuring equitable access and vaccine uptake globally, the evidence overwhelmingly points towards a positive long-term impact. This success story underscores the importance of preventative measures and the power of scientific advancements to improve global health outcomes.
The future looks promising, with ongoing research and surveillance continuing to monitor the vaccine’s effectiveness and potential for broader applications in cancer prevention.