15 percent of people who survive heart attacks develop PTSD. This sobering statistic highlights a hidden emotional toll often overlooked in the aftermath of a life-altering event. Survivors face a complex journey, grappling with physical recovery while navigating the psychological scars of trauma. Understanding the prevalence, mechanisms, and treatment options for PTSD in this population is crucial for improving patient care and well-being.
The profound impact of PTSD on heart attack survivors extends beyond the individual, affecting their relationships, social interactions, and overall quality of life. This blog post delves into the various facets of this issue, exploring the underlying mechanisms, potential risk factors, and crucial steps toward recovery.
Prevalence and Impact of PTSD after Heart Attacks
The experience of a heart attack is profoundly impactful, leaving lasting emotional scars for some survivors. While physical recovery is often a significant focus, the potential for post-traumatic stress disorder (PTSD) development is a crucial aspect of long-term well-being. This blog post explores the prevalence, impact, and risk factors associated with PTSD in heart attack survivors.Understanding the prevalence and nature of PTSD following a heart attack is essential for developing targeted support systems and interventions.
It’s a sobering statistic: 15 percent of people who survive heart attacks develop PTSD. This underscores the profound impact these events have on the human psyche. Fortunately, stem cell research advancing rapidly here is offering promising avenues for treating not just the physical damage but also the psychological scars. This research could significantly improve the recovery process for those suffering from this type of trauma.
This condition can profoundly affect a person’s life, impacting both their mental and physical health, as well as their social and economic well-being.
Prevalence of PTSD in Heart Attack Survivors
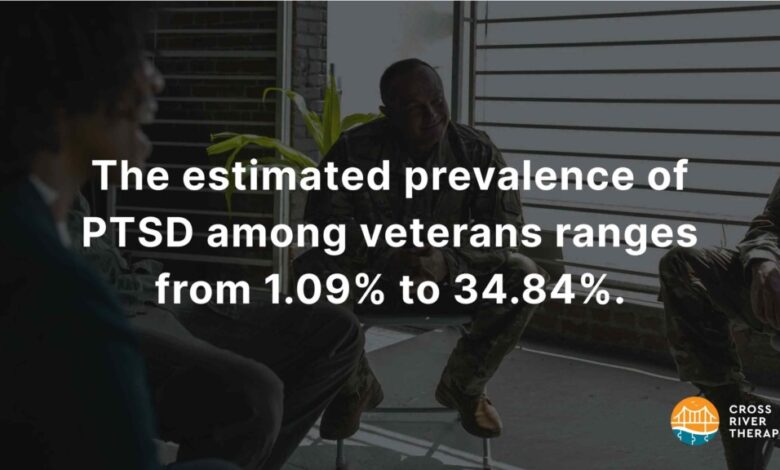
A significant portion of heart attack survivors experience symptoms consistent with PTSD. Research indicates that the prevalence rate varies, but a substantial number, estimated to be around 15% of those who survive a heart attack, experience PTSD. This figure highlights the need for increased awareness and specialized support for this population. This percentage is a rough estimate, and the actual figure can vary depending on the study methodology and the specific population sampled.
Long-Term Effects of PTSD on Heart Attack Survivors
PTSD following a heart attack can have a multifaceted impact on a survivor’s well-being. The emotional distress associated with PTSD can exacerbate existing cardiovascular risks and potentially contribute to future cardiac events. Furthermore, the persistent anxiety, fear, and intrusive thoughts can significantly impair daily functioning, impacting work, relationships, and overall quality of life. PTSD can manifest in various ways, such as flashbacks, nightmares, and avoidance behaviors, impacting the survivor’s ability to cope with daily stressors.
Societal Impact of PTSD in Heart Attack Survivors
The societal impact of PTSD in heart attack survivors extends beyond the individual. The economic burden associated with PTSD can be substantial, encompassing lost productivity, increased healthcare costs, and potential disability claims. Furthermore, the strain on social support systems and healthcare resources can place a significant burden on communities and healthcare systems. In addition to direct costs, there are indirect costs, including lost productivity and reduced quality of life, which impact the wider society.
Risk Factors for Developing PTSD after a Heart Attack
Several factors may increase the likelihood of developing PTSD after a heart attack. These factors can include the severity of the heart attack, the perceived threat to life, the experience of loss or change in lifestyle, and the level of social support available during and after the event. Individuals with pre-existing mental health conditions may also be at a higher risk.
Furthermore, a lack of adequate coping mechanisms or support systems can contribute to the development of PTSD.
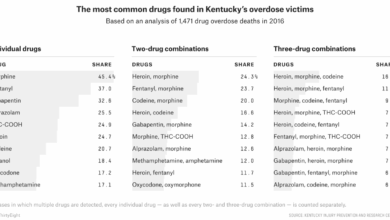
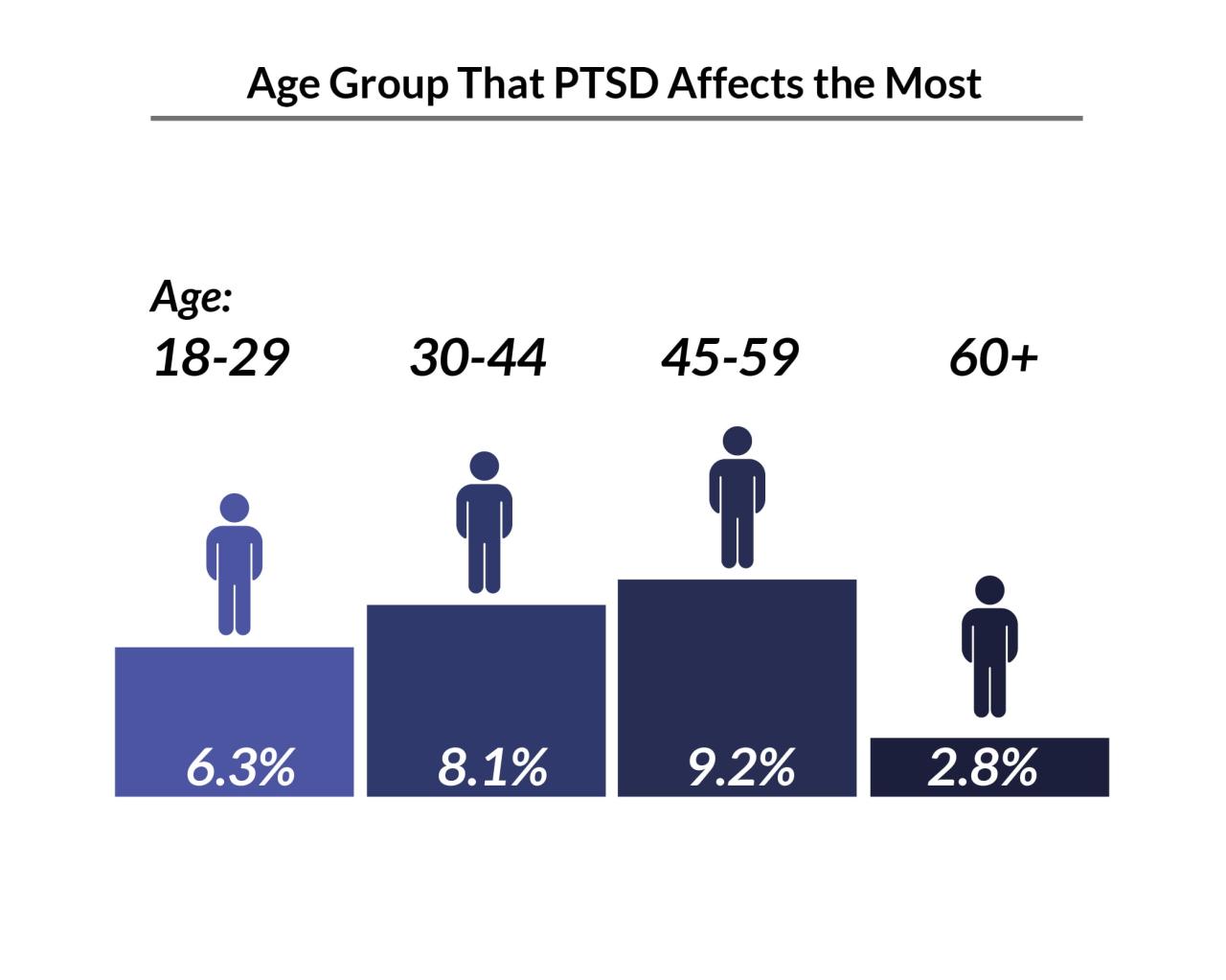
Demographic Comparison of PTSD Prevalence
| Demographic | Estimated Prevalence of PTSD (%) | Explanation |
|---|---|---|
| Age (e.g., 35-54) | 15-20% | Younger survivors may have a higher incidence due to lifestyle changes and concerns about future health. |
| Gender | Slightly higher in women | Potential disparities in coping mechanisms and access to support networks. |
| Socioeconomic Status (e.g., lower income) | Potentially higher | Increased stress from financial strain and limited access to resources. |
The table provides a comparative overview, but precise figures depend on specific research studies and methodologies.
Underlying Mechanisms of PTSD Development: 15 Percent Of People Who Survive Heart Attacks Develop Ptsd
The aftermath of a heart attack can be profoundly impactful, extending beyond physical recovery to encompass the psychological realm. A significant percentage of survivors experience Post-Traumatic Stress Disorder (PTSD), highlighting the complex interplay between biological and psychological factors. Understanding these mechanisms is crucial for developing effective interventions and support systems.The experience of a heart attack is undeniably traumatic.
The fear of death, the uncertainty surrounding the future, and the physical limitations that often follow can trigger profound emotional responses. This trauma, combined with the biological changes associated with the event, creates a fertile ground for PTSD development. A critical understanding of these underlying mechanisms is necessary to better equip individuals and healthcare professionals in providing the most appropriate support.
Biological Mechanisms
The body’s response to a heart attack involves a cascade of physiological changes, including the release of stress hormones like cortisol and adrenaline. These hormones, while crucial for the initial “fight-or-flight” response, can have long-lasting effects on the brain and nervous system if prolonged. Elevated cortisol levels can impair the hippocampus, a brain region essential for memory and emotional regulation.
This impairment can lead to difficulties processing and integrating the traumatic experience, contributing to the development of PTSD symptoms. Furthermore, the disruption to the body’s neurochemical balance, including the levels of norepinephrine and serotonin, can also play a role in the development of anxiety, fear, and emotional dysregulation.
Psychological Mechanisms
Pre-existing mental health conditions can significantly increase the vulnerability to PTSD after a heart attack. Individuals with prior anxiety disorders, depression, or other mental health issues may have a lower threshold for experiencing post-traumatic stress, making them more susceptible to developing PTSD following the trauma of a heart attack. This underscores the importance of addressing and managing any pre-existing conditions prior to and following a heart attack.
For example, a patient with a history of depression might experience more severe symptoms of PTSD, making them more likely to experience prolonged distress and difficulty coping with the recovery process.
Acute Stress Response
The acute stress response, characterized by the release of stress hormones, is a natural bodily response to perceived threats. In the context of a heart attack, this response can be overwhelming and prolonged, potentially leading to an overactivation of the stress response system. This heightened activation can contribute to the development of PTSD symptoms, including intrusive thoughts, flashbacks, nightmares, and emotional distress.
For example, a patient experiencing intense chest pain and fear during a heart attack might experience a more pronounced acute stress response, leading to a heightened risk of developing PTSD symptoms later on.
Coping Mechanisms and Stress Management
Effective coping mechanisms and stress management techniques can significantly reduce the risk of PTSD development or mitigate its severity. These strategies focus on helping individuals regulate their emotions, manage stress, and develop healthier ways to cope with the challenges they face.
| Coping Mechanism | Description |
|---|---|
| Mindfulness Meditation | Practicing mindfulness helps individuals focus on the present moment, reducing rumination on past trauma and anxiety about the future. |
| Cognitive Behavioral Therapy (CBT) | CBT helps individuals identify and challenge negative thought patterns and develop healthier coping strategies for managing stress and anxiety. |
| Support Groups | Connecting with others who have experienced similar trauma can provide emotional support, validation, and a sense of community. |
| Physical Exercise | Regular physical activity can help reduce stress hormones, improve mood, and promote a sense of well-being. |
| Healthy Diet | A balanced diet provides essential nutrients for optimal brain function and stress management. |
Identification and Treatment of PTSD in Heart Attack Survivors
Navigating the emotional aftermath of a heart attack can be incredibly challenging. While the physical recovery is a significant focus, the psychological impact often goes unaddressed, leading to Post-Traumatic Stress Disorder (PTSD) in a substantial portion of survivors. Understanding the specific symptoms, diagnostic approaches, and effective treatments is crucial for supporting these individuals and promoting their well-being.Identifying and addressing PTSD in heart attack survivors is vital for their long-term recovery.
The emotional trauma associated with a life-threatening event like a heart attack can trigger a range of psychological responses, some of which may manifest as PTSD. Early detection and intervention are key to minimizing the negative impact of PTSD and improving overall health outcomes.
Common Symptoms of PTSD in Heart Attack Survivors
Recognizing the specific symptoms of PTSD in heart attack survivors can facilitate timely intervention and appropriate treatment. These symptoms can vary from person to person but often include intrusive thoughts related to the event, avoidance of situations that trigger reminders of the attack, negative emotional states like anxiety and depression, and heightened physiological responses like increased heart rate or sweating in response to reminders.
The constant fear of another heart attack can also be a significant symptom, affecting daily life and relationships.
Potential Diagnostic Tools for PTSD in This Population
Several diagnostic tools can be employed to assess the presence and severity of PTSD in heart attack survivors. These tools typically involve structured interviews and self-report questionnaires designed to measure the severity of PTSD symptoms. Examples include the Posttraumatic Diagnostic Scale (PDS) and the Clinician-Administered PTSD Scale (CAPS). Furthermore, clinicians may use a combination of structured interviews, observations of behavior, and clinical judgment to arrive at a diagnosis.
These approaches ensure a comprehensive evaluation of the individual’s experiences and mental health status.
Importance of Early Intervention and Treatment for PTSD
Early intervention and treatment for PTSD after a heart attack are critical for several reasons. Firstly, untreated PTSD can exacerbate existing physical health issues, leading to increased cardiovascular risks and decreased quality of life. Secondly, PTSD can impede the individual’s ability to engage in lifestyle changes necessary for long-term cardiovascular health. Thirdly, early intervention can prevent the development of chronic PTSD symptoms, which can significantly impact social and occupational functioning.
A timely and appropriate response can make a substantial difference in recovery and future well-being.
Examples of Evidence-Based Therapies
Various evidence-based therapies have proven effective in treating PTSD in general populations, and these approaches can be adapted for heart attack survivors. Cognitive Behavioral Therapy (CBT) is a highly effective method for helping individuals identify and modify negative thought patterns and behaviors associated with PTSD. Exposure therapy, another evidence-based approach, gradually exposes individuals to trauma-related stimuli in a safe and controlled environment, reducing avoidance behaviors and emotional distress.
Eye Movement Desensitization and Reprocessing (EMDR) is another therapeutic approach that has demonstrated efficacy in treating PTSD by using guided eye movements or other forms of bilateral stimulation.
Table: Types of Therapy for PTSD in Heart Attack Survivors
| Therapy Type | Effectiveness | Suitability for Heart Attack Survivors |
|---|---|---|
| Cognitive Behavioral Therapy (CBT) | High – effective in modifying thought patterns and behaviors | High – can address anxiety and maladaptive thoughts |
| Exposure Therapy | High – gradually reduces avoidance behaviors | Moderate – requires careful consideration of triggering stimuli |
| Eye Movement Desensitization and Reprocessing (EMDR) | Moderate – has shown positive results | High – can be helpful in addressing traumatic memories |
| Acceptance and Commitment Therapy (ACT) | Moderate – focuses on acceptance and values-based actions | High – can be particularly useful in managing stress and promoting emotional regulation |
Risk Factors and Protective Factors
Heart attacks are devastating events, and the aftermath can be emotionally challenging. Post-traumatic stress disorder (PTSD) can develop in a significant portion of survivors, impacting their long-term well-being. Understanding the risk and protective factors is crucial for developing effective interventions and support systems. This exploration delves into the factors that contribute to PTSD development, as well as those that can buffer against it.While the exact mechanisms are complex, several factors increase the vulnerability to PTSD after a heart attack.
These are not simply isolated events, but interact in complex ways, highlighting the multifaceted nature of the human response to trauma. Identifying and addressing these factors is essential for improving outcomes.
Risk Factors for PTSD
The experience of a heart attack is inherently stressful. Factors like the severity of the attack, the perceived threat to life, and the degree of perceived loss of control can significantly increase the risk of PTSD development. Pre-existing mental health conditions, such as anxiety or depression, can also heighten vulnerability. The perception of the event as life-threatening and the ensuing uncertainty about the future play a substantial role in the development of PTSD symptoms.
It’s sobering to learn that a significant 15 percent of people who survive heart attacks develop PTSD. While Australia’s proactive approach to cancer prevention, like using the HPV vaccine to eliminate cervical cancer, highlighting the importance of preventative measures , the psychological toll of such life-altering events is still a crucial area of concern. This highlights the broader need for comprehensive support systems for those experiencing trauma after surviving a heart attack.
The immediate aftermath, including the need for intensive care and prolonged recovery, contributes to the risk.
- Severity of the heart attack: A more severe heart attack, requiring extensive medical intervention, can lead to increased anxiety and fear about future health. This can manifest as intrusive thoughts and flashbacks related to the event.
- Perceived threat to life: If the individual perceives the heart attack as a life-threatening event, the associated fear and anxiety can contribute to PTSD development. This is especially true if the experience involved a sense of helplessness or being out of control.
- Pre-existing mental health conditions: Individuals with pre-existing anxiety or depression are more susceptible to developing PTSD after a heart attack. These conditions can make it harder to cope with the stress of the event and its aftermath.
- Social isolation: A lack of social support or a strained family relationship can increase the risk of PTSD. The absence of a supportive network can intensify feelings of isolation and vulnerability.
Protective Factors Against PTSD
Despite the heightened risk, protective factors can mitigate the development of PTSD. These factors often involve individual coping mechanisms, resilience, and social support.
- Strong social support network: A robust network of family and friends offering emotional and practical assistance can significantly reduce the risk of PTSD. The feeling of connection and shared responsibility can be a crucial buffer against negative emotions.
- Effective coping mechanisms: Individuals who utilize healthy coping mechanisms, such as exercise, mindfulness, or engaging in hobbies, can better manage the stress associated with a heart attack. These strategies can reduce the intensity of negative emotions and promote a sense of control.
- Positive outlook and resilience: Individuals with a positive outlook and a history of resilience are more likely to recover from the trauma of a heart attack without developing PTSD. A belief in one’s ability to overcome challenges can significantly influence the outcome.
Comparing Coping Mechanisms
Different coping mechanisms can influence the development of PTSD. Active coping strategies, such as seeking support or engaging in problem-solving, are often more effective than passive coping strategies. Learning and practicing relaxation techniques can be beneficial in reducing anxiety and promoting emotional regulation.
- Active coping: Active coping strategies, such as problem-solving and seeking support, are often more effective than passive coping strategies. This includes actively working through the challenges and seeking help from others.
- Passive coping: Passive coping mechanisms, such as avoidance or denial, can prolong the stress response and increase the risk of PTSD. These strategies tend to exacerbate the negative emotions associated with the trauma.
Influence of Social Support
Social support plays a pivotal role in the recovery process. A strong support system can provide emotional comfort, practical assistance, and a sense of belonging.
It’s sobering to think that a significant 15 percent of heart attack survivors develop PTSD. This highlights the profound impact of trauma on mental well-being. Interestingly, improving financial stability through initiatives like raising the minimum wage can demonstrably boost mental health, as explored in this insightful article on how raising the minimum wage can be a win for mental health.
Ultimately, addressing the root causes of stress and hardship, like ensuring fair wages, could significantly reduce the number of people facing PTSD after a heart attack.
| Support System | Effectiveness | Impact on PTSD |
|---|---|---|
| Strong family relationships | High | Reduces feelings of isolation and provides consistent emotional support. |
| Supportive friends | Moderate | Offers companionship and can provide a sense of community during recovery. |
| Professional support groups | High | Provides a safe space to share experiences and connect with others facing similar challenges. |
| Community resources | Variable | Access to resources like counseling and support groups can be influential in recovery. |
Comparison with Other Stressful Medical Events
Experiencing a serious medical event like a heart attack, cancer, or stroke can be profoundly traumatic, impacting mental well-being alongside physical recovery. Understanding how PTSD develops in response to these events requires careful consideration of the similarities and differences in the experiences, as well as the individual coping mechanisms employed. This comparison can help in identifying risk factors and potentially developing more effective interventions for PTSD prevention and treatment.While the specific stressors and coping strategies vary across different medical events, the underlying psychological processes contributing to PTSD development often share common threads.
The unpredictability, loss of control, and potential for future health complications are key factors in each case, impacting an individual’s emotional well-being. The intensity of the experience, duration of illness, and perceived threat to life also play a significant role.
Similarities in PTSD Development Across Medical Events
The shared experience of a serious illness often leads to a similar set of psychological reactions. These include anxiety, fear, and a profound sense of vulnerability. Individuals may experience difficulties with concentration, sleep, and memory, impacting their overall quality of life. A loss of control over one’s health trajectory is a common factor across medical events. This loss of control can manifest in feelings of helplessness and powerlessness.
Differences in the Experience of Medical Events
The specific nature of each medical event shapes the individual experience, influencing how PTSD develops. A heart attack, for example, often involves a sudden and acute awareness of mortality and a potential disruption to future plans. Cancer, on the other hand, typically involves a longer, more protracted period of uncertainty and treatment. Stroke can present with rapid onset and significant neurological deficits, potentially impacting daily functioning and independence.
Perceived Control Over the Situation
The degree to which an individual perceives control over their situation plays a crucial role in PTSD development. For example, a heart attack survivor who feels empowered to actively participate in their recovery and actively manages their treatment may experience less PTSD compared to someone who feels helpless and overwhelmed by the situation.
Coping Strategies Employed
Individuals facing different medical crises employ diverse coping strategies. Some individuals might rely on social support, seeking comfort and guidance from family and friends. Others might turn to self-reliance, prioritizing personal strength and independence. The availability and perceived effectiveness of these strategies can significantly impact the individual’s mental health outcomes.
Comparison Table of PTSD Development Across Medical Events
| Medical Event | Nature of Event | Potential Impact on PTSD | Coping Strategies |
|---|---|---|---|
| Heart Attack | Sudden, acute awareness of mortality; potential disruption to future plans | Heightened anxiety, fear of recurrence, feelings of vulnerability | Social support, active participation in recovery, seeking professional guidance |
| Cancer | Protracted period of uncertainty, treatment, potential for long-term effects | Fear of recurrence, loss of control over future, body image concerns | Social support, seeking spiritual guidance, focusing on positive aspects of life |
| Stroke | Rapid onset, significant neurological deficits; potential impact on daily functioning and independence | Anxiety, fear of future, difficulty adapting to changes in daily life | Rehabilitation, adapting to new limitations, focusing on positive social interactions |
Public Health Implications and Prevention Strategies
A heart attack is a devastating experience, and the potential for post-traumatic stress disorder (PTSD) adds another layer of complexity to recovery. Understanding the public health implications of PTSD in heart attack survivors is crucial for developing effective preventative strategies and improving long-term well-being. By addressing the mental health needs of these individuals, we can foster a healthier and more supportive environment for recovery.The significant prevalence of PTSD in heart attack survivors underscores the importance of proactive measures aimed at reducing its occurrence.
This necessitates a multifaceted approach encompassing individual-level interventions, support systems, and broader societal changes to promote mental resilience. Prevention is key, not only to mitigating the psychological distress but also to fostering better physical health outcomes.
Public Health Implications of PTSD in Heart Attack Survivors
The public health implications extend beyond the individual experience. Increased rates of PTSD among heart attack survivors contribute to a higher burden on healthcare systems. This manifests in elevated healthcare costs, increased demand for mental health services, and potential long-term economic consequences for both individuals and society. Furthermore, the social stigma associated with mental health conditions can hinder open discussion and appropriate support seeking.
Preventative Measures to Reduce PTSD Incidence
Early identification and intervention are paramount in reducing the incidence of PTSD following a heart attack. Comprehensive pre- and post-heart attack psychological support can be vital. This includes educating patients and their families about the potential for PTSD, and offering coping strategies to manage stress and anxiety. Proactive and tailored support systems are critical to successful recovery.
Educational Materials for Patients and Healthcare Providers
Creating accessible and comprehensive educational resources is essential for both patients and healthcare providers. These materials should include:
- Information on the risk factors and warning signs of PTSD.
- Guidance on stress management techniques, such as relaxation exercises and mindfulness practices.
- Detailed information on available support services, including therapists, support groups, and helplines.
- Educational materials for healthcare providers on recognizing and addressing PTSD symptoms in heart attack survivors.
Clear and concise information empowers patients and healthcare providers to proactively address potential mental health challenges.
Role of Preventative Strategies in Improving Long-Term Outcomes
Proactive preventative strategies are not merely about reducing PTSD incidence; they play a critical role in improving the overall long-term outcomes for heart attack survivors. By equipping individuals with coping mechanisms and access to support systems, we enhance their ability to manage stress, reduce the risk of relapse, and foster a more positive recovery trajectory. This proactive approach leads to better physical and mental well-being, potentially improving adherence to medical treatments, and promoting a higher quality of life.
Costs and Benefits of Prevention Strategies, 15 percent of people who survive heart attacks develop ptsd
The following table illustrates a potential cost-benefit analysis of different prevention strategies:
| Prevention Strategy | Estimated Costs | Potential Benefits (Reduced PTSD Cases/Improved Quality of Life) | Return on Investment |
|---|---|---|---|
| Comprehensive pre- and post-heart attack psychological support | $X (variable depending on intensity and duration) | Y number of PTSD cases averted/improved quality of life scores | Z (calculated as the cost saved through reduced healthcare expenses, increased productivity, and reduced long-term disability claims) |
| Educational programs for patients and healthcare providers | $A (variable depending on reach and intensity) | Reduced incidence of PTSD/increased awareness | B (calculated as the cost savings through reduced healthcare expenses and increased productivity) |
| Community support groups and helplines | $C (variable depending on structure and reach) | Improved access to support/reduced isolation | D (calculated as the cost savings through reduced healthcare expenses and improved social well-being) |
Note: “X”, “Y”, “Z”, “A”, “B”, “C”, and “D” represent variable values dependent on specific program designs and local contexts.The table highlights the potential return on investment associated with various prevention strategies. A comprehensive approach, combining multiple strategies, is likely to yield the most substantial benefits.
Case Studies and Examples
Heart attacks are devastating events, impacting not only physical health but also mental well-being. A significant portion of survivors experience Post-Traumatic Stress Disorder (PTSD). Understanding the lived experiences of these individuals can illuminate the complex interplay of factors contributing to PTSD development and highlight the importance of tailored support systems and therapies. This section presents three case studies, illustrating how these factors play out in real life and showcasing the journeys of recovery.
Case Study 1: The Unexpected Aftermath
Amelia, a 52-year-old teacher, suffered a sudden heart attack while exercising. The intense fear and uncertainty surrounding the event, coupled with the physical limitations imposed by her recovery, led to feelings of anxiety and helplessness. She struggled with intrusive thoughts about the near-death experience and avoided any physical activity that resembled her pre-attack routine. Amelia’s social isolation worsened her condition, as she felt unable to engage in her usual activities.
Her support system, while loving, struggled to fully grasp the depth of her emotional distress. She eventually sought therapy, learning coping mechanisms and regaining a sense of control over her life.
Case Study 2: The Loss of Identity
David, a 65-year-old retired engineer, experienced a heart attack during a routine checkup. The unexpected nature of the event, coupled with the significant lifestyle changes required for his recovery, caused him to question his sense of purpose and identity. He felt like he had lost his role as a provider and a valued member of his community. This loss of identity manifested in feelings of hopelessness and despair.
He benefited greatly from joining a support group for heart attack survivors, where he connected with others who understood his struggles. The shared experiences and encouragement from others provided a sense of belonging and helped him regain a sense of purpose. He also participated in counseling, which provided him with coping strategies and tools to manage his PTSD symptoms.
Case Study 3: The Fear of Recurrence
Maria, a 48-year-old businesswoman, experienced a heart attack during a stressful work event. The intense fear of another attack, coupled with the anxiety surrounding the uncertainty of her future, contributed significantly to her PTSD. She developed anxiety and panic attacks in high-stress situations, such as meetings or presentations, which further complicated her professional life. Recognizing the importance of managing her anxiety, Maria sought professional help.
Cognitive behavioral therapy (CBT) helped her challenge her negative thoughts and develop healthier coping mechanisms for managing stress and anxiety. Her support system, comprising her close friends and family, played a crucial role in her recovery. They provided emotional support and encouragement, fostering a safe environment for her to heal.
Summary of Case Studies
| Case Study | Triggering Event | Illustrative Factors | Recovery Journey |
|---|---|---|---|
| Amelia (Unexpected Aftermath) | Sudden heart attack during exercise | Fear, uncertainty, physical limitations, social isolation | Therapy, coping mechanisms, regaining control |
| David (Loss of Identity) | Heart attack during routine checkup | Unexpected nature, lifestyle changes, loss of purpose | Support group, counseling, regaining sense of purpose |
| Maria (Fear of Recurrence) | Heart attack during a stressful work event | Fear of another attack, anxiety about future | CBT, healthier coping mechanisms, support system |
Conclusion
In conclusion, the development of PTSD following a heart attack is a significant concern requiring comprehensive understanding and proactive support. The 15% statistic underscores the need for improved awareness, early intervention, and tailored treatment strategies. By acknowledging the complexities of this issue, healthcare professionals and support systems can empower survivors to navigate this challenging experience and foster lasting recovery.