Acromegaly and heart failure: a complex interplay of hormonal imbalances and cardiovascular complications. This intricate relationship involves a cascade of effects, from the underlying cause of acromegaly to the resulting heart failure. We’ll explore the mechanisms, symptoms, diagnostics, and treatments involved in this challenging condition, providing a comprehensive understanding for those affected and interested in learning more.
Acromegaly, characterized by excessive growth hormone production, can lead to significant heart problems. The hormonal dysregulation impacts the heart’s structure and function, potentially leading to conditions like cardiac hypertrophy and dysfunction. This article will delve into the pathophysiology, clinical manifestations, and treatment strategies for this often-overlooked connection between acromegaly and heart failure.
Introduction to Acromegaly and Heart Failure
Acromegaly is a rare hormonal disorder characterized by the persistent overproduction of growth hormone (GH) by the pituitary gland. This excess GH leads to abnormal growth and thickening of bones, soft tissues, and organs throughout the body. The uncontrolled growth hormone surge affects multiple systems, including the cardiovascular system, potentially leading to various complications. This condition, if left untreated, can significantly impact quality of life and increase the risk of serious health problems.The link between acromegaly and heart failure is complex.
While acromegaly doesn’t directly cause heart failure, the chronic overproduction of growth hormone can cause structural changes in the heart, including thickening of the heart muscle (hypertrophy), enlargement of the heart chambers, and increased blood pressure. These alterations can strain the heart’s ability to pump blood efficiently, eventually leading to heart failure. The mechanisms involve multiple pathways, including direct effects on cardiac tissue and the indirect effects of hypertension.
Underlying Cause of Acromegaly
Acromegaly arises from a benign tumor, typically a pituitary adenoma, that secretes excessive growth hormone. This tumor, though benign, can disrupt the normal hormonal balance in the body, leading to a cascade of effects on various organs and tissues.
Impact of Acromegaly on the Heart
The persistent overproduction of growth hormone in acromegaly can directly affect the heart. It leads to thickening of the heart muscle (hypertrophy), enlargement of the heart chambers, and increased blood pressure. These changes impair the heart’s ability to pump blood effectively, which can increase the risk of developing heart failure. Symptoms such as chest pain and shortness of breath can occur due to these structural changes and the increased workload on the heart.
Symptoms and Signs of Acromegaly and Heart Failure
- Acromegaly: Common symptoms include gradual enlargement of hands and feet, thickened facial features (coarsened facial features), excessive sweating, joint pain, and headaches. Changes in skin texture, such as thickened and leathery skin, can also be present. Other symptoms may include sleep apnea, carpal tunnel syndrome, and visual disturbances.
- Heart Failure: Common symptoms of heart failure include shortness of breath (dyspnea), especially during exertion or when lying down, fatigue, swelling in the legs, ankles, and feet (edema), persistent cough, and chest pain or discomfort. These symptoms may vary in intensity and presentation depending on the severity of the heart failure.
Importance of Early Diagnosis and Treatment
Early diagnosis and prompt treatment of both acromegaly and heart failure are crucial for improving patient outcomes. Early intervention in acromegaly can prevent the long-term complications, including heart failure, by controlling the excessive growth hormone production. Similarly, early detection and treatment of heart failure can improve the quality of life and potentially slow or halt disease progression. Treatment options for acromegaly include surgical removal of the pituitary tumor, radiation therapy, and medications to suppress growth hormone secretion.
Treatment for heart failure involves managing the underlying cause, medications to improve heart function, and lifestyle modifications.
Key Differences Between Acromegaly and Heart Failure
| Characteristic | Acromegaly | Heart Failure |
|---|---|---|
| Cause | Benign pituitary adenoma secreting excessive growth hormone | Various underlying conditions, including coronary artery disease, hypertension, or valvular heart disease |
| Primary Impact | Systemic growth and thickening of bones, soft tissues, and organs | Impaired ability of the heart to pump blood efficiently |
| Symptoms | Enlarged hands and feet, coarsened facial features, excessive sweating, joint pain, headaches | Shortness of breath, fatigue, edema, persistent cough, chest pain |
| Treatment | Surgical removal, radiation therapy, medications | Lifestyle modifications, medications to improve heart function, treatment of underlying cause |
Pathophysiology of Acromegaly-Related Heart Failure

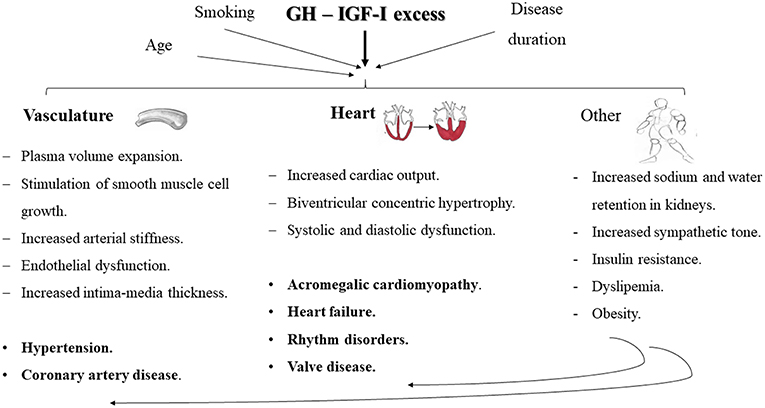
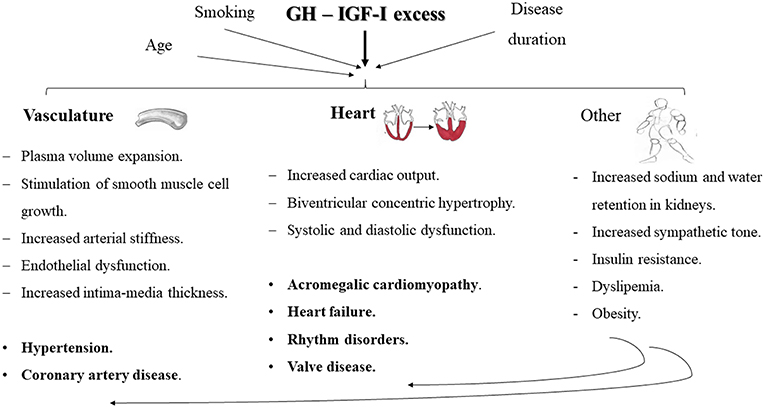
Acromegaly, a hormonal disorder characterized by excessive growth hormone (GH) secretion, often leads to significant cardiovascular complications, including heart failure. The pathophysiology of this association is complex, involving multiple interconnected factors that affect cardiac structure, function, and metabolism. This detailed exploration will illuminate the mechanisms driving the development of heart failure in acromegaly.The excess growth hormone in acromegaly disrupts the delicate balance of hormones within the body.
Acromegaly, a condition causing abnormal growth, often leads to heart issues like heart failure. While researching the potential heart complications in acromegaly, I stumbled upon the complexities of medication side effects, specifically in rheumatoid arthritis. This led me to explore how certain treatments for rheumatoid arthritis can sometimes cause toxicity, impacting overall health, as detailed in toxicity in rheumatoid arthritis medications.
Ultimately, understanding these potential side effects, particularly in the context of acromegaly and its impact on the heart, is crucial for better patient care.
This hormonal imbalance directly impacts the heart, leading to a cascade of events that ultimately contribute to heart failure. Growth hormone, in addition to its effects on bone and soft tissue, also exerts profound influences on cardiac function and metabolism.
Hormonal Imbalances and Cardiac Impact
The overproduction of growth hormone (GH) in acromegaly significantly alters the hormonal milieu. This includes affecting insulin sensitivity, thyroid function, and other hormones critical for maintaining cardiovascular health. The resultant hormonal imbalances directly contribute to the development of cardiac hypertrophy and dysfunction. For instance, elevated GH levels are strongly correlated with impaired glucose metabolism and insulin resistance, which further exacerbates the cardiovascular burden.
This can manifest in elevated blood pressure, lipid abnormalities, and increased risk of atherosclerosis, all factors contributing to the increased strain on the heart.
So, acromegaly and heart failure are a tricky pair. It’s a complex relationship, and understanding the specific ways they intertwine is crucial for effective management. Finding the right support, like in the ultimate guide to sports bras , is important for overall well-being. Proper support for your body, and a holistic approach to managing acromegaly and its effects on the heart, are key to better health.
Molecular Pathways in Cardiac Hypertrophy and Dysfunction
The molecular mechanisms underlying cardiac hypertrophy and dysfunction in acromegaly are multifactorial. Elevated GH levels induce the activation of signaling pathways that promote cardiac myocyte growth and proliferation. This excessive growth, in turn, can lead to an enlargement of the heart (hypertrophy), ultimately impairing its ability to pump blood effectively. Moreover, chronic activation of these pathways can lead to structural and functional abnormalities in the heart’s electrical system, increasing the risk of arrhythmias.
Furthermore, these molecular pathways may also impact the heart’s ability to relax and fill with blood (diastolic function), which can also contribute to heart failure.
Insulin Resistance and Metabolic Syndrome
Insulin resistance, a hallmark of acromegaly, plays a critical role in exacerbating heart failure. The reduced sensitivity to insulin impairs glucose metabolism, leading to elevated blood glucose levels and, subsequently, increased oxidative stress. This oxidative stress further contributes to the damage of cardiac tissues, impairing their function. Furthermore, insulin resistance is often associated with metabolic syndrome, a cluster of metabolic abnormalities that includes obesity, hypertension, and dyslipidemia.
These conditions collectively create a milieu that increases the burden on the heart and accelerate the development of heart failure.
Acromegaly, a hormonal disorder, can unfortunately put a strain on the heart, potentially leading to heart failure. Interestingly, recent research, like a study on how psoriasis medication Otezla might cause fat loss in people with psoriatic arthritis ( psoriasis medication otezla leads to fat loss in people with psoriatic arthritis study says ), highlights the complex interplay between various health conditions.
This underscores the importance of ongoing research to better understand and manage the long-term effects of acromegaly and related cardiovascular issues.
Vascular Changes and Heart Failure
Acromegaly-induced vascular changes significantly contribute to heart failure. The excess growth hormone can lead to thickening and stiffening of the blood vessels, reducing their elasticity and compromising their ability to effectively regulate blood flow. This vascular dysfunction results in increased peripheral resistance, which further elevates blood pressure, placing greater strain on the heart. Moreover, these vascular changes can also lead to atherosclerosis, the buildup of plaque in the arteries, further compromising blood flow to the heart muscle and other vital organs.
This, in turn, contributes to the progression of heart failure.
Comparison of Acromegaly Effects on Organ Systems
| Organ System | Effect of Acromegaly |
|---|---|
| Heart | Cardiac hypertrophy, diastolic dysfunction, increased risk of arrhythmias, impaired contractility, increased risk of heart failure |
| Bones | Enlarged bones, joint pain, arthritis |
| Soft Tissues | Thickening of skin, soft tissue enlargement, increased sweating |
| Endocrine | Insulin resistance, impaired glucose tolerance, thyroid dysfunction |
| Metabolic | Dyslipidemia, hypertension, increased risk of diabetes |
Clinical Manifestations and Diagnosis
Acromegaly, a hormonal disorder characterized by excessive growth hormone production, often leads to significant cardiovascular complications, including heart failure. Understanding the clinical manifestations and diagnostic approaches is crucial for timely intervention and improving patient outcomes. Early detection and management of acromegaly-related heart failure are essential to prevent further complications.
Common Clinical Manifestations of Acromegaly Related to Heart Failure
Acromegaly manifests in various ways, with some symptoms directly affecting the heart. Progressive enlargement of the heart (cardiomegaly) is a common finding, often leading to symptoms like shortness of breath, especially during exertion, and palpitations. Increased blood pressure is frequently observed in individuals with acromegaly, which can contribute to cardiovascular strain and potentially exacerbate heart failure. Other common manifestations, although not directly heart-related, can still impact the heart.
For example, the thickening of soft tissues (such as the tongue and hands) and skin changes can restrict breathing, adding another layer of cardiovascular strain.
Diagnostic Criteria for Acromegaly
Diagnosing acromegaly involves a multi-faceted approach. Blood tests play a crucial role. Elevated levels of growth hormone (GH) and insulin-like growth factor 1 (IGF-1) are key indicators. It’s important to note that a single elevated measurement isn’t definitive; the test must be repeated under specific conditions and confirmed with other tests. Furthermore, imaging studies, particularly MRI scans of the pituitary gland, are essential to identify any tumors or abnormalities in this area, which are the primary source of the excessive GH production.
Specific tests related to heart function, like echocardiograms, are vital for assessing cardiac structure and function, particularly to detect any signs of hypertrophy or other cardiac changes associated with acromegaly.
Role of Echocardiography and Cardiac MRI
Echocardiography is a non-invasive ultrasound technique used to visualize the heart’s structure and function. It can detect abnormalities like cardiac hypertrophy (thickening of the heart muscle), changes in valve function, and signs of diastolic dysfunction (impaired relaxation of the heart). Cardiac MRI provides detailed images of the heart’s anatomy and function. It’s particularly useful for evaluating the extent of myocardial damage and for assessing the presence of any fibrosis, which can indicate long-term heart damage due to acromegaly.
Both echocardiography and cardiac MRI are valuable tools in assessing the severity of acromegaly-related cardiac complications and guiding treatment strategies.
Importance of Thorough Physical Examination and Patient History
A comprehensive physical examination and detailed patient history are crucial elements in the diagnostic process. A healthcare provider should assess for characteristic features of acromegaly, including enlarged hands and feet, facial changes, and thickened skin. The history should cover symptoms such as headaches, visual disturbances (if pituitary tumor is present), and any signs of heart problems, like shortness of breath or chest pain.
A thorough evaluation of the patient’s medical history, including family history of heart disease or other hormonal disorders, can also provide valuable context for the diagnosis.
Comparison of Diagnostic Methods
| Diagnostic Method | Acromegaly | Heart Failure |
|---|---|---|
| Blood Tests (GH, IGF-1) | Essential for detecting elevated hormone levels. | Helpful in assessing electrolyte imbalances and other markers of heart function. |
| Imaging Studies (MRI) | Crucial for identifying pituitary adenomas. | May be used to assess the extent of heart enlargement or other structural abnormalities. |
| Echocardiography | Evaluates cardiac structure and function, detects hypertrophy and dysfunction. | Essential for evaluating ejection fraction, wall thickness, and valve function. |
| Cardiac MRI | Provides detailed images of myocardial tissue, identifies fibrosis and damage. | Provides detailed images of cardiac structures, assesses cardiac function, and helps identify specific types of heart failure. |
| Physical Examination | Identifies characteristic physical features of acromegaly. | Evaluates for symptoms like shortness of breath, edema, and jugular venous distension. |
Treatment Strategies and Management
Acromegaly, a hormonal disorder characterized by excessive growth hormone production, often leads to significant cardiovascular complications, including heart failure. Effective management requires a multi-faceted approach targeting both the underlying acromegaly and the resultant cardiovascular damage. This involves a combination of medical therapies, lifestyle modifications, and diligent monitoring to improve long-term outcomes.Careful management of acromegaly necessitates a tailored strategy, recognizing that each patient’s condition and response to treatment vary.
This includes aggressive treatment of hypertension and other risk factors, lifestyle adjustments, and regular follow-up care to optimize cardiovascular health and overall well-being.
Medical Therapies for Acromegaly
Treatment strategies for acromegaly aim to reduce growth hormone levels and mitigate associated complications. Somatostatin analogs, such as octreotide and lanreotide, are frequently used to suppress growth hormone secretion. These medications work by mimicking the action of somatostatin, a natural hormone that inhibits growth hormone release. Surgical resection of the pituitary adenoma, the tumor responsible for excessive growth hormone production, is another crucial treatment modality.
The success of surgery depends on the tumor’s size, location, and the surgeon’s expertise. In cases where medical therapy and surgery are insufficient, or not suitable, pegvisomant, a growth hormone receptor antagonist, may be considered. This medication blocks the growth hormone receptor, preventing the hormone from binding and exerting its effects.
Managing Hypertension and Other Risk Factors
Hypertension, a common comorbidity in acromegaly, significantly increases the risk of heart failure. Effective blood pressure control is paramount in reducing cardiovascular strain. Aggressive management of other risk factors, such as dyslipidemia (abnormal blood fat levels) and diabetes, is also critical. Controlling these factors can significantly reduce the likelihood of developing or worsening heart failure. Lifestyle modifications play a crucial role in achieving and maintaining these goals.
Lifestyle Modifications
A healthy lifestyle is essential for optimizing cardiovascular health in acromegaly. This includes adopting a balanced diet rich in fruits, vegetables, and whole grains, while limiting processed foods, saturated fats, and excessive sugar intake. Regular physical activity, such as brisk walking, swimming, or cycling, is recommended. Maintaining a healthy weight through dietary adjustments and exercise is vital in reducing cardiovascular strain.
Quitting smoking and limiting alcohol consumption are also crucial steps in improving overall health.
Regular Follow-up Care and Monitoring
Regular monitoring of cardiac function is essential in managing acromegaly-related heart failure. This includes regular echocardiograms, electrocardiograms (ECGs), and blood pressure measurements to assess cardiac structure and function, and to detect any signs of deterioration. Close monitoring of blood glucose levels and lipid profiles is also essential for preventing further cardiovascular complications. Frequent follow-up appointments allow healthcare providers to adapt treatment plans and address any emerging issues promptly.
Treatment Options for Acromegaly and Heart Failure
| Treatment Option | Description | Potential Side Effects |
|---|---|---|
| Somatostatin Analogs (e.g., octreotide, lanreotide) | Suppress growth hormone secretion | Nausea, diarrhea, abdominal pain, gallstones, and in some cases, elevated liver enzymes |
| Surgical Resection | Removal of pituitary adenoma | Risk of cerebrospinal fluid leak, pituitary insufficiency, and visual field defects |
| Pegvisomant | Growth hormone receptor antagonist | Injection site reactions, liver enzyme abnormalities, and in rare cases, allergic reactions |
| Lifestyle Modifications | Balanced diet, exercise, weight management | Requires patient commitment and motivation; no direct side effects |
| Blood Pressure Medications | Control hypertension | Various, depending on the specific medication; common side effects include dizziness, fatigue, and headache. |
| Cardiac Medications (as needed) | Manage heart failure symptoms | Depending on the specific medication, potential side effects may include nausea, dizziness, and increased heart rate. |
Prognosis and Long-Term Outcomes
The journey of managing acromegaly and the accompanying heart failure is a long-term commitment. Understanding the prognosis and potential outcomes is crucial for patients and healthcare providers alike. This involves anticipating the likely course of the disease, recognizing factors that might influence its severity, and exploring strategies for improving long-term well-being. Ultimately, the goal is to empower individuals with a clear picture of what to expect and how to navigate this complex health challenge.
Factors Influencing Severity and Progression
Several factors can significantly influence the severity and progression of heart failure in individuals with acromegaly. These factors include the duration and severity of acromegaly itself, the effectiveness of treatment in controlling excessive growth hormone levels, and the presence of other co-morbidities. For example, uncontrolled acromegaly leads to significant cardiac structural changes, predisposing the heart to dysfunction and failure.
Similarly, the presence of hypertension, diabetes, or sleep apnea can exacerbate the strain on the cardiovascular system, compounding the risk of heart failure progression.
Potential for Improving Outcomes
Early diagnosis and effective treatment play a pivotal role in improving outcomes for individuals with both acromegaly and heart failure. Prompt diagnosis of acromegaly, ideally before significant cardiac changes occur, allows for timely intervention and treatment with growth hormone-lowering therapies. Furthermore, meticulous management of co-morbidities, such as hypertension and diabetes, is essential to mitigate the cardiovascular risks associated with acromegaly.
A multidisciplinary approach, involving endocrinologists, cardiologists, and other specialists, is often necessary to provide comprehensive care and maximize treatment efficacy.
Preventative Strategies
Proactive measures can significantly reduce the risk of heart failure complications in individuals with acromegaly. These strategies include diligent adherence to prescribed medications, regular cardiovascular monitoring, and lifestyle modifications. Maintaining a healthy diet, engaging in regular exercise, and controlling blood pressure and blood sugar levels are critical in reducing the strain on the heart. Furthermore, early detection and management of any co-morbidities are crucial to minimizing the risk of exacerbating heart failure.
Summary of Key Factors Influencing Prognosis
| Factor | Description | Impact on Prognosis |
|---|---|---|
| Duration and Severity of Acromegaly | The length of time acromegaly has been present and the extent of its impact on the body. | Longer duration and greater severity correlate with increased risk of cardiac complications and poorer prognosis. |
| Effectiveness of Treatment | How well growth hormone levels are controlled by treatment. | Adequate control of growth hormone levels is crucial in mitigating cardiac damage and improving prognosis. |
| Presence of Co-morbidities | The existence of other medical conditions, such as hypertension, diabetes, or sleep apnea. | Co-morbidities can exacerbate the strain on the heart and negatively impact the prognosis. |
| Adherence to Treatment | The patient’s commitment to following prescribed medications and lifestyle recommendations. | Adherence to treatment is vital for maintaining controlled hormone levels and managing co-morbidities, thereby improving the long-term outlook. |
| Early Diagnosis | Prompt identification of acromegaly before significant cardiac changes occur. | Early diagnosis allows for timely intervention, minimizing the risk of irreversible heart damage and improving long-term outcomes. |
Case Studies and Illustrative Examples
Understanding acromegaly and its impact on heart failure requires examining real-world cases. These examples illuminate the diagnostic challenges, treatment strategies, and long-term outcomes associated with this complex interplay. The following case studies showcase the varied presentations and highlight crucial factors for effective management.
Hypothetical Case Study: Diagnostic Process and Management
A 45-year-old female presented with progressively worsening headaches, excessive sweating, and enlarged hands and feet. She also reported increasing fatigue and shortness of breath on exertion. Physical examination revealed characteristic features of acromegaly, including enlarged facial features and thickened skin. Blood tests showed elevated growth hormone levels, confirming the diagnosis. Further investigations, including an MRI of the pituitary gland, revealed a pituitary adenoma, the source of excessive growth hormone production.
Treatment involved surgical removal of the tumor, followed by medication to control growth hormone levels. Regular cardiac assessments, including echocardiograms and stress tests, were implemented to monitor the impact of acromegaly on heart structure and function. The patient’s symptoms gradually improved, and cardiac function stabilized with ongoing management.
Case Study Focusing on Impact of Treatment on Cardiac Function, Acromegaly and heart failure
A 62-year-old male with acromegaly and heart failure experienced significant improvement in cardiac function after undergoing pituitary surgery and subsequent medical therapy. Pre-treatment echocardiography demonstrated left ventricular hypertrophy and diastolic dysfunction. Post-treatment assessments showed a reduction in left ventricular mass index and improved diastolic filling, reflecting the positive impact of controlling excessive growth hormone. This case illustrates the crucial link between controlling acromegaly and improving cardiac health.
Continued monitoring of cardiac function and lifestyle adjustments were essential components of the management plan.
Illustration of Acromegaly’s Impact on Heart Structure and Function
Acromegaly significantly affects the heart’s structure and function. The chronic elevation of growth hormone leads to cardiac hypertrophy, particularly left ventricular hypertrophy, a thickening of the heart muscle. This thickened muscle can impair the heart’s ability to relax and fill with blood during diastole, resulting in diastolic dysfunction. Furthermore, acromegaly can increase the risk of hypertension, contributing to further strain on the heart.
Over time, these factors can lead to heart failure. The impact varies from patient to patient, and the severity depends on the duration and degree of growth hormone excess.
Impact of Lifestyle Interventions on Heart Health
Lifestyle modifications play a vital role in mitigating the cardiovascular complications of acromegaly. A patient with acromegaly and heart failure might benefit from a structured exercise program, emphasizing low-impact activities such as walking, swimming, or cycling. This improves overall cardiovascular health, reduces blood pressure, and helps maintain a healthy weight. Dietary changes, such as reducing saturated and trans fats, controlling sodium intake, and increasing fruits and vegetables, can also improve cardiovascular health.
Smoking cessation and stress management techniques further contribute to overall cardiovascular well-being.
Case Example Demonstrating the Importance of Early Intervention
A 38-year-old female experiencing symptoms like headaches, sweating, and enlarged hands initially dismissed them as normal aging. However, persistent symptoms prompted further evaluation, leading to a diagnosis of acromegaly. Early intervention, including surgical removal of the pituitary tumor and growth hormone suppression therapy, prevented further progression of cardiac complications. This case underscores the significance of recognizing and addressing the early signs of acromegaly to minimize the risk of long-term cardiovascular damage.
Prompt medical attention is crucial to effectively manage acromegaly and prevent or delay the onset of heart failure.
Last Recap: Acromegaly And Heart Failure
In conclusion, acromegaly and heart failure represent a significant clinical challenge requiring a multi-faceted approach to diagnosis and management. Early detection and targeted interventions are crucial to mitigating the progression of heart failure in patients with acromegaly. The intricate interplay between hormonal imbalances, cardiovascular effects, and lifestyle factors underscores the importance of personalized treatment plans. This deep dive into acromegaly and heart failure provides a crucial framework for understanding and addressing this complex health concern.
