Almost 20 percent of people with MS are misdiagnosed at first, setting the stage for a crucial discussion about the complexities of diagnosing this often-misunderstood disease. This isn’t just a statistic; it represents countless individuals who’ve endured delays in diagnosis, potentially impacting their treatment, quality of life, and even long-term health outcomes. Understanding the reasons behind these misdiagnoses and the strategies for improvement is essential for better patient care.
Multiple sclerosis (MS) is a chronic autoimmune disease that affects the central nervous system. Common symptoms include vision problems, numbness, muscle weakness, and balance issues. Diagnosing MS can be challenging due to the varied presentation of symptoms and the overlap with other neurological conditions. Various diagnostic methods, such as MRI scans and neurological examinations, are employed, but accurate diagnosis often requires careful consideration of patient history, physical examination, and exclusion of other potential causes.
Introduction to Multiple Sclerosis (MS) Misdiagnosis
Multiple Sclerosis (MS) is a chronic autoimmune disease affecting the central nervous system, including the brain, spinal cord, and optic nerves. It disrupts the flow of information between these parts of the body, leading to a wide range of symptoms that can vary significantly in severity and presentation. Understanding the complexities of MS diagnosis is crucial, as early and accurate diagnosis allows for timely intervention and management of the disease.
Unfortunately, a significant portion of MS cases are initially misdiagnosed, often delaying appropriate treatment.The diagnostic journey for MS can be challenging due to the diverse and often subtle symptoms. These symptoms can mimic those of other neurological conditions, leading to confusion and delays in accurate diagnosis. This makes it imperative to understand the typical symptoms of MS, the diagnostic process, and the potential for misdiagnosis.
Awareness of these aspects is vital for both patients and healthcare professionals.
Common Symptoms of Multiple Sclerosis
MS symptoms are diverse and can vary significantly between individuals. Some of the most prevalent symptoms include: visual disturbances (like blurry vision or optic neuritis), numbness or tingling in the extremities, muscle weakness or spasms, fatigue, balance problems, cognitive difficulties, and pain. These symptoms can appear intermittently and in different combinations, making accurate diagnosis challenging.
Diagnostic Methods for Multiple Sclerosis
Diagnosing MS requires a multi-faceted approach. Clinicians rely on a combination of methods, including: a thorough medical history, neurological examination, and various diagnostic tests. A detailed patient history helps identify patterns and potential triggers. A neurological examination assesses motor skills, sensory function, and reflexes to pinpoint affected areas.
Diagnostic Challenges and Potential Misdiagnosis
Diagnosing MS can be complicated because its symptoms can mimic those of other neurological conditions. The symptoms often fluctuate, and their presentation can vary greatly from person to person. Early symptoms might be subtle and easily overlooked, leading to delays in diagnosis. The lack of a single definitive test for MS further complicates the process. This necessitates a thorough evaluation and consideration of alternative diagnoses.
Comparing Symptoms of MS with Other Conditions
| Condition | Symptoms | Key Differences |
|---|---|---|
| Multiple Sclerosis (MS) | Visual disturbances, numbness/tingling, muscle weakness, fatigue, balance problems, cognitive difficulties, pain | Symptoms can be intermittent and vary widely. Neurological examination is crucial. |
| Amyotrophic Lateral Sclerosis (ALS) | Progressive muscle weakness and atrophy, difficulty speaking, swallowing, and breathing | ALS typically involves progressive muscle weakness, whereas MS can have a more fluctuating course. |
| Stroke | Sudden onset of neurological deficits like weakness, numbness, speech problems, vision loss | Stroke typically has a sudden onset, while MS symptoms often develop gradually. |
| Brain Tumor | Headaches, seizures, cognitive changes, vision problems | Brain tumors may cause more focal neurological deficits, while MS symptoms can be more diffuse. |
| Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) | Progressive weakness and numbness in the limbs, often starting in the distal extremities | CIDP typically affects peripheral nerves, while MS affects the central nervous system. |
This table provides a basic comparison; it is crucial to consult with a healthcare professional for accurate diagnosis.
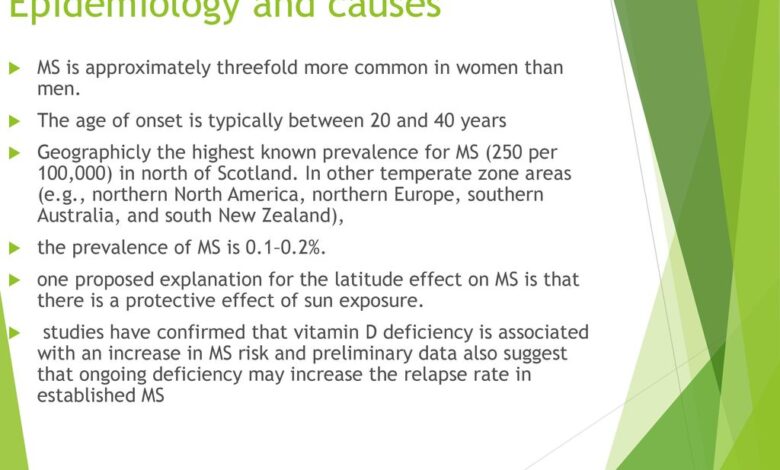
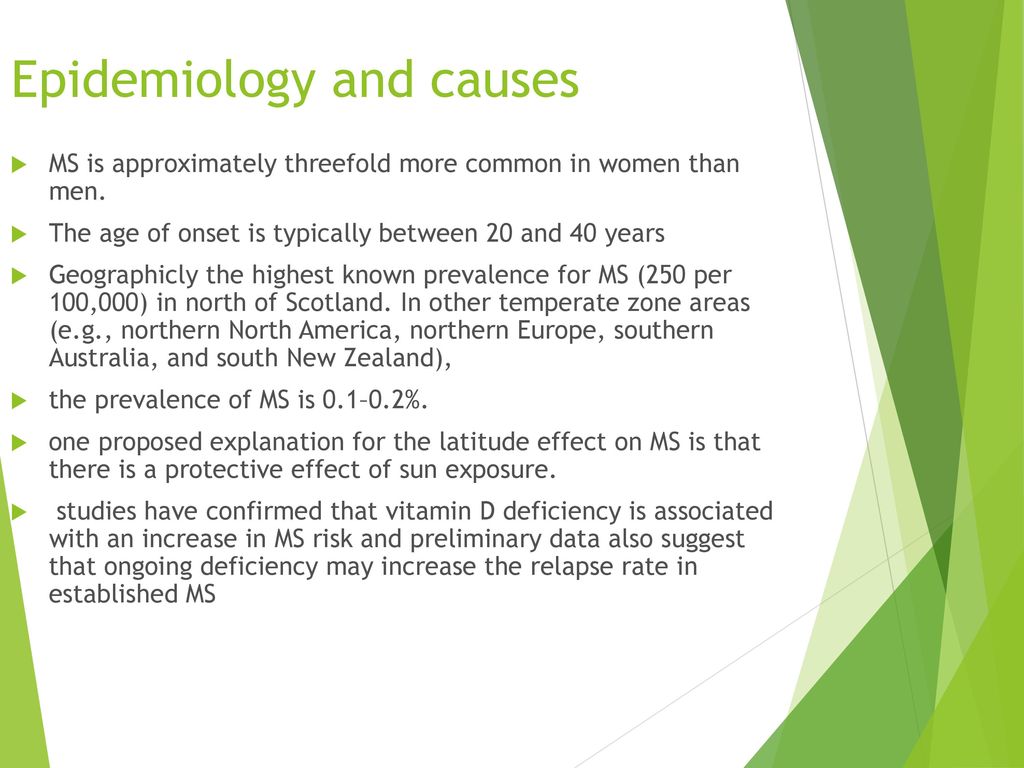
Prevalence and Impact of Misdiagnosis
The initial diagnosis of Multiple Sclerosis (MS) is often a complex and challenging journey. While advancements in diagnostic techniques have improved, a significant percentage of individuals initially receive an incorrect diagnosis, delaying appropriate treatment and impacting their quality of life. This is a critical issue that needs thorough understanding to support those affected.The statistic “almost 20 percent of people with MS are misdiagnosed at first” highlights the substantial problem of misidentification in the early stages of MS.
This high rate of misdiagnosis underscores the need for improved diagnostic criteria and greater awareness among healthcare professionals. It also emphasizes the importance of patient advocacy and the crucial role of self-education in navigating this complex medical landscape.
Statistical Data on Misdiagnosis
The time it takes to receive an accurate MS diagnosis varies considerably. Factors such as symptom presentation, access to specialized care, and the individual’s specific health history all play a role in the diagnostic process. Studies suggest that, on average, the time from initial symptom onset to an accurate diagnosis can range from several months to several years.
This delay in accurate diagnosis often results in missed opportunities for early intervention, leading to potentially irreversible damage to the central nervous system.
Consequences of Delayed or Incorrect Diagnoses
Delayed or incorrect MS diagnoses can have severe consequences for individuals. These include the progressive worsening of neurological symptoms, potentially leading to permanent disability. Moreover, delayed treatment can significantly reduce the effectiveness of disease-modifying therapies, impacting the long-term health and well-being of those affected. The uncertainty and anxiety associated with misdiagnosis can also take a toll on an individual’s mental health, leading to significant emotional distress.
Emotional and Financial Burdens
Misdiagnosis often places a significant emotional and financial burden on individuals. The prolonged period of uncertainty, misinterpretations of symptoms, and the need for multiple consultations and tests can be emotionally draining. The financial implications can be substantial, particularly when associated with unnecessary medical procedures, therapies, and lost time from work. These factors contribute to the overall negative impact of misdiagnosis on an individual’s quality of life.
Timeline of Diagnosis
| Factor | Description | Typical Timeline (Months/Years) |
|---|---|---|
| Symptom Severity | Mild, intermittent symptoms | 12-24 months |
| Symptom Severity | Rapidly progressing, severe symptoms | 6-12 months |
| Access to Healthcare | Limited access to neurologists or specialized MS centers | 24-36 months |
| Access to Healthcare | Immediate access to neurologists or MS specialists | 6-12 months |
| Patient Activeness | Proactive in seeking second opinions or additional testing | 6-12 months |
| Patient Activeness | Reliant on general practitioners for initial care | 12-24 months |
This table illustrates the wide range of timeframes involved in receiving an accurate MS diagnosis. It highlights the importance of factors like symptom severity, access to appropriate medical care, and the patient’s active role in the diagnostic process.
Reasons Behind Misdiagnosis

Misdiagnosis of multiple sclerosis (MS) is a significant concern, impacting patient care and well-being. Understanding the factors contributing to these errors is crucial for improving diagnostic accuracy and reducing the time it takes to receive an appropriate diagnosis. This necessitates a comprehensive approach, involving both a review of common reasons for misdiagnosis and an exploration of the challenges faced by healthcare professionals.The complexity of MS, characterized by its varied presentation and potential overlap with other neurological conditions, makes accurate diagnosis a considerable challenge.
Furthermore, the initial symptoms of MS can be subtle and non-specific, leading to delayed or misdirected investigations.
Common Reasons for Misdiagnosis
Numerous factors contribute to the misdiagnosis of MS. These factors often stem from the multifaceted nature of the disease and the possibility of its symptoms mimicking those of other neurological conditions. Similarities in symptoms between MS and other neurological disorders can lead to incorrect diagnoses, delaying or preventing the appropriate treatment for MS.
- Symptom overlap with other neurological conditions: MS symptoms can closely resemble those of conditions like stroke, brain tumors, or spinal cord injuries. For instance, both MS and stroke can cause weakness, numbness, and vision problems. Early diagnosis can be hampered by this overlap, as distinguishing the underlying cause can be complex.
- Initial symptoms being subtle and non-specific: Early MS symptoms can be mild and nonspecific, such as fatigue, dizziness, or mild vision problems. These subtle manifestations might not raise immediate suspicion for MS, potentially delaying appropriate investigations.
- Lack of standardized diagnostic criteria across healthcare settings: Variations in diagnostic criteria and procedures between different healthcare settings can lead to inconsistent diagnoses. This variability underscores the need for a more uniform approach to diagnosis.
- Subjectivity in symptom reporting and interpretation: Patient experiences and reporting of symptoms can be subjective. This subjectivity can affect the accuracy of diagnoses, particularly in cases where symptoms are not easily quantifiable.
- Limited availability of advanced diagnostic tools in certain regions: Access to sophisticated diagnostic tools, like MRI scans, may be restricted in certain regions, further hindering accurate diagnosis in those areas.
Challenges Faced by Healthcare Professionals
Healthcare professionals face numerous challenges in accurately diagnosing MS. These difficulties stem from the complex nature of the disease and the need for specialized knowledge and experience.
- Variability in symptom presentation: MS symptoms vary considerably from person to person, and even within the same individual over time. This variability poses a challenge for healthcare providers in identifying consistent patterns and making accurate diagnoses.
- Lack of specific diagnostic tests: There isn’t a single definitive test for MS. Diagnoses rely on a combination of clinical evaluations, symptom history, and various investigations. The lack of a single test makes accurate diagnosis more challenging.
- Timely access to specialist expertise: Access to neurologists specializing in MS diagnosis can be limited, leading to delays in diagnosis and appropriate management.
Role of Symptom Variability in MS Diagnosis
Symptom variability significantly complicates MS diagnosis. The diverse range of symptoms experienced by individuals with MS can overlap with other conditions, leading to misdiagnosis.
- Symptoms vary in severity and frequency: Symptoms of MS can range from mild to severe and fluctuate in frequency. This fluctuating nature of symptoms can make it challenging to establish a consistent pattern indicative of MS.
- Symptoms can be intermittent: Symptoms of MS may come and go, making it difficult to identify a pattern or link symptoms to a specific underlying cause.
Diagnostic Processes in Different Healthcare Settings
Diagnostic processes for MS can vary significantly depending on the healthcare setting. This variability underscores the importance of a standardized approach to improve consistency and accuracy.
- Variations in diagnostic criteria and procedures: Diagnostic criteria and procedures used in different healthcare settings might differ, leading to inconsistencies in diagnosis. This highlights the need for a unified set of guidelines for the diagnosis of MS.
- Variations in access to diagnostic tools: The availability and accessibility of diagnostic tools, such as MRI scans, can vary between healthcare settings, potentially impacting the accuracy of diagnoses.
Importance of Patient History and Physical Examination
A thorough patient history and physical examination remain crucial elements in the diagnostic process. This process is essential for building a comprehensive understanding of the patient’s condition and potential underlying causes.
- Gathering detailed patient history: A detailed history, including symptom onset, progression, and any associated factors, can provide vital clues for accurate diagnosis.
- Performing a comprehensive physical examination: A thorough neurological examination is essential for identifying potential neurological deficits and physical manifestations of the disease.
Diagnostic Criteria for MS
Different sets of criteria have been used to diagnose MS over time, reflecting the evolution of understanding of the disease.
| Criteria | Description | Time Period |
|---|---|---|
| 1983 McDonald Criteria | Initially relied heavily on clinical presentation and neurological examination. | 1983 |
| 2001 McDonald Criteria | Introduced the use of MRI findings in the diagnostic process, increasing diagnostic accuracy. | 2001 |
| 2017 McDonald Criteria | Further refined the diagnostic criteria, emphasizing the importance of magnetic resonance imaging (MRI) and clinical presentation for diagnosis. | 2017 |
Impact on Patient Outcomes: Almost 20 Percent Of People With Ms Are Misdiagnosed At First
Misdiagnosis of Multiple Sclerosis (MS) significantly impacts patient outcomes, often leading to delayed treatment and a diminished quality of life. The consequences of misdiagnosis can extend beyond the immediate period of incorrect labeling, potentially altering the course of the disease and creating long-term complications. Understanding these impacts is crucial for raising awareness and improving diagnostic accuracy.The initial misdiagnosis can create a cascade of negative effects, from missed opportunities for early intervention to the emotional toll of navigating an uncertain medical landscape.
It’s pretty shocking that almost 20 percent of people with MS are initially misdiagnosed. This highlights the complexity of diagnosing neurological conditions. Similar to the challenges in recognizing symptoms, sometimes depression can mimic other illnesses, even following a heart attack, as seen in depression after heart attack. This further emphasizes the importance of thorough evaluations and a careful consideration of potential co-occurring conditions when dealing with seemingly isolated symptoms like those often seen in early MS diagnoses.
The time spent searching for a correct diagnosis is often a period of confusion, anxiety, and frustration for patients and their families. This delay in diagnosis can directly affect the effectiveness of treatment and the long-term management of MS.
Treatment Delays and Quality of Life
Misdiagnosis frequently results in delays in appropriate MS treatment. This delay can significantly impact the effectiveness of disease-modifying therapies (DMTs), often leading to more severe disease progression. A timely diagnosis allows for prompt initiation of DMTs, which can slow the progression of the disease and potentially reduce the frequency and severity of relapses. However, when diagnosis is delayed, the damage caused by the disease may already be significant, making it harder to halt the progression.
The psychological impact of a misdiagnosis, including the uncertainty, stress, and frustration, can also significantly affect a patient’s quality of life.
It’s truly frustrating that almost 20 percent of people with MS are initially misdiagnosed. Navigating the complexities of medical diagnoses can be incredibly challenging, especially when dealing with something as serious as MS. Fortunately, there are resources available to help manage the pain relief during labor, such as pain relief during labor , which can provide significant support during a difficult time.
However, this highlights the importance of proper diagnoses, as accurate identification of MS is crucial for effective treatment and management, impacting the quality of life for so many.
Impact on Disease Progression
Misdiagnosis can significantly affect the course of MS. For example, a patient initially diagnosed with another condition, such as fibromyalgia or chronic fatigue syndrome, may experience worsening neurological symptoms over time that could be attributed to MS, only to be recognized later. The delay in appropriate treatment can allow the disease to progress, leading to more extensive nerve damage and the development of disability.
Early intervention, often made possible by a timely and accurate diagnosis, can be instrumental in slowing disease progression and improving long-term outcomes.
Timely and Accurate Diagnosis’ Impact on Treatment Efficacy
A timely and accurate diagnosis is critical for effective treatment. Disease-modifying therapies (DMTs) work best when administered early in the disease process. Delayed diagnosis can reduce the effectiveness of these therapies, making it harder to control the progression of the disease. Early intervention and treatment, guided by an accurate diagnosis, can halt or slow the disease progression and improve the overall quality of life for patients.
Potential for Long-Term Complications
Delayed diagnosis of MS can lead to a variety of long-term complications. Patients who are misdiagnosed may experience more severe neurological symptoms, permanent nerve damage, and increased disability. The cumulative effects of the disease over time can result in a more profound impact on their daily lives. Early and accurate diagnosis can significantly reduce the likelihood of these severe outcomes.
Need for Increased Awareness and Improved Diagnostic Tools
Increased awareness among healthcare professionals and the public about the signs and symptoms of MS is crucial for early detection and diagnosis. Improved diagnostic tools, such as more sophisticated imaging techniques and blood tests, can enhance the accuracy of diagnosis and reduce the time it takes to reach a correct diagnosis. The development and accessibility of such tools can greatly contribute to better patient outcomes.
Comparison of Patient Experiences: Accurate vs. Delayed MS Diagnosis, Almost 20 percent of people with ms are misdiagnosed at first
| Feature | Accurate MS Diagnosis | Delayed MS Diagnosis |
|---|---|---|
| Treatment Initiation | Prompt initiation of disease-modifying therapies (DMTs). | Delayed or inappropriate treatment, potentially missing optimal treatment windows. |
| Disease Progression | Potentially slower disease progression and reduced severity of symptoms. | More rapid disease progression, leading to more significant disability. |
| Quality of Life | Improved quality of life due to timely and effective management. | Reduced quality of life due to delayed diagnosis and management. |
| Emotional Impact | Relief and reassurance from a definitive diagnosis. | Uncertainty, anxiety, and frustration associated with the diagnostic journey. |
Strategies for Improving Diagnosis
Reducing the frequency of misdiagnosis in Multiple Sclerosis (MS) requires a multifaceted approach. Current diagnostic methods, while improving, still suffer from limitations, leading to delays in accurate diagnoses and impacting patient outcomes. Improving diagnostic accuracy is crucial for timely intervention, reducing disease progression, and enhancing quality of life for those affected.The cornerstone of better MS diagnosis lies in a comprehensive understanding of the disease’s diverse presentation, recognizing that symptoms can manifest in various ways and mimic other neurological conditions.
This requires not only advanced diagnostic tools but also a refined clinical judgment process, which includes careful consideration of patient history, physical examination findings, and appropriate diagnostic testing.
Improving Early Detection of MS
Early detection of MS is vital for initiating treatment as early as possible, potentially slowing disease progression and preventing long-term disability. This necessitates a proactive approach to identifying individuals at risk, particularly those presenting with subtle or atypical symptoms. Developing more sensitive diagnostic markers, such as blood tests or advanced imaging techniques, is crucial in enhancing the speed and accuracy of diagnosis.
The integration of these advancements with experienced clinicians will provide a more efficient pathway for detecting MS in its early stages.
Enhanced Diagnostic Protocols
Refined diagnostic protocols are critical to minimize misdiagnosis. These protocols should incorporate a standardized approach to evaluating patients, ensuring consistency in the assessment process. They should also incorporate the latest advancements in neuroimaging techniques, such as MRI, to identify characteristic lesions in the central nervous system. Furthermore, these protocols should incorporate a standardized assessment of patient history and neurological examination to ensure that all relevant information is considered during the diagnostic process.
Educational Resources for Healthcare Professionals
Comprehensive educational resources for healthcare professionals play a critical role in improving the diagnostic accuracy of MS. Continuous medical education programs should focus on the latest diagnostic criteria, diagnostic imaging techniques, and differential diagnoses that can mimic MS. These resources should emphasize the importance of recognizing subtle symptoms and incorporating patient history into the diagnostic process. Online platforms, webinars, and workshops can facilitate dissemination of this information to a broader audience of healthcare providers.
It’s shocking that almost 20 percent of people with MS are initially misdiagnosed. This highlights the complexities of diagnosing neurological conditions. While exploring the reasons behind these misdiagnoses, it’s worth considering how lifestyle choices, such as the diets associated with increased risk of heart disease, the diets associated with increased risk of heart disease , might sometimes be contributing factors, indirectly affecting neurological health.
Ultimately, accurate and timely diagnosis remains crucial for effective treatment and management of MS.
Comparison of Diagnostic Approaches for MS
Different diagnostic approaches for MS offer varying degrees of sensitivity and specificity. Clinical evaluation, often the first step, relies on the clinician’s experience in recognizing suggestive symptoms. Neuroimaging techniques, such as MRI, provide visual confirmation of lesions in the central nervous system. Neurophysiological tests, like evoked potentials, can assess nerve conduction and aid in the differential diagnosis.
Each approach has strengths and weaknesses; combining these methods in a structured protocol can significantly enhance the diagnostic process.
Suggested Improvements to the Diagnostic Process
| Category | Improvement Suggestion | Rationale |
|---|---|---|
| Pre-diagnostic | Implement a standardized patient questionnaire to collect detailed symptom history, including duration, frequency, and location. | Comprehensive symptom collection improves accuracy and aids in ruling out other conditions. |
| Pre-diagnostic | Encourage patients to maintain detailed symptom diaries. | Provides a comprehensive record of symptoms for clinicians to analyze, which aids in diagnosis. |
| Diagnostic | Incorporate a multidisciplinary approach to diagnosis, involving neurologists, neuropsychologists, and other specialists. | Provides a more holistic assessment, which can reduce misdiagnosis. |
| Diagnostic | Implement a standardized MRI protocol for MS diagnosis, including specific sequences and criteria for lesion identification. | Standardization ensures consistent and accurate lesion identification. |
| Post-diagnostic | Establish clear communication channels for sharing diagnostic findings and treatment plans between healthcare professionals. | Reduces ambiguity and improves patient care coordination. |
| Post-diagnostic | Provide patients with comprehensive information regarding their diagnosis, treatment options, and prognosis. | Empowers patients to actively participate in their care and reduces anxiety. |
Illustrative Case Studies (Hypothetical)
Misdiagnosis in Multiple Sclerosis (MS) can significantly impact a patient’s life, delaying appropriate treatment and potentially causing further complications. Understanding the potential diagnostic journeys of individuals facing misdiagnosis can shed light on the challenges and highlight the importance of patient advocacy. These hypothetical cases illustrate common symptoms and diagnostic difficulties encountered by those with MS.
Case Study 1: The Initially Misinterpreted Fatigue
This hypothetical case focuses on a young adult, Sarah, experiencing increasing fatigue, often accompanied by dizziness and vision problems. Initially, her symptoms were attributed to stress and lack of sleep by healthcare providers. The symptoms worsened over several months, and Sarah’s quality of life significantly declined. She sought multiple opinions but faced skepticism about the possibility of MS.
She persisted, researching MS symptoms and advocating for further testing. Ultimately, MRI scans revealed characteristic lesions indicative of MS, and a neurologist confirmed the diagnosis. This case highlights the importance of patient persistence and the potential for initial symptoms to be dismissed or misattributed.
Case Study 2: The Mimicking Pain
John, a middle-aged man, experienced persistent pain in his legs, initially thought to be due to arthritis. The pain was intermittent and accompanied by numbness and tingling. His primary care physician prescribed pain relievers, which provided only temporary relief. John’s condition progressively worsened, and he struggled with mobility. His relentless pursuit of a proper diagnosis, fueled by his own research and advocacy, led him to a neurologist who recognized the pattern of symptoms.
A neurological examination and subsequent MRI confirmed the diagnosis of MS. This example underscores the need for comprehensive neurological evaluations, even when initial diagnoses seem plausible.
Case Study 3: The Masked Vision Changes
Emily, a young professional, started experiencing blurred vision in one eye. Her initial tests were inconclusive. She was diagnosed with a common eye condition. However, Emily continued to experience worsening vision problems, including double vision and optic neuritis. She sought second opinions and tirelessly advocated for more detailed investigations.
Her persistence ultimately led to an MRI revealing characteristic lesions, confirming the diagnosis of MS. This scenario illustrates the potential for symptoms of MS to be masked or misattributed to other conditions, emphasizing the importance of comprehensive evaluations and patient advocacy.
Summary Table of Case Studies
| Case Study | Symptoms | Diagnostic Tests | Final Diagnosis |
|---|---|---|---|
| Sarah (Fatigue) | Increasing fatigue, dizziness, vision problems | Comprehensive history, physical exam, MRI | Multiple Sclerosis |
| John (Pain) | Persistent leg pain, numbness, tingling | Physical exam, neurological examination, MRI | Multiple Sclerosis |
| Emily (Vision) | Blurred vision, double vision, optic neuritis | Eye exams, neurological examination, MRI | Multiple Sclerosis |
Public Awareness Campaigns
Misdiagnosis is a significant hurdle in the MS journey, impacting not only the patient’s health but also their quality of life and ability to access timely treatment. Public awareness campaigns are crucial to combat this issue. Educating the public about MS, its symptoms, and the potential for misdiagnosis can lead to earlier diagnoses and better outcomes. Understanding the nuances of this disease and the complexities of its early presentation is essential for everyone.Raising awareness about MS misdiagnosis is vital because it empowers individuals to recognize potential symptoms and encourages them to seek medical attention promptly.
This proactive approach can significantly improve the chances of an accurate diagnosis and initiate appropriate treatment. By fostering a better understanding of MS among the general public, we can create a supportive environment for those living with the condition.
Need for Public Awareness Campaigns
Public awareness campaigns are essential to address the high prevalence of MS misdiagnosis. Early diagnosis is critical for managing MS effectively, and public awareness campaigns play a key role in educating the public about the disease and its early symptoms. This understanding can empower individuals to seek medical attention sooner, leading to quicker diagnoses and better treatment outcomes.
Effective Public Awareness Strategies
Several strategies can make public awareness campaigns impactful. Utilizing diverse media platforms, such as social media, television, radio, and print, can broaden the reach of the campaign. Partnerships with healthcare professionals and organizations specializing in MS can enhance credibility and provide accurate information. Interactive events, such as awareness walks and educational seminars, can engage the public directly and promote a sense of community.
Visual aids and storytelling are powerful tools to help convey complex information in a relatable and engaging way.
Hypothetical Public Awareness Campaign Plan
A hypothetical public awareness campaign focusing on MS misdiagnosis could include a multi-pronged approach. Initial phases would concentrate on educating healthcare professionals through workshops and educational materials. Subsequently, a comprehensive public awareness campaign would involve targeted advertising on social media, online platforms, and in local communities. This campaign would highlight the common symptoms of MS and encourage individuals to seek prompt medical attention if they experience them.
Creating a series of easily accessible resources, including educational videos and infographics, would further assist the public in understanding the complexities of the disease. A crucial aspect would be collaboration with patient advocacy groups to ensure the message resonates with the community and is accurate.
Role of Patient Advocacy Groups
Patient advocacy groups play a vital role in public awareness campaigns. Their firsthand experience and understanding of the disease make them valuable partners. These groups can offer testimonials, provide support to individuals experiencing misdiagnosis, and help ensure the accuracy of information disseminated through the campaign. They are often deeply involved in community outreach programs, workshops, and events, providing vital support to those affected.
Furthermore, their networks within the medical community facilitate connections with healthcare professionals and foster a better understanding of MS among practitioners.
Social Media for Public Education
Social media platforms are powerful tools for educating the public about MS and its misdiagnosis. They allow for targeted outreach, real-time engagement, and a more interactive learning experience. Creating engaging content, such as informative videos, infographics, and personal stories, can increase public awareness and encourage discussions. Regular posts and updates can keep the topic relevant and attract attention.
Using hashtags related to MS and misdiagnosis can help people discover and share the content more effectively.
Potential Social Media Posts
| Post Type | Content Example |
|---|---|
| Awareness Post | “Did you know that MS can present in various ways, sometimes mimicking other conditions? Early diagnosis is key! #MSAwareness #MSMisdiagnosis” |
| Informational Post | “Common early symptoms of MS include vision problems, numbness, and fatigue. Don’t ignore these! Learn more at [link to website]. #MSSymptoms #EarlyDiagnosis” |
| Testimonial Post | “I experienced a significant delay in my diagnosis. Early awareness saved me from years of unnecessary suffering. Please share this to help others. #MSJourney #MisdiagnosisStories” |
| Interactive Post | “What are your thoughts on early MS symptoms? Share your experiences in the comments below. #MSDiscussion #MSCommunity” |
| Educational Post | “Infographic: Understanding the difference between MS symptoms and other conditions. Share this with your network. #MSFacts #MSEducation” |
Final Thoughts
The alarming statistic of almost 20 percent misdiagnosis highlights the urgent need for improved diagnostic protocols, increased awareness, and better education for healthcare professionals. By examining the reasons behind misdiagnosis, implementing strategies for earlier detection, and empowering patients to advocate for themselves, we can move toward a future where MS diagnoses are more accurate and timely, ultimately leading to better patient outcomes.
The hypothetical case studies illustrate the real-life impact of misdiagnosis, while the public awareness campaign Artikels actionable steps to create a more informed and supportive environment for those living with MS.