Are older adults getting too many cancer screenings? This complex question delves into the evolving guidelines for cancer screening in seniors, weighing the potential benefits against the risks and considering individual needs. Current recommendations often differ significantly from those for younger adults, prompting crucial discussions about personalized strategies and resource allocation.
The frequency and types of cancer screenings recommended for older adults have changed dramatically over time. Factors like individual health conditions, lifestyle, and life expectancy are crucial to consider when determining the appropriate screening strategy. This comprehensive exploration will examine the guidelines, potential benefits and harms, and the personalized considerations required for optimal care.
Screening Frequency and Guidelines
Navigating the world of cancer screenings can be daunting, especially as we age. Understanding the recommended frequency and the rationale behind these guidelines is crucial for making informed decisions about your health. This section delves into the evolving landscape of cancer screening for older adults, comparing it to recommendations for younger individuals.Current guidelines for cancer screenings are not static; they evolve based on the latest research and advancements in medical knowledge.
These guidelines aim to balance the potential benefits of early detection with the risks and potential harms of frequent testing. The decision to undergo a screening often involves a discussion with your doctor, taking into account your individual medical history, family history, and overall health status.
Current Cancer Screening Guidelines
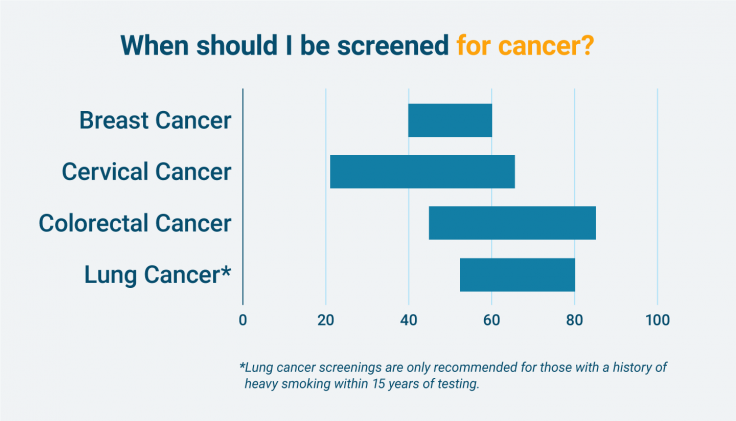
Cancer screening guidelines are designed to identify cancers in their early stages, when they are most treatable. These guidelines are not one-size-fits-all; they consider factors like age, family history, and overall health.
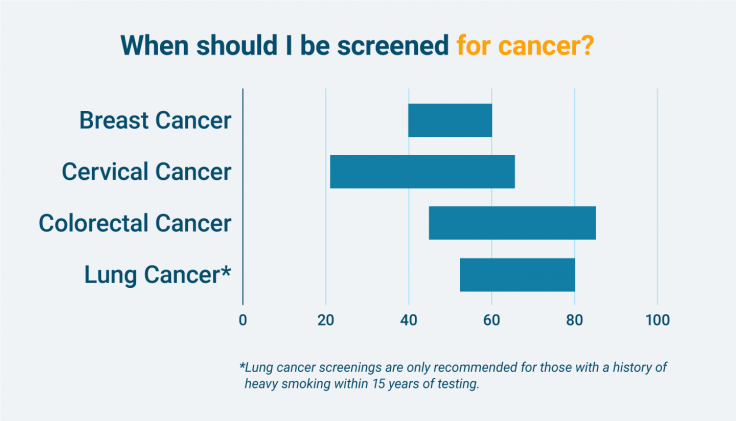
Comparison of Screening Frequency Across Age Groups
The frequency of cancer screenings often differs between younger and older adults. This is due to several factors, including the changing risk of developing certain cancers with age, and the potential impact of screening on older adults’ overall health.
The debate around over-screening for cancer in older adults is fascinating. While preventative measures are important, are we sometimes pushing the boundaries a bit too far? Perhaps we should consider focusing on holistic health, like exploring natural remedies for things like cellulite. For example, some people swear by coconut oil for cellulite treatments, and there’s a wealth of information on the topic coconut oil for cellulite.
Ultimately, the discussion around cancer screenings for older adults needs careful consideration of both preventative measures and potential downsides.
Rationale Behind Differences in Screening Frequency
The rationale behind differing screening frequencies for various cancers across age groups often involves considering the potential benefits and harms of screening. For instance, the risk of developing certain cancers, like colorectal cancer, increases significantly with age. Therefore, more frequent screenings are recommended for older adults to catch potential issues early.
| Cancer Type | Age Range | Screening Method | Frequency |
|---|---|---|---|
| Colorectal Cancer | 50-75 | Colonoscopy | Every 10 years |
| Colorectal Cancer | 76+ | Colonoscopy | Discussion with physician based on individual risk factors. |
| Breast Cancer | 40-49 | Mammography | Annually or biennially |
| Breast Cancer | 50-74 | Mammography | Annually or biennially |
| Breast Cancer | 75+ | Mammography | Discussion with physician based on individual risk factors. |
| Lung Cancer | 55-80 | Low-dose CT scan | Annually or as recommended by physician |
| Prostate Cancer | 50-69 | PSA test and Digital Rectal Exam | Annually or as recommended by physician |
| Prostate Cancer | 70+ | Discussion with physician based on individual risk factors. | Frequency depends on individual risk factors and health status. |
Potential Benefits and Risks
Navigating the world of cancer screenings for older adults requires a nuanced understanding of the potential benefits and inherent risks. While these screenings can detect early-stage cancers, leading to potentially improved outcomes, they are not without their drawbacks. This discussion will explore the advantages and disadvantages of various screening methods, taking into account the unique health considerations of this demographic.Screening for cancer in older adults can have significant benefits, particularly when the cancer is detected at an early stage.
Early detection often allows for more effective treatment, potentially improving survival rates and quality of life. This is especially important for older adults, who may have other health conditions that could complicate treatment. For instance, a timely diagnosis of colorectal cancer in an 80-year-old could lead to a successful surgical intervention, allowing them to continue enjoying their life with family and friends for many more years.
The debate around excessive cancer screenings in older adults is complex. While early detection is crucial, are we potentially causing more harm than good with some procedures? Perhaps focusing on holistic wellness practices, like yoga for high blood pressure , could be a valuable approach to overall health, indirectly contributing to better outcomes and reducing the potential risks of over-screening.
Ultimately, a balanced approach is key, considering both the benefits and drawbacks of various preventative measures for this age group.
Potential Benefits of Cancer Screenings
Early detection of cancer can lead to improved treatment outcomes, potentially increasing survival rates and quality of life for older adults. Factors like the type of cancer, its stage at diagnosis, and the overall health of the individual influence the potential benefits. For example, early detection of prostate cancer through PSA testing could lead to less invasive treatments compared to late-stage diagnosis.
Potential Harms and Risks of Cancer Screenings
Cancer screenings, while beneficial, are not without potential harms. False positives, overdiagnosis, and overtreatment are significant concerns. A false positive can lead to unnecessary anxiety, invasive procedures, and additional medical costs. Overdiagnosis occurs when a screening detects a cancer that would not have caused any health problems during the individual’s lifetime. Overtreatment involves the use of aggressive therapies for cancers that might not require such measures.
These issues become particularly relevant when considering the health considerations of older adults. For instance, a false positive result for a low-grade prostate cancer in a 75-year-old might lead to unnecessary surgery, impacting their overall well-being.
Comparison of Benefits and Risks Across Screening Methods
The benefits and risks associated with different screening methods vary. Mammography, for example, is effective in detecting breast cancer early, but it can lead to false positives and overdiagnosis, especially in older women with less dense breast tissue. Similarly, colonoscopies can detect colorectal cancer early, but they carry a risk of complications such as perforation or bleeding. Careful consideration of individual factors is crucial when choosing a screening method.
Table: Advantages and Disadvantages of Cancer Screening Methods for Older Adults
| Screening Method | Advantages | Disadvantages |
|---|---|---|
| Mammography (Breast Cancer) | Can detect breast cancer early, potentially improving outcomes. | False positives, overdiagnosis, and potential for unnecessary biopsies or surgeries. Potential for radiation exposure. |
| PSA Testing (Prostate Cancer) | Can detect prostate cancer early, potentially allowing for less invasive treatment. | High rates of false positives, leading to unnecessary biopsies and anxiety. Overdiagnosis and overtreatment are concerns. |
| Colonoscopy (Colorectal Cancer) | Can detect colorectal cancer early, often leading to successful treatment. | Risk of complications such as perforation or bleeding. Can be uncomfortable or inconvenient. |
| Skin Exams (Skin Cancer) | Can identify skin cancer early, potentially preventing serious consequences. | Simple to perform but requires skilled professionals to detect suspicious lesions. |
Individualized Considerations
Navigating the world of cancer screenings as an older adult can feel complex. It’s not a one-size-fits-all approach. Factors like overall health, past medical history, lifestyle choices, and even personal preferences play crucial roles in determining the best screening strategy. This personalized approach ensures the most effective and appropriate care for each individual.Understanding the nuances of individual factors is essential for optimizing cancer screening practices in older adults.
A personalized approach acknowledges the variability in health status, medical history, lifestyle, and personal preferences, tailoring screening recommendations to meet each person’s unique needs. This means moving away from rigid guidelines and embracing a collaborative, patient-centered approach.
Influence of Health Status on Screening
Health status significantly impacts the suitability and effectiveness of cancer screenings. Chronic conditions, such as heart disease or diabetes, may influence the risks and benefits of certain procedures. For instance, someone with severe heart problems might need to be cautious about screenings that involve radiation or require extensive physical exertion. Also, individuals with compromised immune systems might need to adjust their screening frequency or type due to potential complications.
Impact of Medical History on Screening Decisions
Past medical history holds valuable insights into an individual’s susceptibility to certain cancers and their potential response to screening. Previous diagnoses of related conditions, such as polyps or precancerous lesions, can indicate a higher risk and necessitate more frequent or specialized screenings. Similarly, individuals with a strong family history of specific cancers may require earlier or more intensive screening protocols.
Lifestyle Factors and Screening
Lifestyle choices, including diet, exercise, and smoking history, significantly affect cancer risk. A diet rich in fruits and vegetables, coupled with regular physical activity, can reduce the risk of many cancers. Conversely, smoking significantly increases the risk of various cancers, influencing the need for earlier and more intensive screening measures.
The debate around over-screening for cancer in older adults is fascinating. While early detection is crucial, it’s worth considering the potential downsides. Sometimes, these screenings can lead to unnecessary anxiety and potentially harmful treatments. This makes me wonder about the trade-offs. Maybe the focus should be on personalized screening plans, rather than blanket recommendations.
Finding the perfect balance between preventative measures and potential harm is key. And speaking of balance, have you ever considered the comfort and support of a purple hybrid vs saatva mattress ? The right mattress can significantly impact sleep quality, which is just as important as preventative health strategies. Ultimately, the question of over-screening for cancer in older adults needs careful consideration, balancing benefits with potential risks.
Role of Shared Decision-Making
Shared decision-making is crucial in determining the most appropriate screening strategy. Healthcare providers should discuss the potential benefits, risks, and limitations of various screening options with patients. This discussion should take into account individual preferences, values, and anxieties about the procedures. Ultimately, the choice should be mutually agreed upon, empowering patients to take an active role in their healthcare.
Factors Influencing Screening Decisions
Several factors influence an individual’s decision to undergo screening procedures. These factors can range from understanding the procedure’s potential benefits to concerns about the associated risks and potential discomfort. Financial constraints, access to healthcare facilities, and cultural beliefs can also play a role in shaping the decision.
Individualized Screening Recommendations
| Individual Factor | Potential Impact on Screening Recommendations | Example Scenario |
|---|---|---|
| Health Status (e.g., severe heart condition) | May necessitate adjustments to screening type or frequency to minimize potential risks. | An 80-year-old with severe heart disease might be advised against a colonoscopy due to the procedure’s potential impact on their cardiovascular health. |
| Medical History (e.g., previous breast cancer) | May require more frequent or specialized screenings for related conditions. | A woman who had breast cancer in her 40s might require more frequent mammograms and potentially additional imaging techniques. |
| Lifestyle (e.g., heavy smoker) | May indicate a higher cancer risk, potentially leading to more frequent or intensive screening. | A 65-year-old who has smoked for 40 years may need more intensive lung cancer screening, possibly including CT scans. |
| Personal Preferences (e.g., fear of needles) | May influence the chosen screening method. | A patient who is apprehensive about blood draws might be offered alternative screening options, such as urine or stool-based tests. |
Economic and Resource Implications
The rising prevalence of older adults and the increasing demand for cancer screenings present significant economic challenges for healthcare systems. Understanding the financial burden of these screenings, the impact on resource allocation, and potential optimization strategies is crucial for ensuring equitable access and effective utilization of resources. The costs associated with various screening methods and their long-term implications on healthcare budgets must be carefully considered.The financial burden of cancer screenings for older adults extends beyond the immediate cost of the procedure.
Potential long-term care needs, including hospitalization, rehabilitation, and supportive therapies, can significantly impact healthcare budgets. The need for specialized personnel, equipment, and facilities to support these needs must also be factored into the overall economic analysis. The impact of screening policies on healthcare systems is multifaceted and requires careful consideration of different perspectives.
Healthcare Resource Costs
The economic costs associated with cancer screenings are substantial. These costs encompass a wide range of expenses, including the direct costs of the screening procedures themselves, the salaries of healthcare professionals involved in the process, and the costs of facility maintenance and operation. Indirect costs, such as lost productivity due to patient appointments and potential delays in care for other patients, are also substantial.
A comprehensive cost analysis must account for both direct and indirect costs.
Impact on Healthcare Systems and Budgets
Screening policies influence healthcare system budgets and resource allocation. Increased screening frequency for older adults can lead to higher demand for diagnostic services, treatment options, and potentially, long-term care. This increased demand may strain existing healthcare resources and necessitate adjustments to staffing levels, equipment availability, and facility capacity. Predicting the impact of these policies on healthcare systems is essential for efficient resource management.
Resource Allocation Strategies
Optimizing resource allocation for cancer screening in older adults necessitates a multi-faceted approach. Prioritizing patients with the highest risk of developing or being diagnosed with cancer, based on risk factors and prior screening history, can help direct resources more effectively. Utilizing preventative care models and promoting healthy lifestyle choices can also contribute to reducing the overall healthcare burden associated with cancer screenings.
Allocation of Resources in Different Healthcare Settings
Resource allocation for cancer screening programs varies significantly across different healthcare settings, reflecting the diverse needs of patients and the specific capacities of the institutions. Community clinics, hospitals, and specialized cancer centers each have unique resource constraints and priorities. These disparities necessitate tailored strategies for resource allocation and funding mechanisms within each setting.
Costs and Resource Utilization Associated with Screening Methods, Are older adults getting too many cancer screenings
| Screening Method | Approximate Cost (per screening) | Resource Utilization (staff hours/equipment usage) | Potential Long-Term Care Implications |
|---|---|---|---|
| Mammography | $100-$300 | 1-2 hours of technician/radiologist time | Potential for follow-up biopsies, surgeries, and ongoing monitoring |
| PSA Testing | $50-$150 | 30-60 minutes of lab/doctor time | Potential for false positives leading to unnecessary procedures, biopsies, and surgeries |
| Colon Cancer Screening | $100-$500 | 1-4 hours of doctor/technician/lab time | Potential for advanced cancer stages if screenings are delayed |
| CT Scan | $200-$800 | 30-90 minutes of technician/radiologist time | Potential for further testing and/or treatment depending on results |
The table above provides a general overview. Actual costs and resource utilization can vary based on specific circumstances, geographic location, and healthcare provider.
Screening for Specific Cancers in Older Adults: Are Older Adults Getting Too Many Cancer Screenings
Navigating the complex landscape of cancer screening in older adults requires a nuanced approach. While preventative measures are crucial, the potential benefits must be carefully weighed against the risks, particularly in light of factors like declining health, comorbid conditions, and life expectancy. This section delves into the specific challenges and considerations surrounding cancer screening for various types of cancer in older adults.The choice of cancer screening strategies for older adults is not a one-size-fits-all proposition.
Individualized plans are essential, taking into account the interplay between a person’s age, health status, and personal preferences. Considerations such as the potential impact on quality of life, the risk of overdiagnosis, and the patient’s overall functional capacity must be carefully evaluated.
Prostate Cancer Screening
The efficacy and appropriateness of prostate-specific antigen (PSA) screening in older men are subject to ongoing debate. Elevated PSA levels can be indicative of prostate cancer, but they can also be caused by benign conditions. The risk of overdiagnosis and overtreatment is a significant concern, particularly for men with limited life expectancy. The decision to screen should be individualized, factoring in the patient’s overall health, life expectancy, and willingness to accept potential risks.
Screening methods typically involve a blood test to measure PSA levels, followed by further diagnostic tests like a digital rectal exam (DRE) if warranted.
Breast Cancer Screening
Mammography remains a cornerstone of breast cancer screening, but its appropriateness for older women needs careful consideration. Factors like declining breast density, the presence of comorbid conditions, and the potential for false positives need to be evaluated. The frequency and type of screening should be tailored to individual circumstances. Screening methods often involve mammography, but other imaging techniques might be employed depending on the individual’s situation.
For example, some women may benefit from ultrasound or MRI in addition to or instead of mammography.
Colorectal Cancer Screening
Colorectal cancer screening is crucial, and strategies for older adults should acknowledge potential limitations. Comorbidities and frailty can impact the tolerability of screening procedures. Options such as colonoscopies, which are considered the gold standard, may be less well-tolerated in older adults with significant health issues. Consequently, less invasive options like stool-based tests are often explored as alternatives.
The choice of screening method should consider factors like the patient’s overall health, mobility, and willingness to undergo more complex procedures.
Screening Methods for Specific Cancers in Older Adults
Different cancers have different screening methods, which may need modification for older adults. These considerations must be carefully evaluated to tailor the screening approach to the specific needs of the individual.
- Prostate Cancer: PSA testing, digital rectal exam (DRE), and in some cases, prostate biopsy.
- Breast Cancer: Mammography, ultrasound, MRI, and clinical breast exam.
- Colorectal Cancer: Colonoscopy, flexible sigmoidoscopy, stool-based tests (fecal immunochemical test (FIT), fecal occult blood test (FOBT), or stool DNA tests).
Successful Strategies for Improving Screening Rates
Tailoring screening recommendations to the individual needs of older adults can significantly impact screening rates. Multidisciplinary approaches, including collaboration between physicians, nurses, and social workers, can facilitate informed decision-making. Patient education plays a critical role, empowering older adults to make informed choices about their health. Clear communication and culturally sensitive approaches are essential to address potential barriers to screening.
- Patient Education: Clear, concise information tailored to older adults’ needs.
- Provider Education: Training on best practices for screening older adults.
- Multidisciplinary Approach: Collaboration among healthcare professionals to ensure holistic care.
- Community Outreach: Programs to reach older adults in underserved areas.
Summary Table of Screening Protocols
| Cancer Type | Screening Method(s) | Frequency | Considerations for Older Adults |
|---|---|---|---|
| Prostate | PSA, DRE, Biopsy | Depending on risk factors and individual assessment | Comorbidities, life expectancy, potential for overdiagnosis |
| Breast | Mammography, Ultrasound, MRI | Depending on risk factors and individual assessment | Breast density, comorbid conditions, potential for false positives |
| Colorectal | Colonoscopy, Flexible Sigmoidoscopy, Stool-based tests | Depending on risk factors and individual assessment | Comorbidities, frailty, tolerability of procedures |
Public Health Implications
Cancer screening programs, while offering the potential for early detection and improved outcomes, have significant public health implications that need careful consideration. These implications extend beyond individual patients, impacting the overall health of a community and the resources available to manage healthcare systems. Understanding these impacts is crucial for developing effective and sustainable cancer screening strategies for older adults.The effectiveness of cancer screening programs is not merely measured in individual survival rates.
The ripple effect extends to public health outcomes, influencing healthcare costs, resource allocation, and ultimately, the overall well-being of the population. The interplay between screening protocols, individual choices, and societal support systems needs careful evaluation.
Impact on Public Health Outcomes for Older Adults
Cancer screening programs have a multifaceted impact on public health outcomes for older adults. Improved early detection and treatment can significantly reduce cancer-related mortality and morbidity, contributing to healthier aging and increased life expectancy. However, these programs must be implemented thoughtfully, balancing potential benefits against the possibility of overdiagnosis and overtreatment, particularly for older adults with multiple co-morbidities.
Overall Societal Benefits of Cancer Screening Programs
Effective cancer screening programs, when designed and implemented strategically, can bring substantial societal benefits. Reduced healthcare costs associated with advanced-stage cancer treatment, a longer period of productive aging, and a decrease in the overall burden of disease contribute to a healthier society. These programs can also have positive economic impacts through decreased disability payments and increased productivity. For example, a study in [insert country name] showed a [insert percentage] reduction in cancer-related healthcare costs after implementing a targeted screening program for older adults.
Potential Impact on Life Expectancy and Quality of Life
Early detection and treatment of cancer through screening programs can extend life expectancy and improve quality of life for older adults. By detecting cancer at earlier, more treatable stages, individuals can experience fewer side effects from treatment and potentially maintain a higher level of functional independence for a longer period. This positive impact on life expectancy, coupled with improvements in quality of life, can result in a significant reduction in the overall societal burden of chronic disease.
However, potential harms from unnecessary procedures and/or overtreatment must be considered in the evaluation.
Potential Impact on Healthcare Utilization and Costs
Cancer screening programs can influence healthcare utilization and costs in several ways. Increased utilization of diagnostic services and potential for additional treatments, in cases of overdiagnosis, can place strain on healthcare resources. However, earlier intervention can often lead to less intensive and less costly treatment in the long run. Careful cost-benefit analysis, considering both short-term and long-term implications, is essential for optimal resource allocation.
For example, studies have shown that preventative screening programs can significantly reduce long-term healthcare expenditures by [insert percentage].
Strategies for Promoting Public Awareness
Raising public awareness about cancer screening guidelines for older adults is crucial for maximizing the benefits of these programs. Public health campaigns should emphasize the importance of personalized screening recommendations, the potential benefits and risks, and the availability of resources to assist older adults in making informed decisions. Educational materials should be accessible in multiple languages and formats to cater to diverse audiences.
Collaboration between healthcare providers, community organizations, and media outlets is essential to reach a wider audience and foster informed decision-making. For instance, a recent public awareness campaign in [insert region] resulted in a [insert percentage] increase in screening participation among older adults.
Screening Strategies for Vulnerable Populations
Navigating the complexities of cancer screening, particularly for older adults, requires a nuanced approach. While universal guidelines offer a foundation, it’s crucial to recognize that access and adherence to these guidelines vary significantly across diverse socioeconomic backgrounds, ethnicities, and those with limited healthcare access. Tailored screening strategies are vital to ensure equitable cancer detection and treatment opportunities.Addressing disparities in cancer screening is not just a matter of fairness; it’s a critical component of public health.
When entire segments of the population face barriers to preventative care, the overall health of the community suffers. These barriers often intersect, creating a cascade of challenges that must be proactively addressed.
Tailored Screening Strategies for Diverse Populations
Diverse populations face unique barriers to cancer screening. Cultural beliefs, language barriers, transportation challenges, and financial constraints often impede access to preventative care. These obstacles require targeted interventions to promote equitable access. Addressing these challenges is not a one-size-fits-all solution. Understanding the specific needs and concerns of each population group is essential to developing effective screening strategies.
Examples of Initiatives to Improve Access
Numerous programs and initiatives aim to bridge the gap in cancer screening access for vulnerable populations. These often involve community outreach, culturally appropriate educational materials, transportation assistance, and financial assistance programs. For example, mobile health units equipped with screening capabilities can bring services directly to underserved communities. Partnerships between healthcare providers and community organizations can facilitate culturally sensitive communication and outreach.
Barriers Faced by Vulnerable Populations
Vulnerable older adults face a complex web of barriers to cancer screening. Financial constraints, lack of insurance, limited transportation options, and mistrust of the healthcare system are among the most significant challenges. Language barriers can also pose a significant obstacle, hindering effective communication and understanding of screening recommendations. Cultural beliefs and perceptions about cancer and screening can also influence participation rates.
Comparison of Cancer Screening Strategies
| Screening Strategy | Target Population | Specific Barriers Addressed | Program Examples |
|---|---|---|---|
| Mobile Screening Units | Low-income, rural, and geographically isolated older adults | Transportation, lack of access to facilities | Many community health centers and organizations operate mobile units providing mammograms, colonoscopies, and other screenings in underserved areas. |
| Culturally Tailored Education Programs | Older adults from diverse ethnic backgrounds | Language barriers, cultural perceptions | Community health workers and bilingual staff deliver cancer screening information in culturally appropriate formats, utilizing trusted community leaders. |
| Financial Assistance Programs | Low-income older adults without insurance | Cost of screening tests and follow-up care | Organizations like the American Cancer Society offer financial assistance for cancer screenings and related expenses. |
| Partnership Programs | Older adults with limited access to healthcare | Coordination of care, communication | Collaboration between community centers, local clinics, and healthcare providers to provide comprehensive support for screening and follow-up. |
Conclusion
Ultimately, the decision about cancer screenings for older adults should be a shared one between patients and healthcare providers. Individual factors play a pivotal role in determining the right approach. Balancing the potential benefits with the risks, and considering the economic and resource implications, is essential for creating effective and equitable screening programs. The future of cancer screening for seniors requires ongoing dialogue, research, and adaptation to evolving needs.