Are pituitary tumors hereditary? This question delves into the fascinating interplay between genetics and the development of these often-subtle yet impactful tumors. We’ll explore the intricate relationship between genes, family history, and the likelihood of pituitary tumors, examining potential inheritance patterns and the role of various factors.
Understanding the potential for hereditary pituitary tumors is crucial for both individuals and their families. This comprehensive exploration investigates the genetic mechanisms involved, highlighting specific syndromes and the current research aimed at uncovering the causes and implications of these tumors. We will examine the different types of pituitary tumors, their common symptoms, and potential causes, and delve into the role of family history.
Introduction to Pituitary Tumors: Are Pituitary Tumors Hereditary
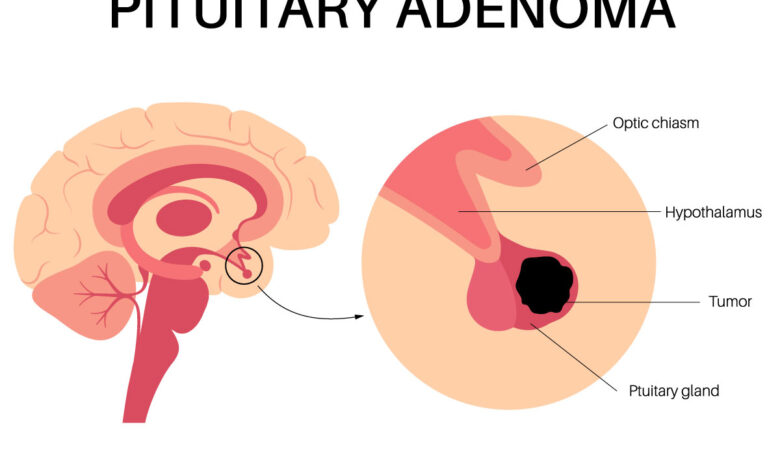
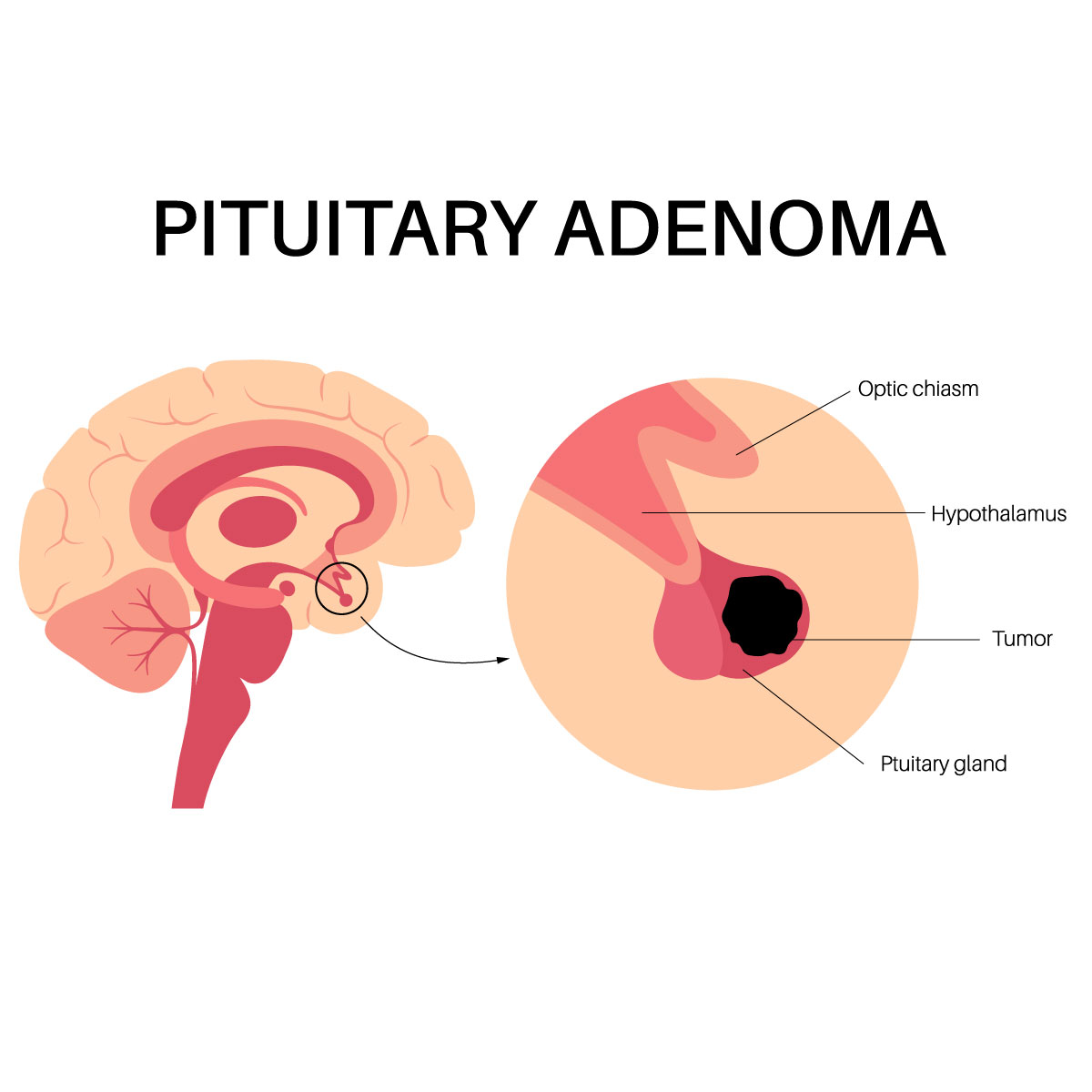
The pituitary gland, often called the “master gland,” is a small, pea-sized organ located at the base of the brain, nestled within a bony structure called the sella turcica. It plays a crucial role in regulating various bodily functions by producing hormones that influence growth, metabolism, reproduction, and other essential processes. Sometimes, abnormal growth within this delicate gland can lead to the development of pituitary tumors.Pituitary tumors are growths of abnormal cells within the pituitary gland.
These tumors can vary significantly in size and behavior, ranging from benign (non-cancerous) microadenomas that are barely detectable to larger, potentially aggressive adenomas. The impact of these tumors depends heavily on their size, location, and the hormones they produce. Understanding the different types of pituitary tumors and their potential effects is crucial for diagnosis and effective treatment.
Types of Pituitary Tumors
Pituitary tumors are categorized based on whether they produce hormones (functioning or hormone-secreting tumors) or do not (non-functioning or non-hormone-secreting tumors). Understanding the different types is essential to identifying potential symptoms and appropriate treatment approaches. Functioning tumors can further be classified by the hormone they overproduce.
While the inheritance of pituitary tumors is a complex topic, recent research suggests they aren’t typically passed down through families in a straightforward way. This contrasts with the current FDA discussions about banning codeine in cough syrups for children, a move driven by concerns about its potential adverse effects. The FDA’s decision highlights the importance of understanding the risks and benefits of various medications, and ultimately, further research on the causes of pituitary tumors is crucial.
fda on the verge of banning codeine in cough syrup for children is a fascinating look at the FDA’s role in safeguarding public health. The potential link between these seemingly disparate issues, however, is still a subject of ongoing investigation for pituitary tumor research.
Location and Function of the Pituitary Gland, Are pituitary tumors hereditary
The pituitary gland is situated at the base of the brain, just below the hypothalamus. This critical location allows for close communication between the brain and the endocrine system. Its function is to receive signals from the hypothalamus, which then regulates hormone production and release. This complex interplay affects a multitude of bodily processes.
Characteristics of Pituitary Tumors
| Tumor Type | Common Symptoms | Potential Causes |
|---|---|---|
| Prolactinoma | Infertility, decreased libido, irregular menstrual cycles (women), breast milk production (galactorrhea) in both men and women, headaches, vision problems | Unknown, but genetic predisposition and other factors may play a role. |
| Growth Hormone Adenoma | Gigantism (in children), acromegaly (in adults), increased body size, headaches, vision problems, excessive sweating, and/or glucose intolerance. | Unknown, but genetic predisposition and other factors may play a role. |
| Adrenocorticotropic Hormone (ACTH) Adenoma | Cushing’s syndrome, characterized by weight gain (especially in the face and trunk), stretch marks, muscle weakness, high blood pressure, and diabetes. | Unknown, but genetic predisposition and other factors may play a role. |
| Non-functioning Adenoma | Often asymptomatic or with vague symptoms like headaches, vision problems, or hypopituitarism (insufficient hormone production). | Unknown, but genetic predisposition and other factors may play a role. |
Genetics and Heredity
Understanding the genetic underpinnings of pituitary tumors is crucial for predicting risk, tailoring treatment strategies, and potentially identifying individuals at higher risk. While the exact mechanisms aren’t fully elucidated, several genetic factors are known to play a role in tumor development. This section will delve into the known genetic factors and their potential impact on pituitary tumor formation.
Known Genetic Factors
The development of pituitary tumors is a complex process often influenced by a combination of genetic and environmental factors. While environmental factors remain largely unknown, certain genetic predispositions are increasingly recognized. Genetic mutations can disrupt normal cell growth and signaling pathways, leading to the uncontrolled proliferation of cells, ultimately resulting in a tumor.
Specific Genes and Mutations
Several specific genes have been identified as being associated with an increased risk of pituitary tumors. Mutations in these genes can lead to abnormal protein function, which in turn disrupts the delicate balance required for healthy cell growth and development. One example is the MEN1 gene, mutations in which are linked to multiple endocrine neoplasia type 1 (MEN1), a syndrome characterized by the development of tumors in various endocrine glands, including the pituitary.
Inheritance Patterns
The inheritance patterns of pituitary tumors vary depending on the specific genetic factors involved. Some pituitary tumor types exhibit an autosomal dominant inheritance pattern, meaning that an individual only needs to inherit one mutated copy of the gene to be at risk. Other types may follow an autosomal recessive pattern, requiring the inheritance of two mutated copies of the gene for the individual to be affected.
These patterns can significantly influence the likelihood of family members developing similar tumors.
Family History
A strong family history of pituitary tumors can be a significant risk factor. Individuals with a family history of pituitary tumors, especially if multiple family members are affected, may have a higher predisposition to developing the condition themselves. This suggests that genetic factors play a crucial role in the development of these tumors. This isn’t a guarantee, but the risk is definitely elevated.
Genetic Mechanisms and Tumor Formation
| Genetic Mechanism | Relation to Tumor Formation |
|---|---|
| Mutations in genes controlling cell growth and division | Disrupting the normal cell cycle, leading to uncontrolled cell proliferation and tumor formation. |
| Mutations in genes involved in signal transduction pathways | Altering communication between cells, leading to aberrant cell behavior and tumor growth. |
| Inherited syndromes | These syndromes often predispose individuals to developing tumors in multiple endocrine glands, including the pituitary. |
| Epigenetic modifications | Changes in gene expression without altering the DNA sequence, potentially contributing to tumor development. |
Familial Pituitary Tumor Syndromes
Beyond sporadic cases, some individuals inherit a predisposition to developing pituitary tumors. These familial syndromes often involve multiple endocrine organs, highlighting the intricate interplay between genetics and endocrine function. Understanding these inherited conditions is crucial for early detection and personalized management strategies.Familial pituitary tumor syndromes are characterized by a genetic predisposition that increases the risk of developing pituitary adenomas and, sometimes, tumors in other endocrine glands.
These syndromes are typically associated with specific genetic mutations, which can be identified through genetic testing. Early diagnosis and management are essential to minimize the impact on patient health.
Specific Inherited Syndromes
Several inherited syndromes are linked to pituitary tumors. These syndromes are characterized by a combination of genetic mutations and clinical features that affect multiple endocrine glands. A thorough understanding of these syndromes allows for targeted interventions and appropriate management.
Clinical Features of Familial Syndromes
Clinical manifestations of familial pituitary tumor syndromes vary depending on the specific syndrome and the genetic mutation involved. A common thread is the increased risk of pituitary adenomas, often with specific hormonal imbalances as a result. For instance, a mutation in the MEN1 gene may lead to an increased risk of prolactinomas or growth hormone-secreting adenomas, resulting in symptoms such as galactorrhea, gynecomastia, and/or acromegaly.
Prevalence and Incidence of Syndromes
Precise prevalence and incidence figures for specific familial pituitary tumor syndromes can be challenging to determine due to the often-subtle presentation of the condition and the limited availability of large-scale epidemiological studies. However, some syndromes, such as Multiple Endocrine Neoplasia type 1 (MEN1), are recognized as relatively rare, but their potential for significant morbidity emphasizes the importance of early detection and management.
Comparison of Familial Syndromes
Different familial pituitary tumor syndromes exhibit distinct characteristics. For example, MEN1 syndrome often involves tumors in the parathyroid glands, pancreas, and anterior pituitary, whereas Carney complex, while also affecting pituitary function, often includes other clinical features like skin pigmentation and cardiac myxoma. These differences in the spectrum of affected organs and the associated symptoms necessitate tailored management strategies for each syndrome.
While the exact inheritance patterns of pituitary tumors aren’t fully understood, researchers are actively studying the potential genetic links. This kind of exploration is crucial, as early detection is key, mirroring the importance of early detection strategies in conditions like colon cancer. For instance, the article detecting colon cancer earlier treating later highlights the benefits of screening and preventative measures.
Ultimately, understanding the hereditary component of pituitary tumors will help refine strategies for early diagnosis and treatment, just as research in other areas continues to improve the chances of successful outcomes.
Summary Table of Familial Pituitary Tumor Syndromes
| Syndrome | Associated Genes | Pituitary Tumor Types | Other Endocrine Involvement | Clinical Features (Pituitary) |
|---|---|---|---|---|
| Multiple Endocrine Neoplasia Type 1 (MEN1) | MEN1 | Prolactinomas, growth hormone-secreting adenomas, ACTH-secreting adenomas | Parathyroid hyperplasia, pancreatic tumors | Galactorrhea, acromegaly, Cushing’s disease |
| Carney Complex | PRKAR1A, other genes | Prolactinomas, ACTH-secreting adenomas | Skin pigmentation, cardiac myxoma | Galactorrhea, Cushing’s disease |
| McCune-Albright Syndrome | GNAS | Prolactinomas, growth hormone-secreting adenomas | Fibrous dysplasia, café-au-lait spots | Galactorrhea, acromegaly |
Risk Factors and Inheritance Patterns
Understanding the risk factors and inheritance patterns of pituitary tumors is crucial for both prevention and early detection. While not all pituitary tumors are hereditary, a significant portion are linked to specific genetic predispositions. This understanding allows for targeted screening and management strategies, particularly within families with a history of these conditions.
Potential Risk Factors
Identifying factors that increase the likelihood of developing pituitary tumors is vital for proactive health management. Beyond genetics, various environmental influences may play a role in pituitary tumor development.
- Genetic Predisposition: Certain genetic mutations can significantly increase the risk of pituitary tumors. These mutations are often associated with specific syndromes, such as multiple endocrine neoplasia type 1 (MEN1) and Carney complex. These syndromes are characterized by the development of tumors in multiple endocrine glands, not just the pituitary. Individuals with a family history of pituitary tumors or these syndromes are at higher risk.
- Environmental Factors: While the precise mechanisms are still under investigation, environmental factors might contribute to pituitary tumor development. Exposure to certain toxins, radiation, or specific medications could potentially play a role. However, the evidence linking these factors to pituitary tumors is often circumstantial and not definitive.
- Age: Pituitary tumors can occur at any age, but there is a slight tendency for them to occur more frequently in middle-aged individuals.
- Gender: Some studies suggest a slight difference in incidence rates between genders, but this is not a consistent finding across all research.
Inheritance Patterns in Familial Pituitary Tumor Syndromes
The inheritance patterns of pituitary tumors vary greatly depending on the specific genetic condition.
- Autosomal Dominant Inheritance: In conditions like MEN1, a single mutated gene from either parent can lead to the development of pituitary tumors. This means an affected individual has a 50% chance of passing the mutation on to their offspring. For example, if one parent has MEN1, their children have a 50% chance of inheriting the predisposition.
- Autosomal Recessive Inheritance: In some cases, two mutated genes, one from each parent, are required to trigger the development of pituitary tumors. This inheritance pattern is less common than autosomal dominant. For example, a child inherits one mutated copy from each parent and has a much higher chance of developing the condition.
Evidence Supporting or Refuting Hereditary Nature
Extensive research supports the hereditary nature of pituitary tumors in specific syndromes. Genetic testing is crucial in identifying individuals at increased risk, allowing for proactive screening and management. For example, families with a history of MEN1 are often screened for pituitary tumors and other endocrine abnormalities.
Flowchart of Potential Pathways
A simplified flowchart depicting potential pathways from genetic predisposition to pituitary tumor development is as follows:
(Please note that this is a simplified representation and does not encompass all possible pathways.)
Genetic Mutation (e.g., MEN1)
|
|
Increased Risk of Pituitary Tumor
|
|
Exposure to Environmental Factors (hypothetical)
|
|
Pituitary Tumor Development
Diagnostic Methods
Pinpointing the cause of pituitary tumors, especially hereditary ones, requires a multi-faceted approach.
The process involves a series of tests and assessments to determine the type, size, and location of the tumor, along with evaluating potential genetic predispositions. This comprehensive evaluation helps guide treatment decisions and monitor disease progression.
While pituitary tumors can sometimes run in families, they aren’t always hereditary. Recent studies on the correlation between various factors and pituitary tumor development are ongoing. Interestingly, a significant number of e-scooter accidents involve alcohol, as detailed in this article on scooter DUI and most e-scooter accidents related to drinking. This highlights the complex interplay of lifestyle choices and health conditions.
Ultimately, the inheritance patterns of pituitary tumors are still being researched.
The diagnosis of pituitary tumors, especially when hereditary factors are suspected, necessitates a meticulous investigation. This involves a combination of clinical evaluations, imaging techniques, hormone assays, and genetic testing. The interplay between these methods provides a clearer picture of the tumor’s characteristics and the patient’s individual risk profile.
Clinical Evaluation
Thorough medical history taking and a physical examination are the initial steps in the diagnostic process. Symptoms, such as headaches, visual disturbances, or hormonal imbalances, are carefully documented. The doctor assesses the patient’s family history for any occurrences of pituitary tumors or related conditions, paying close attention to patterns of inheritance. This initial assessment provides crucial insights for directing further investigations.
Imaging Techniques
Magnetic resonance imaging (MRI) is a critical imaging technique used to visualize the pituitary gland and surrounding structures. MRI scans can reveal the presence, size, and location of pituitary tumors, distinguishing them from other abnormalities. The high resolution of MRI enables precise characterization of the tumor’s morphology. Computed tomography (CT) scans might also be employed to complement MRI findings, particularly for evaluating bone structures.
Hormone Assays
Hormonal analysis is essential to determine the specific hormone imbalances caused by the tumor. Blood tests measure levels of various hormones, such as growth hormone, prolactin, adrenocorticotropic hormone (ACTH), and thyroid-stimulating hormone (TSH). These tests are crucial for confirming the presence of a pituitary tumor and identifying the specific hormones being affected.
Genetic Testing
Genetic testing plays a vital role in diagnosing hereditary pituitary tumors. It identifies specific gene mutations that predispose individuals to developing these tumors. This information is particularly valuable for individuals with a family history of pituitary tumors or those presenting with atypical symptoms.
Genetic Testing Approaches
Various genetic testing approaches exist, each with its own strengths and weaknesses. Polymerase chain reaction (PCR) techniques are commonly used to amplify specific DNA sequences for mutation analysis. Next-generation sequencing (NGS) offers a broader spectrum of gene coverage, enabling the simultaneous screening of multiple genes implicated in pituitary tumor development. The choice of approach depends on the specific clinical scenario and the suspected genetic mutations.
Potential Genetic Tests
Several genes are associated with hereditary pituitary tumor syndromes. These include, but are not limited to, MEN1, AIP, PRKAR1A, and NF1. The selection of specific genes for testing depends on the patient’s family history and the suspected syndrome.
Diagnostic Process
| Stage | Methods | Role of Genetic Testing |
|---|---|---|
| Initial Evaluation | Medical history, physical examination | Assess family history for patterns of pituitary tumors. |
| Imaging | MRI, CT scans | Visualize the pituitary gland and surrounding structures. Help determine the presence, size, and location of the tumor. |
| Hormonal Analysis | Blood tests for hormone levels | Identify hormone imbalances caused by the tumor. Confirm the presence of a pituitary tumor. |
| Genetic Testing | PCR, NGS | Identify specific gene mutations associated with hereditary pituitary tumor syndromes. Assess the risk of hereditary pituitary tumors. |
Current Research
Unraveling the mysteries behind pituitary tumors requires a deep dive into the genetic underpinnings. Current research is actively investigating the intricate relationships between specific genes, mutations, and the development of these tumors. This exploration is vital to understanding the predisposition to pituitary tumors, improving diagnostic accuracy, and potentially paving the way for personalized treatment strategies.
Ongoing studies are meticulously examining the genetic landscape of pituitary tumors, seeking to identify key players in the tumorigenesis process. Researchers are utilizing sophisticated genomic techniques to analyze DNA and RNA, hoping to find patterns and biomarkers that can predict tumor behavior and patient outcomes. This detailed examination allows for a deeper comprehension of the disease’s mechanisms, which is critical for future therapeutic developments.
Genetic Basis of Pituitary Tumors
Researchers are actively scrutinizing the specific genes implicated in pituitary tumor development. This involves comparing the genetic makeup of pituitary tumors with that of healthy pituitary tissue to pinpoint differences that might trigger or contribute to tumor formation. These studies aim to identify particular genetic variations or mutations that are strongly associated with pituitary tumor formation. Further investigation into the regulatory mechanisms that control the expression of these genes is crucial for a comprehensive understanding.
Ongoing Studies Investigating the Link Between Genetics and Pituitary Tumor Development
Numerous studies are investigating the role of specific genes in pituitary tumor development. Researchers are focusing on identifying genetic markers that could be used for early diagnosis and predicting tumor behavior. These investigations are meticulously exploring the intricate interplay between genetic predispositions and environmental factors that might contribute to the disease’s development. The outcomes of these studies hold promise for developing more effective diagnostic and prognostic tools.
Areas of Uncertainty and Gaps in Knowledge
While significant progress has been made, there remain gaps in our understanding of the genetic basis of pituitary tumors. The precise mechanisms by which specific genetic alterations contribute to tumor growth and function are still not fully understood in some cases. Further research is needed to unravel the intricate regulatory pathways that control pituitary hormone production and the interplay between genetic mutations and environmental factors.
This will enhance our ability to tailor treatments and personalize care for individuals affected by these tumors.
Methods Employed in Current Research Studies
Advanced genomic techniques are employed in current research to analyze the genetic makeup of pituitary tumors. These techniques include whole-exome sequencing, which identifies variations across the entire coding region of the genome, and RNA sequencing, which measures the expression levels of genes. Researchers also utilize bioinformatic tools to identify patterns and correlations between genetic alterations and clinical outcomes.
These advanced methods provide detailed information about the genetic changes involved in the development and progression of pituitary tumors.
Recent Research Findings on Hereditary Pituitary Tumors
- Studies have identified specific genetic mutations in families with a history of multiple pituitary tumors, suggesting a hereditary component. These mutations are often found in genes involved in cell cycle regulation, growth signaling, or DNA repair.
- Recent research indicates a correlation between specific genetic variants and the risk of developing certain types of pituitary adenomas. This knowledge can help in identifying individuals at higher risk for developing the condition.
- Investigations are revealing that genetic variations in specific genes may influence the aggressiveness of pituitary tumors, providing insights into potential prognostic markers.
- Research continues to identify rare familial syndromes linked to pituitary tumors, enhancing our understanding of the genetic mechanisms underlying pituitary tumor development.
Implications for Patients and Families
A hereditary predisposition to pituitary tumors significantly impacts the lives of affected individuals and their families. Understanding the implications, including the emotional and practical challenges, is crucial for providing comprehensive support and guidance. This knowledge empowers families to make informed decisions about genetic testing, counseling, and potential treatment strategies.
Hereditary pituitary tumor diagnoses bring a complex mix of emotions, from fear and anxiety about future health to the burden of potentially passing the predisposition to offspring. The implications extend beyond the patient, affecting family members who may be at risk and require their own support and understanding.
Genetic Counseling for Individuals at Risk
Genetic counseling plays a vital role in managing the implications of a hereditary pituitary tumor diagnosis. It provides a structured approach to understanding the risk, available options, and the potential impact on family members. This includes detailed explanations of the specific genetic condition, its inheritance pattern, the likelihood of developing a tumor, and strategies for risk reduction and early detection.
Counseling empowers individuals with the knowledge to make informed decisions about their health and family planning.
Benefits and Challenges of Genetic Testing
Genetic testing for individuals with a family history of pituitary tumors offers significant benefits, such as identifying those at high risk, enabling early monitoring, and potentially influencing treatment strategies. However, it also presents challenges, including the psychological impact of receiving positive or negative results and the potential for discrimination based on genetic information.
Potential Impact on Treatment Decisions
Genetic information can profoundly influence treatment decisions for individuals with pituitary tumors. Understanding the specific genetic mutation involved can aid in selecting the most effective treatment approach and potentially reduce the risk of recurrence. Personalized treatment plans, incorporating genetic insights, may lead to improved outcomes and reduced side effects. For example, knowing a specific gene mutation linked to aggressive tumor growth could prompt earlier and more aggressive intervention.
Comparison of Genetic Testing Options
| Testing Option | Potential Benefits | Potential Drawbacks |
|---|---|---|
| Comprehensive Gene Panel Testing | Identifies mutations across multiple genes associated with pituitary tumors, providing a broader understanding of risk and potentially leading to more personalized treatment strategies. | Can be more expensive and may not be covered by insurance. Results might be complex and require further interpretation by a specialist. Could reveal incidental findings unrelated to pituitary tumors. |
| Targeted Gene Testing | Focuses on specific genes known to be associated with pituitary tumors in a family. This can be more cost-effective and provide a more focused assessment of risk. | Might miss mutations in other genes that could contribute to risk. May not provide a complete picture of predisposition if the family history suggests involvement of other genes not yet identified. |
| Family History Assessment | Provides a framework for understanding the inheritance patterns of pituitary tumors within a family, potentially guiding risk assessment and genetic testing decisions. | May not identify specific genetic mutations but can inform the probability of a mutation existing in the family. Requires detailed information about family medical history, which might not always be readily available or accurate. |
Conclusive Thoughts
In conclusion, while a definitive answer to the question of are pituitary tumors hereditary isn’t always straightforward, we’ve uncovered a complex interplay between genetics and environmental factors. The potential for inherited syndromes, while not a guarantee, significantly increases the risk for certain individuals. Genetic testing, combined with careful consideration of family history, plays a vital role in diagnosis and management.
Ongoing research continues to shed light on the intricate pathways involved, offering hope for improved understanding and targeted treatment approaches.
