
Arrhythmia electrical activity circular pattern is a fascinating and complex aspect of cardiac function. This detailed exploration delves into the heart’s electrical signals, revealing how abnormal activity can manifest as circular patterns on an electrocardiogram (ECG). We’ll examine the characteristics of these patterns, their mechanisms, clinical implications, treatment strategies, and illustrative cases. Understanding these intricate processes is crucial for accurate diagnosis and effective treatment.
From defining arrhythmias and the heart’s electrical system to interpreting ECGs and exploring treatment options, this comprehensive guide unpacks the significance of circular patterns in arrhythmias. We’ll also discuss the monitoring and prevention strategies that are critical for patients with these conditions.
Defining Arrhythmia Electrical Activity
Arrhythmias are disturbances in the heart’s normal rhythm, a critical aspect of cardiovascular health. Understanding the electrical basis of these irregularities is crucial for diagnosis and treatment. This involves recognizing the normal electrical activity of the heart and how deviations from this norm lead to arrhythmias.The heart’s rhythmic contractions are driven by electrical impulses. These impulses originate and propagate through specialized cells in the heart, creating a coordinated wave of depolarization that causes the chambers to contract.
Understanding the circular pattern of electrical activity in arrhythmias is crucial. Sometimes, these irregular heart rhythms can be linked to high blood pressure, which can be treated with magnesium sulfate. For instance, a study of hypertension magnesium sulfate treatment hypertension magnesium sulfate treatment might reveal correlations between the two, shedding light on how the body responds to these conditions.
Ultimately, deciphering the electrical patterns of arrhythmias is key to proper diagnosis and treatment.
This precisely timed electrical activity is fundamental to maintaining a healthy heart rate and blood flow.
Normal Heart Electrical Activity
The heart’s electrical system involves a complex network of specialized cells, including the sinoatrial (SA) node, atrioventricular (AV) node, bundle of His, and Purkinje fibers. The SA node acts as the heart’s natural pacemaker, generating electrical impulses at a regular rate. These impulses spread through the atria, causing them to contract. The AV node then delays the impulse before transmitting it to the ventricles.
The bundle of His and Purkinje fibers ensure rapid and coordinated ventricular contraction. This sequence is crucial for efficient blood pumping.
Abnormal Electrical Activity Leading to Arrhythmias
Deviations from this normal electrical pathway can lead to various arrhythmias. These irregularities can stem from several factors, including:
- Problems with the generation or conduction of electrical signals. For example, a malfunctioning SA node may generate impulses at an abnormally slow or fast rate, resulting in bradycardia or tachycardia, respectively.
- Structural damage to the heart muscle, such as from a heart attack. Scar tissue can disrupt normal electrical conduction pathways, leading to reentrant circuits and other arrhythmias.
- Electrolyte imbalances, such as low potassium or magnesium levels, can interfere with the electrical activity of the heart cells.
- Certain medications can also affect the heart’s electrical activity, either directly or indirectly.
Types of Arrhythmias and Electrical Patterns
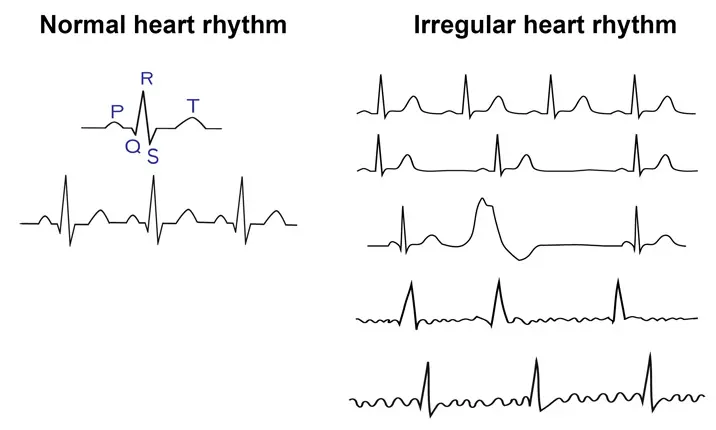
Different types of arrhythmias exhibit distinct electrical patterns. These patterns are analyzed through electrocardiograms (ECGs), which measure the electrical activity of the heart over time.
- Bradycardia: characterized by a slow heart rate. The ECG would show prolonged intervals between the electrical impulses.
- Tachycardia: characterized by a rapid heart rate. The ECG would show short intervals between the electrical impulses.
- Atrial Fibrillation (AFib): occurs when the atria quiver rather than contract in a coordinated manner. The ECG shows irregular, rapid, and chaotic electrical activity in the atria.
- Ventricular Fibrillation (VFib): a life-threatening arrhythmia where the ventricles quiver and do not contract effectively. The ECG exhibits a chaotic, disorganized pattern.
Examples of Common Arrhythmias and Electrical Patterns
- Sinus Tachycardia: a common, often benign, rapid heart rate originating from the SA node. The ECG shows a regular, rapid rhythm with normal P waves.
- Premature Ventricular Contractions (PVCs): extra heartbeats originating from the ventricles. The ECG shows an extra, often wide and distorted, QRS complex.
Circular Patterns in Arrhythmias
Circular patterns of electrical activity in the heart, often referred to as reentrant circuits, are a crucial aspect of understanding certain types of arrhythmias. These patterns involve the repetitive firing of electrical impulses within a closed loop of cardiac tissue, leading to sustained abnormal heart rhythms. The characteristics of these patterns, their manifestation on electrocardiograms (ECGs), and the underlying mechanisms are pivotal to diagnosis and treatment.Circular electrical patterns in the heart are characterized by a continuous, repetitive activation wave traveling in a closed loop, resulting in repetitive, often regular, arrhythmic heartbeats.
These patterns differ from other arrhythmias by their specific propagation pathways and the manner in which they are visualized on an ECG.
Characteristics of Circular Electrical Patterns
Circular electrical patterns in the heart involve a specific pathway of electrical activation that continually loops back on itself. This loop creates a self-sustaining circuit, leading to a repeating pattern of electrical activity. The speed of this loop, and the duration of the repetitive activation, significantly influence the heart rate during the arrhythmia.
Manifestation in Electrocardiograms (ECGs)
Circular patterns manifest on ECGs in distinct ways, depending on the specific location of the loop and the direction of the electrical activation within it. The ECG will show characteristic patterns that repeat in a regular, often predictable, manner. These patterns may exhibit a specific morphology (shape) that can help differentiate from other arrhythmias.
Mechanisms Causing Circular Patterns
Circular patterns arise from various mechanisms, most commonly involving a combination of factors such as slow conduction in certain areas of the heart, and/or the presence of an accessory pathway. These factors can create a situation where the electrical impulse cannot completely depolarize a portion of the heart, thus generating a “reentry” circuit.
Understanding the circular pattern of electrical activity in arrhythmias is crucial for diagnosis and treatment. Proper footwear support is also key for maintaining overall health, especially for individuals with flat feet, choosing the right running shoes can make a significant difference. Consider the best running shoes for flat feet to support your feet and help prevent issues like discomfort or worsening of underlying conditions, which can ultimately impact the electrical activity patterns within the heart.
This connection between foot health and cardiac health highlights the importance of comprehensive care in maintaining a healthy lifestyle.
Implications on Heart Function
The presence of circular patterns significantly impacts heart function. Depending on the location and speed of the circular pathway, the heart rate can be abnormally fast or slow. In severe cases, the heart may not be able to effectively pump blood throughout the body, leading to potentially life-threatening complications. The sustained nature of the circular pattern can lead to decreased cardiac output and reduced blood flow to vital organs.
Comparison with Other Arrhythmia Patterns
Circular patterns differ from other arrhythmia patterns by their specific characteristics on the ECG. For example, atrial fibrillation exhibits irregular, chaotic electrical activity, while ventricular tachycardia may manifest as wide, complex QRS complexes. Differentiating these patterns is crucial for proper diagnosis and treatment.
Examples of ECG Recordings
A precise representation of ECG recordings showcasing circular patterns is not possible within this text format. However, understanding the general features is important. A key feature is the repetitive nature of the pattern, a repeating shape and timing of the waves. Further investigation, including specialized analyses, is required to definitively identify the presence of a circular pattern.
These recordings often exhibit a particular morphology, with repetitive patterns that may not be present in other arrhythmias. Clinical observation and further investigation are crucial for proper interpretation.
Understanding the circular pattern of electrical activity in arrhythmia can be fascinating, but it’s also important to consider how lifestyle choices can impact our health. For instance, consistent eating habits, like only eating during the daytime, can significantly influence blood sugar levels, which is crucial for managing type 2 diabetes. This concept, explored further in how eating only in the daytime can help people with type 2 diabetes , could potentially have a ripple effect on other aspects of our physiological processes, ultimately affecting the electrical activity in our hearts and the potential for arrhythmias.
A deeper dive into these connections is still needed to fully grasp the intricate interplay between diet and cardiac health, but it’s a fascinating area of research.
ECG Interpretation of Circular Patterns
ECG interpretation plays a crucial role in diagnosing and managing arrhythmias. Identifying circular patterns in ECGs, indicative of specific arrhythmias, requires meticulous analysis of waveform characteristics, durations, and lead involvement. A thorough understanding of the steps involved in ECG interpretation, coupled with knowledge of specific leads useful for identifying these patterns, is essential for accurate diagnosis and treatment.
ECG Interpretation Steps
Accurate ECG interpretation involves a systematic approach. First, assess the rhythm: is it regular or irregular? Second, analyze the rate: is it within the normal range or outside it? Third, evaluate the morphology of the P waves, QRS complexes, and T waves. Fourth, determine the presence and characteristics of any arrhythmias.
These steps are crucial for recognizing the subtle changes indicative of circular patterns.
Identifying Circular Patterns on an ECG
Circular patterns on an ECG represent repetitive electrical activity within a closed loop. These patterns manifest as recurring, consistent changes in the ECG waveforms across multiple leads. Visualizing the pattern requires a keen eye for detail. Notice recurring waveform shapes and durations in the ECG leads. The repeating nature of the pattern is a key identifier.
ECG Leads for Identifying Circular Patterns
Several ECG leads are particularly useful for identifying circular patterns. Leads that encompass the area of the heart exhibiting the circular activity are often critical. Leads V1 through V6, which directly view the depolarization and repolarization of the ventricles, are valuable. Precordial leads (V1-V6) and limb leads (I, II, III, aVR, aVL, aVF) can provide crucial information.
The specific leads useful will depend on the precise location of the circular activity within the heart.
Measuring Duration of Circular Patterns
Measuring the duration of circular patterns involves calculating the time interval between successive occurrences of the characteristic waveforms. Use the time axis on the ECG tracing to accurately determine the intervals. This measurement helps determine the frequency and periodicity of the circular pattern, providing insights into the underlying electrical activity.
Comparison of Circular Patterns
| ECG Lead | Waveform Shape | Duration (ms) | Clinical Significance |
|---|---|---|---|
| V1-V6 | Repeated sawtooth or U-shaped waves | Variable, typically 100-400 ms | Possible Atrial Flutter |
| I, II, III | Repeated sawtooth or U-shaped waves | Variable, typically 100-400 ms | Possible Atrial Flutter |
| V1-V6 | Alternating positive and negative deflections | Variable, typically 200-600 ms | Possible Ventricular Tachycardia |
| I, II, III | Alternating positive and negative deflections | Variable, typically 200-600 ms | Possible Ventricular Tachycardia |
This table provides a general overview. Specific waveform characteristics and durations may vary depending on the individual case and the type of circular pattern. Detailed analysis of the pattern in multiple leads is crucial for accurate diagnosis.
Examples of Circular Patterns and Their ECG Features
A key example of a circular pattern is atrial flutter. In atrial flutter, the atria depolarize at a rapid, regular rate, often creating a characteristic “sawtooth” pattern in the ECG. This rapid depolarization creates a repeating pattern in the ECG tracing. Ventricular tachycardia is another example. In this case, a consistent, repeating pattern in the ventricular depolarization can be observed.
This repeated pattern in the ECG waveform is crucial for diagnosis.
Clinical Significance of Circular Patterns
Circular patterns in electrocardiograms (ECGs) represent a crucial diagnostic indicator, signaling potentially life-threatening arrhythmias. Understanding these patterns’ clinical implications, risk factors, and potential consequences is paramount for timely intervention and patient management. Early detection allows for prompt treatment, reducing the risk of severe complications.Detecting these patterns in ECGs allows for rapid and precise diagnosis of specific arrhythmias, enabling clinicians to implement targeted therapies.
This accurate assessment is essential for predicting the likelihood of adverse events and for tailoring the most effective treatment strategies.
Clinical Implications of Circular Patterns
Circular patterns on ECGs are strong indicators of complex and often serious cardiac conditions. They frequently signify reentrant arrhythmias, where electrical impulses circulate in a closed loop within the heart. This can lead to various potentially dangerous consequences, from palpitations to sudden cardiac arrest. The specific clinical implications are dependent on the type of circular pattern, the speed of the circuit, and the underlying heart conditions.
Risk Factors Associated with Circular Patterns
Several factors can contribute to the emergence of circular patterns in ECGs. These include pre-existing heart conditions like coronary artery disease, cardiomyopathy, and congenital heart defects. Electrolyte imbalances, medications, and certain metabolic disorders can also increase the risk. Lifestyle factors such as smoking, excessive alcohol consumption, and a lack of physical activity can also contribute to an increased risk of arrhythmias.
Potential Consequences of Circular Patterns
Circular patterns can lead to a range of adverse consequences, depending on the specific arrhythmia and the patient’s overall health. Mild cases may present as palpitations or dizziness, while more severe cases can result in syncope (fainting), loss of consciousness, and potentially fatal cardiac arrest. The rapid and irregular electrical activity can disrupt the heart’s ability to pump blood effectively, leading to organ damage and decreased quality of life.
Examples of Situations Where Circular Patterns Are Crucial for Diagnosis
Circular patterns are crucial for diagnosing specific arrhythmias, such as atrial flutter and ventricular tachycardia. In atrial flutter, a circular pattern indicates rapid, repetitive electrical impulses within the atria, leading to a characteristic “sawtooth” pattern in the ECG. Similarly, ventricular tachycardia involves a circular pattern in the ventricles, often characterized by a rapid and irregular heart rate. Early detection of these patterns is vital for prompt intervention and prevention of complications.
Role of Circular Patterns in Classifying Severity of Arrhythmias
The characteristics of circular patterns, such as the rate and regularity of the electrical activity, can help in classifying the severity of the arrhythmia. Patterns with faster rates and less regular activity are often associated with more severe arrhythmias and a higher risk of complications. Detailed analysis of the ECG and patient history is crucial in determining the appropriate level of urgency and the most effective treatment strategy.
Categorization of Circular Patterns by Risk Level and Potential Complications, Arrhythmia electrical activity circular pattern
| Risk Level | Characteristics | Potential Complications |
|---|---|---|
| Low | Slow, regular circular pattern; infrequent occurrence | Palpitations, mild dizziness |
| Medium | Moderate rate, intermittent irregularity; presence of underlying heart conditions | Syncope, chest pain, shortness of breath |
| High | Rapid, irregular circular pattern; associated with significant underlying cardiac issues | Cardiac arrest, loss of consciousness, organ damage |
Treatment Strategies for Arrhythmias with Circular Patterns
Treating arrhythmias characterized by circular patterns in electrical activity necessitates a multifaceted approach. The goal is to restore normal sinus rhythm and prevent potentially life-threatening complications. Successful treatment hinges on careful evaluation of the specific arrhythmia, its underlying cause, and the patient’s overall health. A personalized strategy, often incorporating multiple interventions, is frequently required.
Medication Management
Pharmacological interventions play a crucial role in managing arrhythmias with circular patterns. These medications aim to modify the electrical properties of the heart, either by slowing conduction, enhancing repolarization, or suppressing abnormal impulses. Different medications target various aspects of the electrical cycle.
- Beta-blockers, such as metoprolol and atenolol, reduce heart rate and contractility, which can be helpful in slowing down the circular patterns. Their efficacy depends on the specific arrhythmia and patient response.
- Calcium channel blockers, like verapamil and diltiazem, can also decrease heart rate and conduction velocity. They may be particularly effective in certain types of circular arrhythmias.
- Antiarrhythmic agents, including amiodarone and sotalol, directly affect the electrical activity of the heart. They can interrupt the circular pathways and restore normal rhythm. However, these agents can have potential side effects and are often used with caution.
Electrical Procedures
In some cases, medications alone may not be sufficient to control the arrhythmia. Electrical procedures are designed to correct the underlying electrical abnormalities.
- Catheter ablation involves inserting catheters into the heart via blood vessels. These catheters deliver radiofrequency energy to specific areas of the heart that are causing the circular pattern. This procedure effectively eliminates the abnormal electrical pathways.
- Implantable cardioverter-defibrillators (ICDs) are devices that monitor the heart’s rhythm. If the heart rate falls outside a safe range, the ICD delivers an electrical shock to restore normal rhythm. ICDs are crucial in preventing potentially fatal ventricular arrhythmias.
Successful Treatment Outcomes
Numerous patients with circular arrhythmias have experienced significant improvements in their quality of life following successful treatment. Examples include patients who were previously experiencing frequent episodes of palpitations, lightheadedness, or syncope. After undergoing catheter ablation, these symptoms were significantly reduced or eliminated. The restoration of normal heart rhythm allows for increased physical activity and improved overall well-being.
Continuous Monitoring and Follow-up
Post-treatment, continuous monitoring is essential to assess the effectiveness of the interventions and identify any recurrence of the arrhythmia. Regular electrocardiograms (ECGs) and Holter monitoring are often employed. Early detection of any recurrence allows for timely intervention to prevent complications. Patients need to be educated on recognizing and reporting any new symptoms, such as palpitations or dizziness.
Treatment Strategies Table
| Treatment Strategy | Pros | Cons |
|---|---|---|
| Medication Management | Generally less invasive, potentially effective for some cases, easier to administer | May not be effective for all patients, potential side effects, may require multiple medications, less predictable outcomes |
| Electrical Procedures (Catheter Ablation) | Potentially curative, effective for specific types of arrhythmias, often leads to long-term resolution | More invasive procedure, potential complications (bleeding, infection), higher cost, not suitable for all cases |
| Implantable Cardioverter-Defibrillators (ICDs) | Provides life-saving intervention for high-risk patients, detects and corrects potentially fatal arrhythmias | Requires device implantation, potential for device-related complications, potential for inappropriate shocks, lifelong commitment to device management |
Illustrative Cases: Arrhythmia Electrical Activity Circular Pattern
Understanding arrhythmias with circular patterns requires a practical approach. Illustrative cases help solidify the theoretical concepts by showcasing real-world scenarios. The following examples detail the symptoms, ECG findings, diagnosis, treatment, and outcomes associated with such arrhythmias. This practical application enhances the understanding of the clinical implications and management strategies.
Hypothetical Case 1: Atrial Flutter with Variable Conduction
Atrial flutter with variable conduction is a common arrhythmia characterized by a rapid, regular atrial rhythm with a variable degree of AV nodal block. This variability in conduction can lead to a circular pattern on the ECG, presenting as fluctuating R-R intervals.
- Patient Symptoms: A 65-year-old male patient presented with palpitations, lightheadedness, and mild shortness of breath. These symptoms were intermittent, lasting for several minutes at a time.
- ECG Findings: The ECG revealed a regular atrial rhythm at a rate of approximately 300 bpm, with characteristic “sawtooth” waves in the atrial leads. Variable conduction was evident by irregular ventricular responses. The R-R intervals showed fluctuations, creating a circular pattern on the ECG.
- Diagnosis: Atrial flutter with variable conduction was suspected based on the ECG findings, including the sawtooth waves and irregular ventricular response. Further diagnostic testing, such as a Holter monitor, may have been used to confirm the diagnosis.
- Treatment: The patient was initially treated with intravenous adenosine, which effectively slowed the ventricular rate. Following this, a beta-blocker was prescribed to control the atrial rate and prevent recurrence. Further treatment options, such as catheter ablation, might have been considered.
- Outcome: The patient responded well to treatment. Palpitations and symptoms subsided. The patient remained asymptomatic with regular follow-up visits and continued medication.
Hypothetical Case 2: Wandering Pacemaker
A wandering pacemaker is an arrhythmia where the impulse for ventricular contraction originates from different sites in the heart. This can result in a cyclical pattern of P waves, with varying P-R intervals and QRS complexes.
- Patient Symptoms: A 40-year-old female patient complained of intermittent palpitations, a feeling of a rapid heartbeat, and dizziness. These symptoms were more pronounced during periods of exertion.
- ECG Findings: The ECG showed an irregular rhythm with variable P wave morphology and PR intervals. The QRS complexes also exhibited variations in shape and duration, illustrating a wandering pacemaker pattern.
- Diagnosis: The ECG pattern was suggestive of a wandering pacemaker, and further investigation, such as a Holter monitor, may have been performed to assess the duration and frequency of the arrhythmia. Electrophysiological studies might be necessary to confirm the diagnosis.
- Treatment: Management primarily involved addressing the underlying cause of the wandering pacemaker. If no specific cause was identified, medications to control the heart rate and rhythm were considered. In certain cases, catheter ablation could be an option.
- Outcome: The patient’s symptoms improved with the administration of medications, and regular follow-up visits maintained the patient’s stable condition. The wandering pacemaker subsided, with the patient experiencing minimal or no symptoms.
Summary Table of Illustrative Cases
| Patient Symptoms | ECG Findings | Diagnosis | Treatment | Outcome |
|---|---|---|---|---|
| Palpitations, lightheadedness, mild shortness of breath | Regular atrial rhythm (300 bpm), sawtooth waves, variable ventricular response | Atrial flutter with variable conduction | Adenosine, beta-blocker, catheter ablation (possible) | Symptomatic relief, stable condition |
| Intermittent palpitations, rapid heartbeat, dizziness, worse with exertion | Irregular rhythm, variable P wave morphology, PR intervals, and QRS complexes | Wandering pacemaker | Medications to control heart rate and rhythm, catheter ablation (possible) | Symptom improvement, stable condition |
Monitoring and Prevention
Staying vigilant and proactive is crucial for managing arrhythmias with circular patterns. Proactive monitoring and lifestyle adjustments can significantly reduce the risk of recurrence and improve overall well-being. Early detection and intervention can help prevent potentially serious complications.Effective management involves a multi-faceted approach, combining close monitoring, lifestyle modifications, and medical interventions. Understanding the triggers and risk factors is essential for developing personalized prevention strategies.
Methods of Monitoring Patients
Continuous cardiac monitoring is a critical component of managing patients with a history of arrhythmias exhibiting circular patterns. This allows for real-time detection of any abnormalities. Several methods are available, each with its own advantages and limitations.Electrocardiograms (ECGs) remain a cornerstone of monitoring. Regular ECGs allow healthcare professionals to identify any changes in heart rhythm, including the characteristic circular patterns.
Holter monitors provide continuous ECG recordings over 24 hours or longer, offering a more comprehensive picture of the patient’s heart activity throughout the day. Implantable loop recorders (ILRs) offer extended monitoring, recording heart activity for several months, enabling detection of infrequent or intermittent arrhythmias. Event recorders are used for capturing episodes of arrhythmia when they occur. These devices are triggered by the patient when they experience symptoms, providing a snapshot of the heart’s electrical activity during the event.
Lifestyle Factors Contributing to Circular Patterns
Several lifestyle factors can contribute to the development and recurrence of arrhythmias with circular patterns. These factors can interact with genetic predispositions and underlying heart conditions to increase the risk of these patterns.Unhealthy dietary habits, including excessive intake of saturated fats and sodium, can increase strain on the cardiovascular system. Lack of regular physical activity can weaken the heart muscle and increase the risk of arrhythmias.
Smoking, excessive alcohol consumption, and stress can all negatively impact heart health, potentially contributing to the development of circular patterns. Sleep deprivation can also disrupt the body’s natural rhythm, increasing the risk of cardiac irregularities. Medications, including some over-the-counter drugs, can sometimes trigger or worsen arrhythmias.
Preventive Measures to Reduce Recurrence
Implementing preventive measures is key to reducing the risk of recurrent arrhythmias. These strategies aim to mitigate the identified risk factors and support overall cardiovascular health.A balanced diet rich in fruits, vegetables, and whole grains, along with regular exercise, can help maintain a healthy weight and cardiovascular function. Limiting alcohol consumption and avoiding smoking are crucial steps in minimizing cardiovascular stress.
Stress management techniques, such as yoga, meditation, or deep breathing exercises, can help regulate the body’s response to stress. Getting adequate sleep and managing any underlying medical conditions are essential components of a comprehensive prevention strategy.
Importance of Regular Checkups and Screenings
Regular checkups and screenings are crucial for early detection and management of arrhythmias. These appointments allow healthcare providers to monitor the patient’s condition, identify any changes, and adjust treatment plans as needed. Proactive screening helps in identifying potential risks and enabling early intervention.Regular checkups and screenings help in maintaining a healthy cardiovascular system. By identifying and addressing potential problems early, the risk of developing serious complications is minimized.
The frequency of checkups will vary depending on the individual’s risk factors and the severity of their condition. Monitoring and adjustments are essential for successful management of arrhythmias.
Lifestyle Modifications for Prevention
Implementing these lifestyle modifications can contribute significantly to preventing the recurrence of circular patterns.
- Balanced Diet: A diet rich in fruits, vegetables, and whole grains, and low in saturated fats and sodium, can support heart health. Example: The Mediterranean diet, rich in fresh produce and healthy fats, has shown positive effects on cardiovascular health.
- Regular Exercise: Engaging in regular physical activity strengthens the heart and improves overall cardiovascular health. Example: Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week.
- Stress Management: Incorporating stress-reducing techniques, such as yoga, meditation, or deep breathing exercises, can help regulate the body’s response to stress. Example: Daily meditation can help manage stress and improve sleep quality.
- Adequate Sleep: Prioritizing sufficient sleep (7-8 hours per night) is crucial for the body’s restorative processes and cardiovascular health. Example: Maintaining a regular sleep schedule and creating a relaxing bedtime routine can promote better sleep quality.
- Avoidance of Smoking and Excessive Alcohol: These habits can significantly increase the risk of heart problems and arrhythmias. Example: Stopping smoking can lead to a noticeable improvement in cardiovascular health.
Final Review
In conclusion, arrhythmia electrical activity circular patterns represent a significant aspect of cardiac electrophysiology. Understanding their characteristics, mechanisms, and clinical implications is vital for accurate diagnosis and effective treatment. This comprehensive overview provides a framework for grasping the intricacies of circular patterns in arrhythmias, highlighting the importance of ECG interpretation, treatment strategies, and patient monitoring. The illustrative cases further emphasize the clinical relevance of these patterns.
