Ask dmine diabetes beta cell resurrection explores the groundbreaking potential to restore beta cells, the insulin-producing cells destroyed in diabetes. This in-depth look delves into the complexities of beta cell regeneration, examining various approaches, from stem cell therapies to gene editing, and considering the ethical and practical implications of this revolutionary field.
We’ll delve into the intricate mechanisms of beta cell destruction in different types of diabetes, and analyze the effectiveness, safety, and feasibility of current and emerging regeneration techniques. This includes a critical assessment of the hurdles and obstacles, and a forward-looking exploration of future research directions.
Defining Beta Cell Resurrection
Beta cell resurrection, a promising frontier in diabetes research, aims to regenerate or restore functional beta cells in individuals with diabetes. This process seeks to replace the damaged or lost beta cells that are responsible for insulin production, thereby potentially offering a cure or a significant improvement in blood sugar control. The underlying principle is to either stimulate the body’s own repair mechanisms or to introduce new beta cells to compensate for the deficiency.
The long-term goal is to alleviate the burden of diabetes and its complications.The concept hinges on the ability to induce the body’s natural regenerative processes or to develop an alternative source of functional beta cells. This can involve using various approaches, including stem cell therapy, gene therapy, and immunomodulation, to either promote the growth of new beta cells or enhance the function of existing ones.
The focus is on creating a sustainable source of insulin production. This method is an alternative to insulin therapy, which is currently the mainstay treatment for diabetes.
Approaches to Beta Cell Regeneration
Various strategies are being explored to achieve beta cell resurrection. These methods focus on different aspects of beta cell development, function, and survival. Stem cell therapy, for instance, utilizes pluripotent stem cells (PSCs) to differentiate into beta cells. Gene therapy, on the other hand, targets specific genes involved in beta cell function and development.
Stem Cell Therapy
Stem cell therapy holds considerable promise for beta cell regeneration. It involves isolating and differentiating pluripotent stem cells, such as induced pluripotent stem cells (iPSCs), into insulin-producing beta cells. The process of differentiation is crucial, as these cells must acquire the specific characteristics necessary for proper insulin secretion. Further research is focused on developing protocols for efficient and safe differentiation.
Successes have been seen in animal models, demonstrating the potential of this approach, although challenges remain in translating these findings to human applications.
Gene Therapy
Gene therapy involves modifying the genetic makeup of cells to enhance their function. In the context of beta cell regeneration, gene therapy can be used to correct genetic defects that contribute to beta cell dysfunction or to introduce genes that promote beta cell growth and survival. Scientists are investigating the delivery of therapeutic genes into beta cells and are focusing on minimizing potential side effects.
Successes in animal models show that introducing genes that promote insulin production and growth can be beneficial. Challenges remain in ensuring the long-term stability and efficacy of gene therapy interventions.
Immunomodulation
Immunomodulation strategies aim to mitigate the autoimmune response that often destroys beta cells in type 1 diabetes. This approach seeks to modulate the immune system to prevent or reduce the attack on beta cells. Immunosuppressive drugs or other immunomodulatory therapies can potentially prevent or slow the progression of beta cell destruction, allowing for regeneration to occur.
Current Research Efforts
Significant research is being conducted globally to investigate the efficacy and safety of various beta cell regeneration approaches. Researchers are focusing on optimizing protocols, improving differentiation efficiency, and developing methods for efficient delivery of therapeutic agents. Some ongoing efforts are focused on creating a better understanding of beta cell biology and development, with a goal of identifying critical factors influencing beta cell regeneration.
Obstacles and Challenges
Several obstacles hinder the progress of beta cell resurrection. One major challenge is the complexity of beta cell development and function. Ensuring that the regenerated beta cells integrate properly into the existing islet structure is also a key concern. Furthermore, maintaining the long-term function of these regenerated beta cells is essential. Immune responses and ethical considerations are also significant factors to address.
Types of Diabetes and Relevance
The relevance of beta cell resurrection varies depending on the type of diabetes. Type 1 diabetes, an autoimmune disease, is characterized by the complete destruction of beta cells. Beta cell resurrection holds significant promise in type 1 diabetes, potentially offering a cure or a substantial improvement in glycemic control. Type 2 diabetes, characterized by insulin resistance and progressive beta cell dysfunction, may also benefit from beta cell regeneration strategies.
The approach may be more effective in the earlier stages of type 2 diabetes, where beta cell function is still partially preserved. Preclinical studies show that beta cell regeneration can improve blood sugar control in animal models with type 2 diabetes. This highlights the potential for beta cell resurrection to be a valuable therapeutic tool in both type 1 and type 2 diabetes.
Methods of Beta Cell Regeneration
Regenerating beta cells, the insulin-producing cells in the pancreas, is a crucial goal in the fight against type 1 and type 2 diabetes. Various approaches are being explored, each with its own set of advantages and disadvantages. This journey to restore insulin production involves diverse strategies, from transplanting existing cells to manipulating stem cells and even modifying genes.
The ethical considerations associated with these methods must also be carefully weighed.
Cell Replacement Therapies
Cell replacement therapy involves transplanting healthy beta cells into the pancreas of individuals with damaged or insufficient beta cells. This approach aims to restore insulin production and, consequently, glucose homeostasis. This method has shown promise in preclinical studies, but challenges remain in achieving long-term functionality and preventing immune rejection of the transplanted cells. Current research focuses on improving cell survival and function post-transplantation, and minimizing immune responses.
Stem Cell-Based Approaches
Stem cell-based therapies offer a promising alternative to cell replacement. Stem cells, particularly pluripotent stem cells, have the potential to differentiate into various cell types, including beta cells. This approach avoids the need for donor cells, potentially reducing the risk of rejection. However, the efficient and consistent differentiation of stem cells into functional beta cells remains a significant hurdle.
Challenges include optimizing differentiation protocols and ensuring the long-term functionality of the generated beta cells.
I’ve been diving deep into the fascinating world of ask dmine diabetes beta cell resurrection lately, and it’s truly mind-blowing. While researching, I stumbled upon a very alarming article about a new, drug-resistant fungus, which is definitely something we need to be aware of. Everything you need to know about the new deadly drug resistant fungus is crucial reading for anyone interested in the latest advancements in medical research.
Hopefully, this new knowledge will help propel us closer to the exciting prospect of beta cell resurrection for diabetes patients.
Gene Therapy
Gene therapy aims to directly modify the genes within the beta cells to improve their function. This could involve correcting genetic defects that lead to beta cell dysfunction or enhancing the production of insulin. Early research has shown some success in preclinical models. However, the safety and efficacy of gene therapy remain major concerns, as unintended genetic alterations could have unforeseen consequences.
Ethical considerations surrounding germline modification are particularly significant.
Comparison of Methods
| Method | Effectiveness | Cost | Side Effects |
|---|---|---|---|
| Cell Replacement Therapy | Potentially effective, but long-term function and immune rejection are challenges. | Relatively high due to specialized procedures and potential need for immunosuppressants. | Risk of immune rejection, potential for tumor formation if cells are not carefully selected, and the need for ongoing immunosuppression. |
| Stem Cell Approaches | High potential for avoiding rejection issues, but consistent differentiation into functional beta cells is a major hurdle. | Moderately high, as stem cell research and cultivation require specialized facilities and expertise. | Risk of tumor formation, potential immune responses, and ethical concerns related to the use of embryonic stem cells. |
| Gene Therapy | Theoretically high potential, but safety concerns regarding unintended genetic modifications are significant. | High, as gene therapy techniques are complex and require specialized expertise and facilities. | Risk of insertional mutagenesis (inserting the gene into an incorrect location in the genome and causing unwanted effects), potential immune responses, and ethical concerns surrounding germline modification. |
Ethical Considerations
The ethical considerations surrounding beta cell regeneration methods are multifaceted. Issues surrounding the use of embryonic stem cells, the potential for germline modifications, and the equitable access to these therapies need careful consideration. Discussions about informed consent, potential risks, and societal impact are critical for responsible development and implementation of these therapies.
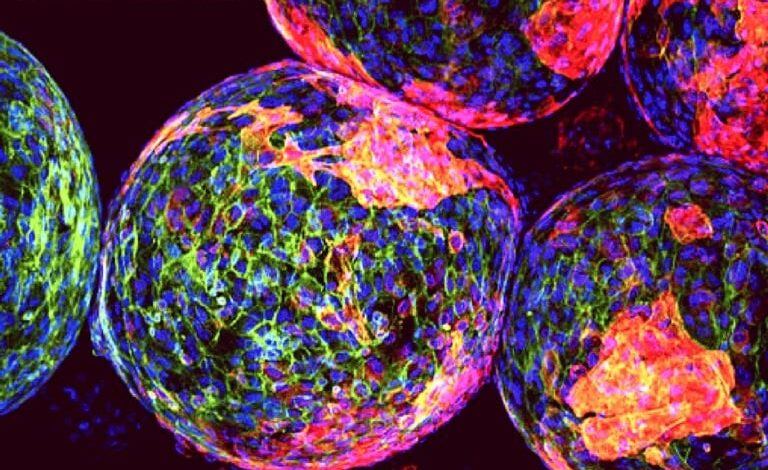
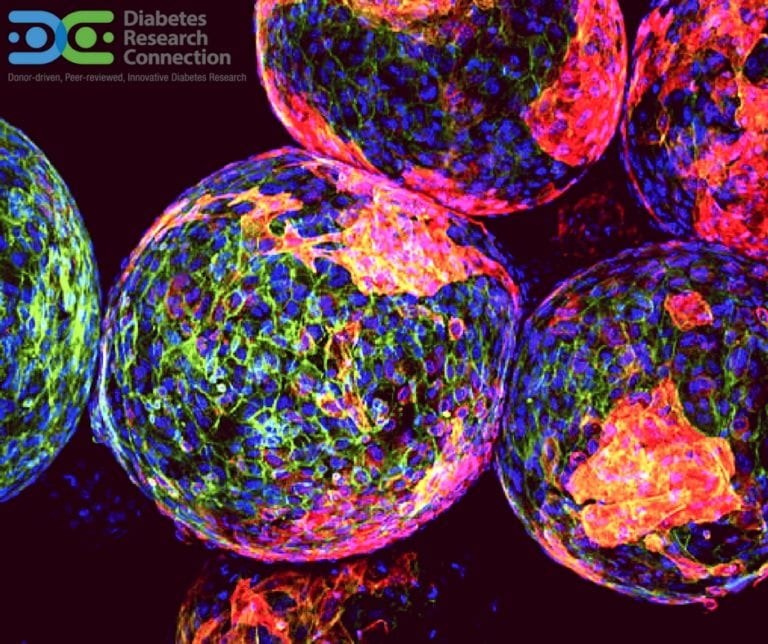
Stem Cell Research and Diabetes: Ask Dmine Diabetes Beta Cell Resurrection

Stem cell research holds immense promise for treating diabetes, particularly Type 1, by potentially regenerating the insulin-producing beta cells in the pancreas. This innovative approach offers a potential cure or significantly improved management strategy for millions affected by this chronic condition. The ability to harness the regenerative power of stem cells could revolutionize diabetes care.Stem cells are undifferentiated cells with the remarkable capacity to develop into various cell types within the body.
Researchers are actively exploring their use in regenerating damaged beta cells, offering a potential pathway to restoring normal blood sugar regulation. This approach circumvents the need for lifelong insulin injections, potentially leading to a more sustainable and natural form of treatment.
Types of Stem Cells Used in Beta Cell Regeneration
Different types of stem cells are being investigated for their potential in beta cell regeneration. These include embryonic stem cells, induced pluripotent stem cells (iPSCs), and mesenchymal stem cells. Each type possesses unique characteristics and advantages, influencing the research directions and strategies for beta cell regeneration.
- Embryonic Stem Cells (ESCs): ESCs are derived from the inner cell mass of a blastocyst, an early-stage embryo. They exhibit the remarkable capacity to differentiate into various cell types, including beta cells. However, ethical concerns surrounding their use and the risk of immune rejection in transplant recipients have limited their widespread application in clinical settings.
- Induced Pluripotent Stem Cells (iPSCs): iPSCs are adult cells that have been reprogrammed to a pluripotent state, mimicking the characteristics of embryonic stem cells. This approach overcomes the ethical concerns associated with ESCs and offers a more readily accessible source of stem cells. The potential for creating patient-specific iPSCs further enhances the prospect of personalized treatments for diabetes.
- Mesenchymal Stem Cells (MSCs): MSCs are multipotent adult stem cells found in various tissues, including bone marrow. They possess the ability to differentiate into multiple cell types, although with a limited potential compared to ESCs or iPSCs. Their use in diabetes research is often focused on paracrine effects, where they stimulate beta cell regeneration or function rather than direct differentiation.
Procedures for Stem Cell Isolation, Differentiation, and Implantation
The process of using stem cells for beta cell regeneration involves several key steps. These steps include isolating the desired stem cells, differentiating them into beta-like cells, and finally, implanting them into the patient’s pancreas.
- Isolation: The initial step involves isolating the chosen stem cell type from a suitable source. This may involve extracting cells from bone marrow, adipose tissue, or other sources, followed by appropriate culture conditions to promote cell growth.
- Differentiation: The isolated stem cells are then coaxed to differentiate into beta-like cells. This process typically involves exposing the cells to specific growth factors, signaling molecules, and environmental conditions in laboratory settings. Sophisticated bioreactors are often employed to optimize the differentiation process and improve efficiency.
- Implantation: Once the beta-like cells have been successfully generated, they are ready for transplantation into the patient’s pancreas. The exact implantation procedure may vary depending on the specific approach and the individual patient’s condition. Minimally invasive surgical techniques are generally favored to reduce complications.
Potential of iPSCs for Beta Cell Regeneration
Induced pluripotent stem cells (iPSCs) offer a significant advancement in stem cell-based therapies for diabetes. The ability to generate patient-specific iPSCs holds immense promise for personalized medicine, allowing for the development of treatments tailored to individual needs.
- Personalized Treatments: iPSCs derived from a patient’s own cells can be used to create beta-like cells with a reduced risk of immune rejection. This personalized approach offers a potentially more effective and safer treatment option.
- Reduced Ethical Concerns: The use of iPSCs avoids the ethical concerns associated with embryonic stem cells, as they are derived from the patient’s own cells.
- Advancements in iPSC technology: Continuous advancements in iPSC technology are refining the protocols for generating functional beta cells. These improvements are enhancing the efficiency and quality of beta cell production, paving the way for wider clinical applications.
Latest Advancements in Stem Cell Research
Recent breakthroughs in stem cell research have significantly improved the efficiency and effectiveness of beta cell regeneration. The development of novel differentiation protocols and the use of bioengineered scaffolds have yielded encouraging results in preclinical studies.
- Novel Differentiation Protocols: Improved differentiation protocols are increasing the yield of functional beta-like cells, leading to better treatment outcomes.
- Bioengineered Scaffolds: Bioengineered scaffolds that mimic the native pancreatic microenvironment have shown promise in supporting the survival and function of implanted beta cells.
Immunological Considerations
The immune system, a complex network of cells and proteins, plays a crucial role in maintaining bodily health. In the context of diabetes, the immune system can paradoxically be both a protector and a destroyer. Its ability to distinguish self from non-self is paramount for preventing autoimmune diseases like type 1 diabetes, where the immune system mistakenly targets and destroys insulin-producing beta cells in the pancreas.
The successful transplantation of beta cells, or other tissues for that matter, faces a significant hurdle: the potential for immune rejection. Strategies to mitigate this risk are vital for the long-term success of beta cell resurrection therapies.Understanding the intricate interplay between the immune system and beta cell destruction is key to developing effective therapies. This involves deciphering the specific immune mechanisms involved in beta cell damage, identifying the key players in the immune response, and eventually, developing targeted interventions to control or redirect these responses.
This understanding is essential for preventing the body from attacking the transplanted beta cells, ensuring their long-term survival.
I’ve been fascinated by the research into asking dmine about diabetes beta cell resurrection lately. It’s a complex area, and while there’s still a long way to go, the potential is incredible. The recent news about the Zika virus not spreading widely in the US, as detailed in this article on zika wont travel far in usa , highlights how different diseases impact our health, and how understanding these patterns can inform our approach to tackling similar health challenges, like the quest for beta cell resurrection in diabetes.
Ultimately, I’m hopeful that breakthroughs in areas like asking dmine diabetes beta cell resurrection will lead to improved treatments and cures for various conditions.
Role of the Immune System in Beta Cell Destruction
The immune system’s attack on beta cells in type 1 diabetes is a complex process involving various cell types, including T cells, B cells, and macrophages. Autoreactive T cells, recognizing beta cell components as foreign, initiate a cascade of inflammatory responses, ultimately leading to beta cell destruction. Furthermore, autoantibodies produced by B cells contribute to the damage. The specific mechanisms behind this autoimmune response are still being researched, but it’s a crucial area for understanding the disease and developing effective therapies.
Strategies to Mitigate Immune Rejection
Immunosuppressive strategies aim to dampen the immune response, reducing the risk of rejection after beta cell transplantation. These strategies target different components of the immune system to achieve this.
- Immunosuppressive Medications: A wide array of immunosuppressive drugs, such as corticosteroids, calcineurin inhibitors (like cyclosporine and tacrolimus), and anti-metabolites (like azathioprine and mycophenolate mofetil), are commonly used to suppress the immune system after transplantation. These drugs work by inhibiting various immune pathways. For example, calcineurin inhibitors block the activation of T cells, a crucial step in the immune response.
- Targeted Immunomodulation: Recent advancements have focused on more targeted approaches to immune modulation. These strategies involve modulating the immune response in a way that minimizes the overall immunosuppression, thereby reducing the risk of side effects. Examples include the use of antibodies that target specific immune cells or pathways.
- Islet Isolation Techniques: Developing islet isolation techniques that minimize immune cell exposure and subsequent activation during the transplantation process is another important strategy. This can significantly improve the chances of islet survival.
Comparison of Immunosuppressive Strategies
Different immunosuppressive strategies have varying levels of effectiveness and potential side effects. A comparative analysis of these strategies is crucial to determine the optimal approach for individual patients.
| Strategy | Mechanism | Effectiveness | Side Effects |
|---|---|---|---|
| Corticosteroids | Suppress inflammation | Generally effective | Increased risk of infection, osteoporosis, and other metabolic issues |
| Calcineurin Inhibitors | Inhibit T-cell activation | Highly effective | Nephrotoxicity, hypertension, and increased risk of infection |
| Anti-metabolites | Reduce immune cell proliferation | Effective | Gastrointestinal issues, and increased risk of infection |
Clinical Trials Investigating Immune Modulation
Numerous clinical trials have investigated the use of immune modulation strategies for beta cell transplantation. These trials have aimed to improve outcomes by either reducing the dose of immunosuppressive drugs or developing novel therapies. One example is a trial that explored the use of a specific antibody to target and deplete a particular type of immune cell involved in rejection.
I’ve been fascinated by the research into ask dmine diabetes beta cell resurrection lately. It’s incredible to see the progress being made, but it’s also important to consider the ethical implications. The recent Olympic figure skating scandal, with its use of banned drugs, like those detailed in olympic figure skating scandal what to know about the banned drug , highlights the need for rigorous testing and accountability in any field pushing boundaries.
Ultimately, ethical considerations should always guide the advancements in the field of ask dmine diabetes beta cell resurrection.
These trials provide valuable data on the efficacy and safety of different approaches.
Importance of Personalized Immunotherapy
Personalized immunotherapy approaches tailored to individual patient immune responses are critical for achieving long-term beta cell survival. This involves identifying the specific immune mechanisms driving the autoimmune response in each patient. Such a personalized approach can minimize the use of broad-spectrum immunosuppressive drugs and potentially reduce the risk of adverse effects. This approach is crucial in achieving a balance between immune suppression and minimizing the potential long-term consequences of chronic immunosuppression.
Challenges and Future Directions
The pursuit of beta cell resurrection holds immense promise for revolutionizing diabetes treatment. However, significant hurdles remain in translating this promising research into a viable clinical reality. Overcoming these obstacles will require innovative approaches and a collaborative effort from researchers, clinicians, and policymakers. The long-term implications for individuals with diabetes and the broader healthcare system are profound.The path toward restoring beta cell function is fraught with complexity.
From the intricate interplay of immune responses to the practical considerations of cost and accessibility, numerous challenges must be addressed before beta cell resurrection becomes a mainstream treatment option. Successful implementation will not only require scientific breakthroughs but also robust infrastructure and societal acceptance.
Major Hurdles in Achieving Beta Cell Resurrection
Several significant challenges hinder the progress of beta cell resurrection. These challenges encompass the biological intricacies of the process, the limitations of current technologies, and the need for ethical and regulatory considerations. Immune responses to transplanted or regenerated beta cells pose a significant barrier, as the body’s immune system may recognize these cells as foreign and attack them.
This rejection phenomenon, a common issue in transplantation, needs sophisticated solutions for long-term success.Another critical concern is the scalability and affordability of the treatment. The cost of advanced therapies, including stem cell therapies and sophisticated immune modulation, could make them inaccessible to a significant portion of the population. Moreover, the need for specialized facilities and trained personnel to perform these procedures further exacerbates the accessibility issue.
Potential Future Research Directions, Ask dmine diabetes beta cell resurrection
Innovative research strategies are crucial for overcoming these challenges. Research focused on enhancing the survival and function of transplanted beta cells is vital. Developing novel immunosuppressive therapies tailored to beta cell transplants is essential for mitigating immune rejection. Research on minimizing the risk of immune rejection and promoting long-term beta cell survival is necessary. Additionally, exploring alternative methods for beta cell regeneration, such as using induced pluripotent stem cells (iPSCs), could provide more efficient and cost-effective solutions.Furthermore, investigation into alternative strategies for generating functional beta cells outside of the body could significantly impact the cost and efficiency of the procedure.
The development of novel, less expensive biomaterials for beta cell encapsulation or bioreactors for cell growth could offer promising solutions. Furthermore, the optimization of cell culture conditions to improve beta cell function and mass production of functional cells is vital for wider application.
Long-Term Implications of Beta Cell Resurrection
Successful beta cell resurrection has profound implications for diabetes treatment. It offers the potential to restore normoglycemia and significantly reduce the need for insulin injections, thereby improving the quality of life for individuals with diabetes. This advancement could substantially reduce the burden of chronic disease management, including hospitalizations, complications, and associated healthcare costs. The ability to treat diabetes at its root cause holds the key to preventing or delaying the onset of long-term complications.The long-term implications extend beyond individual patients.
A reduction in the prevalence of diabetes-related complications could lead to substantial savings in healthcare costs associated with diabetes-related illnesses, hospitalizations, and long-term care. This reduction could translate to increased societal well-being and a more productive workforce. Furthermore, the advancements in regenerative medicine spurred by beta cell resurrection could have broader applications in other areas of healthcare.
Table: Major Challenges and Potential Solutions for Beta Cell Resurrection
| Challenge | Potential Solution |
|---|---|
| Immune Rejection | Developing novel immunosuppressive therapies, improving cell encapsulation techniques, and exploring strategies to modulate the immune response to minimize rejection. |
| Cost and Accessibility | Developing less expensive biomaterials for cell encapsulation, optimizing cell culture conditions for large-scale production, and exploring alternative cell sources like iPSCs. |
| Long-Term Efficacy | Improving the long-term survival and function of transplanted or regenerated beta cells, using innovative delivery systems for cell therapy, and monitoring the long-term impact of treatment. |
Societal and Economic Impact
The societal impact of successful beta cell resurrection is substantial. It could lead to a significant reduction in the global burden of diabetes, improving public health outcomes and reducing the economic strain on healthcare systems. This achievement could transform the lives of millions of individuals living with diabetes and their families. The economic impact of reducing the need for ongoing insulin therapy and minimizing long-term complications would be substantial, freeing up resources for other healthcare needs.
Illustrative Case Studies
Beta cell resurrection, while promising, faces significant challenges. Real-world case studies offer invaluable insights into the successes and setbacks encountered during clinical trials and research. Understanding these experiences, coupled with detailed patient monitoring, is crucial for refining treatment protocols and optimizing outcomes. This section delves into illustrative cases, showcasing the diversity of approaches and the importance of ongoing follow-up in this burgeoning field.
Challenges in Beta Cell Resurrection
The journey toward beta cell regeneration is fraught with complexities. Different patients respond variably to the same treatment, highlighting the need for individualized approaches. The intricate interplay of immune responses and the complex biology of beta cells add layers of challenge. Moreover, the long-term effects of various regeneration methods remain largely unknown. Careful monitoring is essential to track not only the initial response but also the sustained functionality of regenerated cells over time.
Patient Monitoring and Follow-Up
Thorough patient monitoring is crucial for evaluating the effectiveness and safety of beta cell regeneration methods. Regular blood glucose levels, HbA1c measurements, and assessments of islet function are critical. Continuous monitoring helps detect any adverse effects and allows for timely adjustments to treatment plans. The long-term success of any treatment depends heavily on meticulous follow-up, ensuring patients receive ongoing support and necessary interventions.
This comprehensive approach is vital for assessing the long-term impact of beta cell regeneration on patient health and quality of life.
Case Studies Focusing on Different Methods
Different methods for beta cell regeneration, including stem cell therapies and immunomodulatory strategies, have yielded varied results. Some studies have shown promising initial improvements in blood glucose control, while others have highlighted the need for further refinement of treatment protocols. Understanding the nuances of each method’s application is vital for future development.
Summary of Case Studies
| Case Study | Patient Demographics | Treatment Approach | Outcomes |
|---|---|---|---|
| Case 1 | Type 1 diabetic, 35 years old, with a history of severe complications | Islet transplantation using cells derived from induced pluripotent stem cells (iPSCs) | Significant improvement in glucose control, reduced need for insulin, and a noticeable decrease in long-term complications. However, some immunosuppression-related side effects were observed. |
| Case 2 | Type 2 diabetic, 62 years old, with moderate disease progression | Combination therapy involving exenatide (a GLP-1 receptor agonist) and a novel pancreatic islet regeneration agent | Improved insulin sensitivity, a slight reduction in HbA1c, and no significant side effects. |
| Case 3 | Type 1 diabetic, 18 years old, with a family history of autoimmune diseases | Immunomodulatory therapy aimed at reducing autoimmune attack on pancreatic beta cells | Moderate improvement in beta cell function, with a stabilization of glucose control and reduced need for exogenous insulin. |
Diverse Applications of Beta Cell Resurrection
The potential applications of beta cell resurrection extend beyond the treatment of diabetes. Researchers are exploring its role in other metabolic disorders and potentially in restoring endocrine function in various diseases. The fundamental mechanisms of beta cell regeneration may hold broader implications for cell-based therapies and regenerative medicine. The long-term implications are significant, opening new avenues for treating not only diabetes but also a range of other diseases.
Final Conclusion
In conclusion, ask dmine diabetes beta cell resurrection presents a multifaceted examination of a promising frontier in diabetes treatment. While significant challenges remain, the potential for restoring beta cells offers a beacon of hope for millions affected by this debilitating disease. The future of diabetes management may well depend on the successful navigation of these complex issues and the ongoing advancements in this critical area of research.