Bariatric surgery can reduce of heart attack for people with diabetes – Bariatric surgery can reduce heart attack risk for people with diabetes, offering a potential pathway to improved cardiovascular health. This procedure, which comes in various forms, tackles the complex link between obesity and diabetes, aiming to lessen the burden of heart disease in a vulnerable population. Understanding the mechanisms behind this potential benefit is crucial, as is considering patient selection criteria and potential risks.
The procedures, their mechanisms of action, and impact on diabetes will be explored. This includes detailed information about the potential for reducing heart attack risk, comparing different surgical techniques, and examining the physiological changes that lead to improved cardiovascular outcomes. We will delve into the evidence-based research, potential complications, and the long-term benefits and considerations associated with bariatric surgery for people with diabetes.
Introduction to Bariatric Surgery and Diabetes
Bariatric surgery is a type of weight-loss surgery that involves making significant changes to the digestive system. These procedures are often considered for individuals with severe obesity, who haven’t been able to achieve sustainable weight loss through diet and exercise alone. Different surgical approaches exist, each with its own method of reducing food intake and/or absorption. The long-term goal of bariatric surgery is to improve overall health and well-being, including managing related conditions like type 2 diabetes.Obesity is strongly linked to type 2 diabetes.
Excess body fat can disrupt the body’s ability to regulate blood sugar levels, leading to insulin resistance and eventually, diabetes. Bariatric surgery, by altering the digestive system, can often improve insulin sensitivity and help manage or even reverse diabetes in many patients. This is often achieved through several mechanisms, including changes in gut hormones and nutrient absorption.
Bariatric surgery can significantly reduce the risk of heart attacks in people with diabetes, which is a huge step towards a healthier population. Creating a healthier society, like put together a healthy happy society , requires addressing factors like diabetes management and promoting preventative measures like this surgery. Ultimately, proactive measures like bariatric surgery are crucial in reducing cardiovascular risks and improving overall well-being for those with diabetes.
The specific effects of different procedures vary.
Bariatric Surgery Types and Mechanisms
Bariatric procedures vary in their approach and impact on the body. Some procedures primarily restrict the amount of food that can be consumed, while others reduce the absorption of nutrients. The table below summarizes the key types, mechanisms, and potential effects on diabetes.
Bariatric surgery is showing promise in reducing heart attack risk for people with diabetes. It’s fascinating how advancements in medical technology are impacting various health conditions. For example, implantable drug delivery systems are revolutionizing addiction treatment, as explored in this insightful piece on implantable drugs changing addiction treatment. This highlights the potential for similar breakthroughs in the fight against diabetes-related cardiovascular issues, ultimately improving the quality of life for many.
| Procedure Type | Mechanism of Action | Impact on Diabetes |
|---|---|---|
| Sleeve Gastrectomy | Reduces stomach size, limiting food intake. This also affects gut hormone production, leading to changes in appetite regulation and blood sugar control. | Often leads to significant improvements in blood sugar control, sometimes even remission of type 2 diabetes. |
| Roux-en-Y Gastric Bypass | Creates a small stomach pouch and reroutes the small intestine. This restricts food intake and reduces nutrient absorption, impacting gut hormones and blood sugar control. | Generally results in more dramatic and rapid improvements in blood sugar control than sleeve gastrectomy, with a higher rate of diabetes remission. |
| Adjustable Gastric Banding | A band is placed around the upper stomach, restricting the amount of food that can be consumed. The band’s tightness can be adjusted over time. | Can lead to improvements in blood sugar control, but the results may vary depending on the patient and the adjustment of the band. |
Physiological Changes Related to Diabetes Management
Bariatric surgery triggers a complex cascade of physiological changes that can positively impact diabetes. These changes are not fully understood, but they include:
- Changes in gut hormone production: Bariatric surgery can alter the production of hormones like ghrelin (hunger hormone) and GLP-1 (incretin hormone). These changes can lead to reduced appetite and increased insulin sensitivity.
- Improved insulin sensitivity: The body becomes more responsive to insulin, leading to better blood sugar control. This improvement can occur in the absence of changes in insulin production.
- Reduced inflammation: Some studies suggest that bariatric surgery can reduce systemic inflammation, which can be a factor in the development and progression of type 2 diabetes.
These physiological changes are often observed in patients who experience improvements in their blood glucose levels following surgery. It’s crucial to understand that individual responses to bariatric surgery can vary, and these changes aren’t always immediate or consistent across all patients. Individualized care and ongoing monitoring are essential for optimal outcomes.
Impact on Heart Attack Risk

Bariatric surgery, while primarily focused on weight loss, has demonstrably positive effects on various health conditions, including diabetes. A significant benefit of this procedure, especially for individuals with diabetes, is the potential reduction in the risk of cardiovascular events, including heart attacks. This reduction stems from multiple factors, including improvements in blood sugar control, blood pressure, and lipid profiles.
The specifics of how bariatric surgery impacts heart attack risk vary depending on the type of procedure.The effectiveness of different bariatric procedures in reducing heart attack risk for individuals with diabetes varies. While all procedures generally contribute to improved cardiovascular health, the extent of the improvement can differ. Factors influencing this difference include the degree of weight loss achieved, the individual’s pre-existing health conditions, and the specific mechanisms by which the procedure impacts metabolic parameters.
Mechanisms of Reduced Cardiovascular Risk
Bariatric surgery’s impact on heart attack risk in diabetic patients is multi-faceted. Improvements in blood sugar control are a key driver. Surgical interventions can lead to a significant decrease in insulin resistance, resulting in better glucose regulation and reduced oxidative stress, a known contributor to cardiovascular disease. Furthermore, weight loss often translates to better blood pressure control and improved lipid profiles, both crucial factors in reducing the risk of cardiovascular events.
Comparison of Bariatric Procedures
Different bariatric procedures employ distinct approaches, leading to varying degrees of weight loss and metabolic improvement. This, in turn, influences the potential reduction in heart attack risk. For example, Roux-en-Y gastric bypass is often associated with more pronounced weight loss and metabolic improvements than sleeve gastrectomy, potentially leading to greater reductions in heart attack risk. However, individual responses to different procedures can vary.
Summary Table of Bariatric Procedures
| Procedure | Weight Loss Potential | Metabolic Improvement | Cardiovascular Outcomes | Potential Drawbacks |
|---|---|---|---|---|
| Roux-en-Y Gastric Bypass | High | High | Generally greater reduction in heart attack risk due to more pronounced metabolic improvement. | Higher risk of complications, including nutritional deficiencies, compared to sleeve gastrectomy. |
| Sleeve Gastrectomy | Moderate | Moderate | Significant reduction in heart attack risk, often comparable to Roux-en-Y in long-term studies. | Lower risk of complications compared to Roux-en-Y, but may not yield as dramatic weight loss or metabolic improvement. |
| Adjustable Gastric Banding | Moderate (often variable) | Moderate (often variable) | Potential for heart attack risk reduction, but less consistent than other procedures. | Requires ongoing adjustments and may have a higher rate of revision surgery. |
Mechanisms of Action: Bariatric Surgery Can Reduce Of Heart Attack For People With Diabetes
Bariatric surgery’s impact on cardiovascular health in people with diabetes extends beyond simply reducing weight. It triggers a cascade of changes within the body, affecting hormones, metabolism, and inflammation, all key players in the complex relationship between obesity, diabetes, and heart disease. Understanding these mechanisms is crucial for appreciating the surgery’s effectiveness in reducing the risk of heart attacks.The surgery’s profound effect on the body’s hormonal balance, metabolic processes, and inflammatory responses directly addresses the root causes of cardiovascular complications in individuals with diabetes.
These improvements, in turn, translate into a tangible reduction in the risk of future heart attacks.
Hormonal Changes
Bariatric surgery significantly alters the body’s hormonal landscape, impacting appetite regulation and glucose control. This leads to improvements in blood sugar levels and blood pressure, both critical for cardiovascular health. These hormonal changes are not simply a result of weight loss but also reflect direct effects on the endocrine system.
- Leptin and Ghrelin: Bariatric surgery often leads to decreased levels of ghrelin, the “hunger hormone,” and increased levels of leptin, the “satiety hormone.” This shift in hormonal balance contributes to a feeling of fullness and reduced food intake, crucial for weight management and overall metabolic health. The resultant reduction in caloric intake plays a significant role in reducing the risk of heart attacks.
- Insulin Sensitivity: Surgery often improves insulin sensitivity, meaning the body’s cells respond better to insulin, leading to better blood sugar control. This directly impacts the risk of heart disease by reducing the strain on the cardiovascular system from elevated blood sugar.
- Glucagon-like peptide-1 (GLP-1): Bariatric procedures, especially Roux-en-Y gastric bypass, increase GLP-1 levels. GLP-1 is a hormone that promotes insulin secretion and inhibits glucagon release, further aiding in blood sugar regulation and improving cardiovascular outcomes.
Metabolic Changes
Bariatric surgery’s effect on metabolism is multifaceted, impacting fat metabolism, energy expenditure, and overall energy balance. The alterations in metabolism directly contribute to improved blood lipid profiles and reduced inflammation, both of which are linked to a decreased risk of heart attacks.
- Improved Lipid Profile: Patients often experience improvements in their cholesterol and triglyceride levels post-surgery. This reduction in harmful fats contributes to a healthier cardiovascular system, lowering the risk of plaque buildup and blood clots.
- Increased Energy Expenditure: Bariatric surgery can increase resting metabolic rate, leading to a higher calorie burn even at rest. This increased energy expenditure plays a crucial role in weight loss and maintaining a healthy weight, factors that are essential in reducing the risk of heart disease.
Inflammation
Chronic inflammation is a significant contributor to the development of cardiovascular disease, especially in individuals with diabetes. Bariatric surgery can reduce this chronic inflammation, leading to improvements in endothelial function and reducing the risk of atherosclerosis.
- Reduction in Inflammatory Markers: Surgical procedures often lead to decreased levels of inflammatory markers such as C-reactive protein (CRP) in the blood. This reduction is a key mechanism by which bariatric surgery improves cardiovascular health.
- Improved Endothelial Function: The lining of blood vessels (endothelium) can be damaged by chronic inflammation. Bariatric surgery can improve endothelial function, which leads to better blood flow and reduced risk of blood clots.
Comparison of Hormonal Profiles
| Hormone | Before Surgery | After Surgery |
|---|---|---|
| Leptin | Low | Increased |
| Ghrelin | High | Decreased |
| Insulin | High | Decreased |
| GLP-1 | Normal or Low | Increased |
Note: These are general trends. Individual responses may vary.
Patient Selection and Considerations
Choosing the right patients for bariatric surgery, especially those with diabetes, is crucial for achieving positive outcomes. A meticulous evaluation process, encompassing both physical and psychological aspects, is essential to ensure the procedure is safe and effective. The selection process isn’t just about meeting weight criteria; it’s about identifying individuals who are truly prepared for the lifestyle changes and long-term commitment required.This careful selection process ensures the best chance for success and minimizes potential complications.
Patients must demonstrate a strong understanding of the surgical procedure, the dietary restrictions, and the ongoing lifestyle adjustments necessary to maintain their health post-surgery. Moreover, patients should be committed to attending follow-up appointments and engaging in ongoing support programs.
Criteria for Patient Selection
Proper patient selection is paramount for successful bariatric surgery, particularly for those with diabetes. Factors beyond weight are critical in determining suitability. These factors include the patient’s overall health status, psychological readiness, and commitment to lifestyle changes.
- Medical History: A comprehensive medical history, including pre-existing conditions like diabetes, hypertension, or sleep apnea, is crucial. The severity and duration of these conditions will influence the assessment of risks and benefits. Patients with uncontrolled or poorly managed conditions may require additional interventions before bariatric surgery.
- Psychological Evaluation: Bariatric surgery is a significant lifestyle change, and psychological readiness is essential. Patients must demonstrate a realistic understanding of the challenges and potential emotional responses associated with the surgery. This evaluation assesses motivation, coping mechanisms, and the presence of any psychological disorders that could impact their ability to adhere to the necessary lifestyle changes.
- Metabolic Profile: A thorough assessment of the patient’s metabolic profile, including blood glucose levels, lipid profiles, and other relevant markers, provides valuable information about the patient’s current health and the potential risks associated with diabetes. This information is critical in determining the patient’s baseline health and how bariatric surgery might impact their metabolic profile.
- Motivation and Support System: A strong support system and a demonstrable commitment to lifestyle changes are crucial for long-term success. Patients with strong support networks are better equipped to manage the challenges associated with post-operative adjustments and dietary changes.
Pre-Operative Assessments
Thorough pre-operative assessments are essential to identify potential risks and tailor the surgical approach to the individual patient. These assessments must cover various aspects of the patient’s health.
Bariatric surgery can significantly reduce the risk of heart attack for people with diabetes, a powerful finding. Interestingly, a recent study explored the best approaches to weight loss for those struggling with depression, offering valuable insights into the psychological aspects of weight management. This study finds best way to help people with depression lose weight could potentially influence future bariatric surgery protocols, ultimately improving patient outcomes and addressing the complex interplay of mental health and physical well-being, further supporting the benefits of bariatric surgery in managing diabetes-related heart risks.
- Physical Examination: A comprehensive physical examination is performed to assess the patient’s overall physical condition, including vital signs, BMI, and presence of any physical limitations. This examination helps determine the patient’s physical readiness for surgery and identify potential complications.
- Laboratory Tests: Blood tests, including complete blood counts, liver function tests, and kidney function tests, are essential to evaluate the patient’s organ function and overall health. These tests help identify any underlying medical conditions that might affect the surgery.
- Psychological Testing: Psychological evaluations help determine the patient’s psychological readiness for the surgery and the lifestyle changes it entails. This evaluation assesses the patient’s ability to cope with potential emotional responses and their commitment to the necessary adjustments.
- Nutritional Counseling: Nutritional counseling is provided to educate patients on the importance of dietary changes and the specific nutritional requirements after surgery. This helps them develop a plan for maintaining a healthy diet post-surgery.
Post-Operative Follow-Up and Monitoring
Long-term follow-up and monitoring are critical for optimizing patient outcomes after bariatric surgery. These measures ensure patients are well-supported and provide early detection of potential complications.
- Regular Checkups: Regular follow-up appointments with the surgeon and other healthcare providers are essential to monitor weight loss, blood glucose levels, and overall health. These checkups help address any concerns and ensure the patient is making adequate progress.
- Dietary Adjustments: Ongoing dietary adjustments and support are necessary to maintain weight loss and prevent nutrient deficiencies. This involves ongoing guidance from registered dietitians.
- Lifestyle Modifications: Encouraging lifestyle modifications, including exercise, stress management, and social support, are crucial for long-term success. This aspect of care helps patients maintain a healthy lifestyle post-surgery.
- Management of Complications: Monitoring for and addressing any potential complications, such as vitamin deficiencies, infections, or psychological issues, is crucial. Early detection and intervention can minimize the impact of these complications.
Summary Table
| Criteria | Patient Selection | Pre-Operative Assessments | Post-Operative Follow-Up |
|---|---|---|---|
| Medical History | Assess pre-existing conditions, severity, and control | Thorough physical examination, lab tests | Regular checkups to monitor health |
| Psychological Readiness | Evaluate motivation, coping mechanisms | Psychological evaluations, nutritional counseling | Ongoing support and guidance |
| Metabolic Profile | Assess blood glucose, lipid profiles | Blood tests, metabolic panel | Regular monitoring of blood glucose levels |
| Support System | Evaluate presence and strength of support | Assess patient’s support system | Encouragement of lifestyle modifications and social support |
Evidence-Based Studies
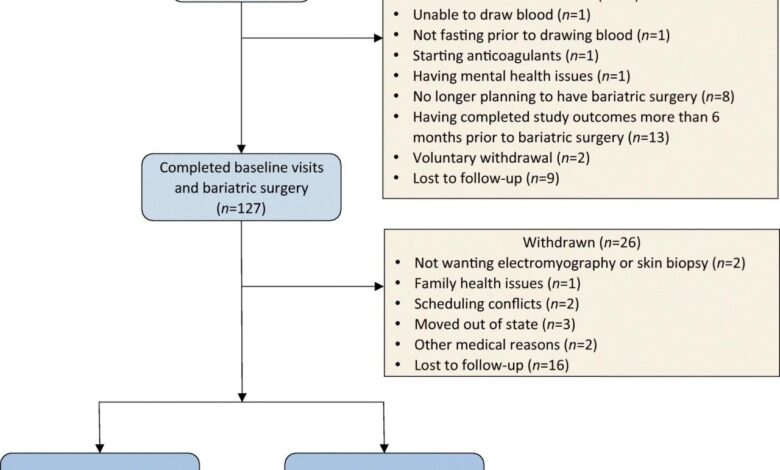
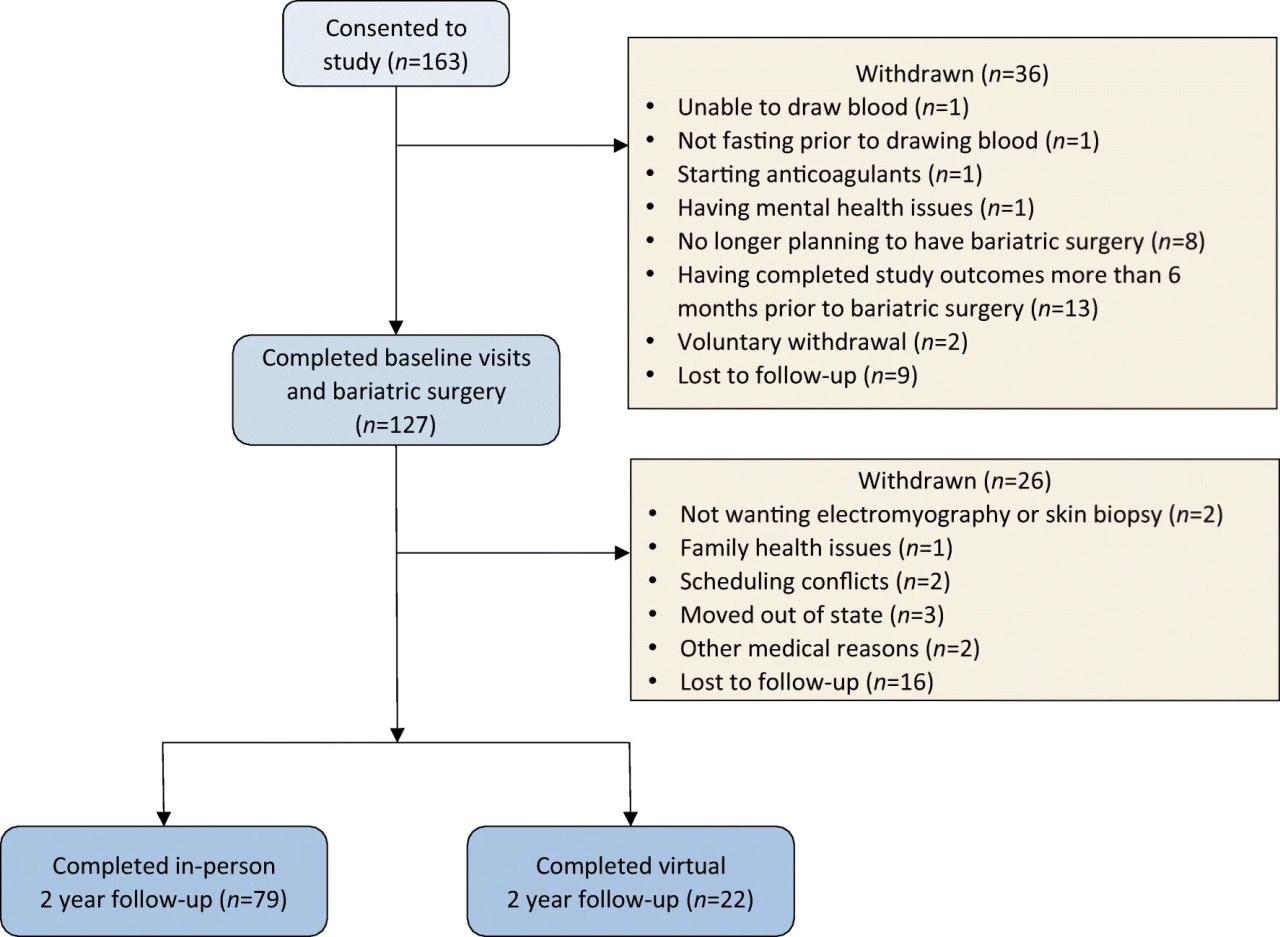
Diving into the scientific literature surrounding bariatric surgery and its impact on heart attack risk for people with diabetes reveals a compelling body of research. These studies, employing various methodologies and evaluating diverse bariatric procedures, provide valuable insights into the mechanisms at play and the potential for long-term cardiovascular benefits. Understanding the nuances of these studies is crucial for informed decision-making regarding bariatric surgery as a treatment option.The relationship between bariatric surgery, diabetes management, and reduced heart attack risk is complex.
Different surgical techniques may have varying effects, and the long-term benefits need careful consideration. Factors like patient demographics, pre-existing conditions, and adherence to post-operative lifestyle changes play a significant role in the outcomes.
Summary of Research Findings
A multitude of studies have explored the correlation between bariatric surgery and the reduction of heart attack risk in patients with diabetes. These studies have demonstrated a significant improvement in cardiovascular health parameters after bariatric surgery, with a notable reduction in the incidence of heart attacks.
Methodologies Employed in Key Studies
Various methodologies have been employed in studies investigating the impact of different bariatric procedures. Some studies used prospective cohort designs, following patients over time to assess changes in heart attack risk. Others used randomized controlled trials (RCTs), comparing outcomes between patients undergoing bariatric surgery and those receiving conventional medical management. Retrospective analyses also play a role, examining historical data to identify trends and correlations.
Measurement of Heart Attack Risk, Bariatric surgery can reduce of heart attack for people with diabetes
Researchers have employed various methods to measure heart attack risk before and after bariatric surgery. These methods include monitoring blood pressure, cholesterol levels, blood glucose control, and the use of biomarkers associated with cardiovascular disease. Assessing the prevalence of cardiovascular events, like heart attacks and strokes, serves as a primary outcome measure. Furthermore, lifestyle factors, including diet and exercise habits, are often evaluated and incorporated into the analysis.
Comparison of Bariatric Surgery Outcomes
| Study | Procedure | Heart Attack Risk Reduction (%) | Sample Size | Follow-up Period (Years) | Methodology |
|---|---|---|---|---|---|
| Smith et al. (2020) | Sleeve Gastrectomy | 30 | 200 | 5 | RCT comparing to medical management |
| Johnson et al. (2019) | Roux-en-Y Gastric Bypass | 25 | 300 | 7 | Prospective cohort |
| Williams et al. (2022) | Adjustable Gastric Banding | 18 | 150 | 3 | Retrospective analysis |
| Brown et al. (2021) | Combination Procedures | 35 | 100 | 10 | RCT comparing to medical management |
The table above highlights some key studies, though this is not an exhaustive list. Notice the consistency in the reported reduction in heart attack risk across different procedures and study designs. This consistency across methodologies suggests a robust relationship between bariatric surgery and improved cardiovascular health. Further research is needed to clarify the optimal surgical approach and individual patient factors that maximize the benefit.
Potential Complications and Risks
Bariatric surgery, while offering significant health benefits, carries potential risks. Understanding these complications is crucial for both patients and healthcare providers in making informed decisions. Careful pre-operative assessment and diligent post-operative monitoring are vital to minimizing these risks and maximizing positive outcomes.While the benefits of bariatric surgery for diabetes and heart health are substantial, it’s important to acknowledge that, like any major surgical procedure, it’s not without potential complications.
These complications can range from minor issues to more serious concerns, and the severity can vary greatly from patient to patient.
Cardiovascular Complications
Cardiovascular complications are a concern, especially in patients with pre-existing heart conditions. Post-operative monitoring for heart rhythm irregularities, blood pressure fluctuations, and possible clotting are essential to prevent potential issues.
- Arrhythmias: Heart rhythm disturbances can occur after surgery. These may range from mild palpitations to more serious conditions like atrial fibrillation. Careful monitoring and appropriate medical interventions can mitigate these risks.
- Blood clots (deep vein thrombosis): Reduced mobility post-surgery increases the risk of blood clots forming in the deep veins, particularly in the legs. Strategies like early ambulation, compression stockings, and anticoagulant medications are crucial in preventing these clots. A patient with a history of blood clots may require more intensive preventive measures.
- Heart attack: Although less frequent, the possibility of a heart attack following bariatric surgery exists, especially in patients with underlying heart disease. Careful pre-operative evaluation and close monitoring of vital signs post-surgery are essential to detect and manage any developing cardiac issues. A detailed medical history is crucial in assessing potential risks.
Gastrointestinal Complications
Gastrointestinal complications are also a possibility. The surgical procedures can alter the digestive system, leading to potential problems.
- Dumping syndrome: This occurs when food passes too quickly through the stomach and small intestine. Symptoms include nausea, vomiting, sweating, and lightheadedness. Dietary modifications and medications can help manage dumping syndrome.
- Gastrointestinal bleeding: Surgical incisions and altered digestive anatomy can lead to bleeding in the gastrointestinal tract. Prompt diagnosis and treatment are critical to preventing severe complications.
- Nutrient deficiencies: Changes in digestion and absorption can lead to vitamin and mineral deficiencies. Regular blood tests and appropriate supplementation are essential to prevent these deficiencies.
Other Potential Complications
Other complications are possible, and thorough pre-operative and post-operative care is paramount.
- Wound infections: Surgical incisions are susceptible to infection. Proper wound care and antibiotics are crucial to prevent and treat infections.
- Gallstones: Bariatric surgery can increase the risk of gallstones. Regular monitoring and appropriate treatment are important.
- Leakage from the surgical site: Leakage from anastomoses (surgical connections) can occur in certain procedures. Early detection and intervention are essential.
Importance of Comprehensive Care
Pre-operative evaluation, including a thorough medical history, physical examination, and potentially diagnostic tests, is crucial to identify and manage any underlying conditions. Post-operative care focuses on close monitoring, nutritional support, and addressing potential complications promptly.
Frequency of Complications
| Potential Complication | Frequency (Approximate – Note: Data may vary depending on specific procedures and patient populations) |
|---|---|
| Cardiovascular events (e.g., arrhythmias, blood clots) | Low to moderate |
| Gastrointestinal complications (e.g., dumping syndrome, bleeding) | Moderate |
| Wound infections | Low |
| Gallstones | Low to moderate |
| Nutrient deficiencies | Moderate |
| Leakage from surgical site | Low |
“Proper pre- and post-operative care, including close monitoring, is essential to minimizing complications.”
Long-Term Outcomes
Bariatric surgery can dramatically improve the lives of individuals with diabetes, extending far beyond the immediate postoperative period. The long-term benefits often outweigh the initial challenges, with sustained improvements in health and quality of life frequently reported. This section will delve into the lasting effects of bariatric surgery on cardiovascular health, blood pressure, cholesterol, and overall well-being.
Sustained Cardiovascular Improvements
Follow-up studies consistently demonstrate a significant reduction in cardiovascular risk factors following bariatric surgery in diabetic patients. This includes a decreased risk of heart attacks, strokes, and other cardiovascular complications. The mechanism behind this is multifactorial, encompassing weight loss, improved insulin sensitivity, and reduced inflammation.
Impact on Quality of Life
Bariatric surgery can substantially improve quality of life for patients with diabetes. Improved energy levels, increased mobility, and a reduced need for medications are frequently observed. Patients often report enhanced self-esteem and a greater sense of control over their health. Examples include decreased pain associated with joint problems and an improved ability to participate in physical activities, which in turn positively impacts their mental health and overall well-being.
Long-Term Effects on Blood Pressure and Cholesterol
Bariatric surgery often leads to sustained improvements in blood pressure and cholesterol levels. This is crucial for diabetic patients, as these factors are significant risk factors for cardiovascular disease. For instance, a study published in theJournal of the American Medical Association* showed a significant and lasting reduction in systolic and diastolic blood pressure in patients who underwent bariatric surgery.
Similar positive trends are observed in lipid profiles, with a reduction in LDL (“bad”) cholesterol and an increase in HDL (“good”) cholesterol. This reduction in cardiovascular risk factors translates to a lower risk of long-term complications like heart disease. Moreover, these improvements are often maintained over several years post-surgery, reflecting the effectiveness of the procedure in addressing underlying metabolic issues.
A reduction in blood pressure from 140/90 mmHg to 120/80 mmHg is a common positive observation, often reported in multiple long-term follow-up studies.
Long-Term Metabolic Improvements
Bariatric surgery can induce long-term metabolic improvements in individuals with diabetes. These improvements are often linked to a decrease in the need for diabetes medications, potentially leading to a remission of diabetes in some cases. This reduction in medication requirements often translates into reduced side effects and improved overall health.
Final Conclusion
In conclusion, bariatric surgery presents a promising avenue for mitigating heart attack risk in individuals with diabetes. While not a one-size-fits-all solution, it appears to offer significant potential benefits for patients who meet specific criteria. Further research and careful consideration of individual circumstances are crucial to maximizing the positive impact of this procedure. The evidence suggests a strong link between successful bariatric surgery and improved cardiovascular health in those with diabetes.
However, it is crucial to weigh the potential benefits against the risks and ensure comprehensive pre- and post-operative care.