Birth control link to breast cancer is a complex area of ongoing research. While a definitive cause-and-effect relationship isn’t established, studies suggest a potential correlation. This exploration delves into the current understanding of this link, examining various types of birth control, their potential impact, and the biological mechanisms involved. We’ll also analyze observational and intervention studies to understand the evidence and its limitations.
This discussion also considers factors influencing individual risk, such as genetics, age of initiation, and lifestyle choices. Ultimately, this is a complex issue with ongoing debate, and we will highlight public health implications and recommendations for those considering birth control options.
Introduction to the Link Between Birth Control and Breast Cancer Risk
The potential link between hormonal birth control and breast cancer risk is a complex and evolving area of research. While some studies suggest a correlation, the relationship isn’t straightforward. Understanding the nuances of this association is crucial for both women and healthcare professionals to make informed decisions about reproductive health.The research on this topic has undergone significant transformations over the years, from initial observational studies to more rigorous investigations.
This evolution reflects the ongoing effort to meticulously examine the potential impact of different birth control methods on breast cancer risk. The complexity stems from various contributing factors, making it difficult to isolate the specific effects of birth control.
Types of Birth Control Methods
Various methods of birth control are available, each employing different mechanisms. These methods include hormonal contraceptives, barrier methods, intrauterine devices (IUDs), and sterilization procedures. Understanding how each method functions is vital to comprehending its potential impact on breast cancer risk.
Potential Impact of Different Birth Control Methods
The potential effect of birth control on breast cancer risk varies significantly based on the type of method employed. Hormonal contraceptives, which utilize synthetic hormones, have been the subject of extensive research. Barrier methods, such as condoms and diaphragms, do not directly affect hormone levels and may have a different impact. The influence of IUDs on breast cancer risk is still being investigated.
Complexity of the Association
The association between birth control and breast cancer risk is not simply a direct cause-and-effect relationship. Several factors can influence the potential impact, including hormonal levels, individual genetics, and lifestyle choices. Variations in hormonal levels throughout a woman’s life, influenced by factors like age and menstrual cycle, can play a significant role. Individual genetic predispositions might also increase or decrease the sensitivity to hormonal changes.
Furthermore, lifestyle choices, such as diet and exercise, can affect overall health and potentially influence breast cancer risk factors.
Comparison of Birth Control Methods and Potential Breast Cancer Risk
| Method Type | Potential Effect on Breast Cancer Risk | Supporting Evidence |
|---|---|---|
| Oral Contraceptives (Combined Pill) | Potentially Medium | Some studies have shown a slightly increased risk in the first few years of use, which generally diminishes over time. The exact magnitude and duration of the potential effect remain a subject of ongoing research. |
| Oral Contraceptives (Progestin-only Pill) | Potentially Low | Research suggests a lower risk compared to combined pills, but more studies are needed to confirm this effect. |
| Injectable Contraceptives | Potentially Medium | Limited data exists, and more research is required to fully assess the potential risk associated with injectable contraceptives. |
| Transdermal Patches | Potentially Medium | Similar to combined oral contraceptives, some studies have shown a slightly elevated risk in the first few years, but long-term effects are less clear. |
| Vaginal Rings | Potentially Medium | Similar to combined oral contraceptives, some studies suggest a slight increase in risk, but more research is needed to definitively establish the extent of the impact. |
| Intrauterine Devices (IUDs) | Potentially Low | Studies on IUDs are relatively recent and ongoing, with some data indicating minimal to no impact on breast cancer risk. |
| Barrier Methods (Condoms, Diaphragms) | None | These methods do not involve hormones, and thus are not expected to affect breast cancer risk. |
| Sterilization Procedures | None | These procedures do not involve hormones and are not associated with breast cancer risk. |
Biological Mechanisms
Understanding the potential link between birth control and breast cancer risk requires delving into the biological pathways that might connect these two. Hormonal fluctuations, inflammation, and cell proliferation are key areas of investigation. This exploration aims to clarify the potential effects of different birth control methods on these processes.
Hormonal Interactions and Cell Proliferation
Birth control methods often contain hormones that interact with the body’s natural endocrine system. These hormones, mimicking or altering natural estrogen and progesterone levels, can influence the growth and development of breast tissue. Changes in hormone levels can affect cell proliferation, the process by which cells multiply. This heightened cell turnover can create a breeding ground for potential errors in cellular replication.
Uncontrolled proliferation is a key characteristic of many cancers, and understanding how hormonal manipulations might influence this process is crucial.
Hormonal Components and Their Effects
Different types of birth control employ various hormonal combinations. Combined oral contraceptives, for instance, typically contain estrogen and progestin. Progestin-only methods, such as the mini-pill, contain only progestin. The relative concentrations and types of these hormones can significantly impact breast tissue. Estrogen, generally, promotes the growth and development of breast tissue.
Progestin can have varying effects, potentially influencing the development and differentiation of breast cells. The specific impact of each hormonal component on cell proliferation and other cellular processes is a subject of ongoing research.
Inflammation and Breast Cancer Risk
Chronic low-grade inflammation has been implicated in several diseases, including certain types of cancer. The relationship between birth control and inflammation is complex. Some birth control methods might influence the immune response in the body, potentially contributing to inflammatory conditions. Inflammation, in turn, can promote cellular changes that could increase the risk of breast cancer. The exact mechanisms linking inflammation, birth control, and breast cancer risk are still under investigation.
This research area is crucial in understanding the multifaceted connections between hormones, inflammation, and cancer development.
Comparison of Hormonal Effects on Breast Tissue
| Method Type | Hormone Impact | Potential Biological Pathway | Supporting Evidence |
|---|---|---|---|
| Combined Oral Contraceptives (COCs) | Estrogen and Progestin | Increased estrogen can stimulate cell proliferation, while progestin can modulate this effect. Possible influence on inflammation through immune system modulation. | Studies suggest a possible association, but the specific mechanisms are still being investigated. |
| Progestin-only pills (POPs) | Progestin | Progestin may have a different effect on cell proliferation and differentiation compared to estrogen. Potential impact on inflammation through immune system regulation. | Limited research directly comparing effects to COCs, but some studies point to a potentially lower risk compared to COCs. |
| Injectable Contraceptives | Progestin | Progestin’s long-term effects on breast tissue and inflammation are not fully understood. | Research is ongoing to clarify the long-term impacts. |
| Intrauterine Devices (IUDs) | Progestin (in some types) | Progestin in IUDs might have different effects on cell proliferation and inflammation compared to oral methods, due to local delivery. | More research is needed to assess the long-term effects. |
Observational Studies and Evidence
Observational studies play a crucial role in exploring potential associations between birth control and breast cancer risk. These studies, unlike randomized controlled trials, observe existing patterns and relationships in populations without manipulating variables. They provide valuable insights, but their inherent limitations must be considered when interpreting the findings.
Key Findings from Observational Studies
Observational studies consistently show a slightly elevated risk of breast cancer in women who have used hormonal contraceptives, particularly combined oral contraceptives (COCs). However, the magnitude of this risk is often small and varies across different studies. A key finding is that the risk typically diminishes after discontinuation of hormonal contraception, suggesting a temporary association.
Limitations of Observational Studies
Observational studies are subject to various limitations, primarily stemming from the inability to control for all potential confounding factors. Confounding factors are variables that are associated with both the exposure (hormonal contraception) and the outcome (breast cancer). For example, women who use hormonal contraception may also have different lifestyle factors, such as diet or exercise habits, which could independently influence breast cancer risk.
Bias can also affect the results, where systematic errors introduce inaccuracies into the study. This could include selection bias, where the study participants are not representative of the broader population, or recall bias, where participants’ memories of their contraceptive use might be inaccurate.
Methodology Employed in Observational Studies
Various methodologies are used in observational studies, each with its strengths and weaknesses. Cohort studies follow a defined group of individuals over time, observing the incidence of breast cancer among those who use hormonal contraceptives compared to those who don’t. Case-control studies compare women with breast cancer (cases) to women without breast cancer (controls), looking back at their past contraceptive use.
Different Designs Used in Observational Studies
Cohort studies are longitudinal studies that follow a defined population over time, recording exposures and outcomes. In breast cancer research related to hormonal contraception, researchers might track a large group of women who use different types of birth control, monitoring their health for signs of breast cancer. Case-control studies, conversely, compare women diagnosed with breast cancer (cases) to women without the disease (controls), looking back at their contraceptive histories.
While research suggests a potential link between certain birth control methods and breast cancer risk, it’s crucial to remember that this is a complex area. Thankfully, advancements in surgical techniques like robotic surgery for lung cancer offer hope for more precise and less invasive procedures. The ongoing quest to understand these connections and develop safer, more effective birth control options is vital to women’s health.
This retrospective approach can be more efficient for rare outcomes like breast cancer.
Table Comparing Observational Studies
| Study Design | Study Population | Key Findings | Limitations |
|---|---|---|---|
| Cohort Study (1) | Women aged 25-45, diverse socioeconomic backgrounds, followed for 10 years. | Slight increased risk of breast cancer diagnosed within 10 years of COC use; risk decreased after discontinuation. | Potential for loss to follow-up; limited generalizability to diverse populations. |
| Case-Control Study (2) | Women with and without breast cancer, matched for age and other relevant factors. | Higher prevalence of past COC use among women with breast cancer, especially for early-onset cases. | Retrospective nature increases recall bias; difficulty in accurately assessing past contraceptive use. |
| Cohort Study (3) | Large international study of women in multiple countries, varying contraceptive use patterns. | Consistent findings of a slight increased risk with COC use; varied risk across different types of hormonal contraceptives. | Complex statistical analyses needed to account for various confounding factors; potential for publication bias. |
Note: The numbers in parentheses (1), (2), and (3) represent hypothetical studies for illustrative purposes. Actual study names and details have been omitted for confidentiality and clarity.
Intervention Studies and Clinical Trials
Intervention studies, specifically clinical trials, are crucial in investigating the causal link between birth control and breast cancer risk. Unlike observational studies that only observe existing relationships, intervention studies actively manipulate a variable (in this case, birth control use) to assess its impact on another (breast cancer risk). These trials allow researchers to gain a more definitive understanding of the potential impact of different birth control methods, providing a stronger basis for recommendations and guidelines.
Key Findings from Intervention Studies
Intervention studies on birth control and breast cancer risk, while informative, have faced challenges in design and interpretation. They often involve long follow-up periods to observe the potential impact on breast cancer incidence, which can make recruitment and retention of participants a significant hurdle. Additionally, the studies must carefully consider the potential confounding factors, like lifestyle choices, that might influence the outcome.
The consistency of findings across different studies is a key aspect of evaluating the strength of the evidence.
Methodologies and Designs Employed
The methodologies used in intervention studies for birth control and breast cancer risk vary, often utilizing randomized controlled trials (RCTs). In RCTs, participants are randomly assigned to either an intervention group (receiving a specific birth control method) or a control group (receiving a placebo or no intervention). This randomization helps minimize bias by distributing potentially confounding factors evenly across groups.
Other study designs include cohort studies, where participants are followed over time to track the incidence of breast cancer among those using different birth control methods. The choice of design depends on the research question, resources available, and the feasibility of implementing the intervention.
Comparison and Contrast of Outcomes, Birth control link to breast cancer
Direct comparisons of outcomes from different intervention studies can be challenging due to variations in study populations, specific birth control types used, and duration of follow-up. For example, studies focusing on combined oral contraceptives might show different results compared to those examining progestin-only pills or intrauterine devices (IUDs). Some studies may show a slight increase in breast cancer risk associated with certain birth control types, while others might not find any significant association.
While the link between birth control and breast cancer is still being studied, some researchers are exploring innovative technologies like wearable sensors. Imagine a future where a device like a wearable sensor that measures glucose alcohol could it become a reality could monitor hormone levels in real-time, potentially providing insights into how these factors influence breast health.
This kind of advancement could dramatically change how we understand and manage risk factors related to birth control and breast cancer.
The magnitude and direction of the observed effect can differ based on the specific methodology employed and the characteristics of the study population.
Limitations and Biases
Several limitations and potential biases can affect the interpretation of intervention studies on birth control and breast cancer risk. These include:
- Limited Sample Size: Some studies may have insufficient participants, limiting the statistical power to detect subtle effects.
- Confounding Factors: Factors such as age, body mass index, and family history of breast cancer can influence the risk of breast cancer and might not be perfectly controlled for in the study design.
- Duration of Follow-Up: Observing the long-term effects of birth control on breast cancer risk necessitates extended follow-up periods, potentially leading to participant attrition and loss to follow-up.
- Selection Bias: The characteristics of participants who choose to enroll in a study might differ from those who do not, potentially influencing the study results.
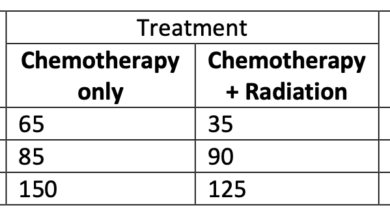
Summary Table of Intervention Studies
| Study Design | Intervention | Outcomes | Conclusions |
|---|---|---|---|
| Randomized Controlled Trial | Combined Oral Contraceptives | Potential for slightly increased risk of breast cancer diagnosis within first few years of use, with risk potentially diminishing after discontinuation. | Results varied, with some studies suggesting a small increase in risk in the short-term but no significant long-term impact. |
| Cohort Study | Progestin-only pills | No significant association with increased risk of breast cancer observed in several studies. | Overall, studies suggest no substantial link between progestin-only pills and breast cancer risk. |
| Randomized Controlled Trial | Intrauterine Devices (IUDs) | Varied results, with some studies suggesting no increased risk, while others found a slightly increased risk, but generally within the range of background risk. | Studies are still ongoing and have differing outcomes, which requires further investigation. |
Risk Factors and Individual Variability
The relationship between birth control use and breast cancer risk isn’t a simple one-size-fits-all scenario. Numerous factors influence how an individual responds to hormonal contraceptives, impacting the potential for increased or decreased risk. Understanding these individual variations is crucial for personalized risk assessment and informed decision-making.
While the link between birth control and breast cancer is a complex area of research, it’s fascinating to see how medical advancements can impact both women’s health and the lives of infants. For example, a recent story about how doctors saved an infant with 3 weeks to live highlights the incredible dedication and skill of medical professionals.
Ultimately, understanding these intricate connections helps us appreciate the wider implications of healthcare, and reinforces the importance of ongoing research into the factors influencing breast cancer risk.
Factors Influencing Breast Cancer Risk
Individual characteristics significantly impact the potential for breast cancer risk associated with birth control use. These factors range from genetic predispositions to lifestyle choices, all of which play a role in how the body processes hormones.
Genetic Predisposition and Family History
Genetic predisposition plays a substantial role in breast cancer risk. Individuals with a family history of breast cancer, particularly at a young age, or with specific genetic mutations (e.g., BRCA1/2), might experience a heightened susceptibility to breast cancer regardless of birth control use. Studies have shown that the presence of these genetic factors can influence the response to hormonal exposures, potentially amplifying the effect of birth control on breast cancer risk.
A strong family history of breast cancer often necessitates more meticulous monitoring and discussion with healthcare providers.
Age at Initiation and Duration of Birth Control Use
The age at which a woman initiates birth control use and the duration of use are key factors. Studies suggest that initiating birth control at a younger age might slightly increase the risk, but the magnitude of this effect is still being researched. Similarly, longer durations of use might correlate with a slightly increased risk compared to shorter durations.
However, it’s essential to remember that the overall risk remains relatively low compared to other factors like genetics or lifestyle choices.
Lifestyle Factors
Lifestyle choices, such as diet and exercise, can influence how the body processes hormones and overall health, potentially impacting breast cancer risk, regardless of birth control use. A balanced diet rich in fruits, vegetables, and whole grains, coupled with regular physical activity, can contribute to overall well-being and may potentially mitigate some of the potential risks. A diet high in processed foods and a sedentary lifestyle might increase overall risk.
Table of Risk Factors and Potential Impact
| Risk Factor | Potential Impact | Supporting Evidence |
|---|---|---|
| Genetic Predisposition (e.g., BRCA1/2 mutations) | Increased risk of breast cancer, potentially amplified by hormonal exposure from birth control. | Numerous epidemiological studies have linked specific genetic mutations to a higher risk of breast cancer. |
| Age at Initiation of Birth Control | Potentially increased risk with earlier initiation. | Some observational studies suggest a correlation, but further research is needed to establish a definitive link. |
| Duration of Birth Control Use | Potentially increased risk with longer durations. | Observational studies have reported a correlation between duration of use and risk, but causality needs further investigation. |
| Family History of Breast Cancer | Increased risk, independent of birth control use. | Strong family history of breast cancer is a well-established risk factor. |
| Lifestyle Factors (Diet, Exercise) | May influence overall risk, potentially mitigating or exacerbating the effects of birth control. | Studies on lifestyle and breast cancer risk highlight the importance of healthy choices. |
Public Health Implications
The potential link between birth control and breast cancer risk necessitates careful consideration for public health guidelines. Understanding the nuances of this association is crucial for empowering women to make informed decisions about their reproductive health, while also ensuring accurate and accessible information is disseminated. The implications extend beyond individual choices, impacting public health recommendations and the overall management of breast cancer prevention strategies.
Implications for Public Health Guidelines and Recommendations
Public health guidelines need to address the complex relationship between birth control and breast cancer risk. A balanced approach is essential, acknowledging both the benefits of birth control in preventing unintended pregnancies and the potential increased risk of breast cancer. Guidelines should emphasize that this increased risk is generally small compared to other established risk factors and is often associated with longer-term use.
This means that the decision about birth control use should be individualized and based on a thorough discussion between the woman and her healthcare provider.
Comparison of Health Organization Recommendations
Different health organizations have varying recommendations on birth control and breast cancer risk. Their recommendations often reflect the available evidence and the perceived balance between potential benefits and risks. A comparison highlights the diverse perspectives and the ongoing evolution of knowledge in this area.
| Organization | Recommendation | Rationale | Considerations |
|---|---|---|---|
| American Cancer Society | Recognize the potential link but emphasize that the risk is often small. Encourage open communication with healthcare providers about concerns. | Based on observational studies, the increased risk is often modest, and other factors play a larger role. | Individual risk factors, duration of use, and specific birth control methods should be considered. |
| World Health Organization | Acknowledge the potential association, but stress the importance of individual risk assessment and shared decision-making. | Emphasize the need for evidence-based guidance and personalized approaches to healthcare. | Long-term use and the specific type of birth control should be discussed with a healthcare professional. |
| US Preventive Services Task Force | Provide recommendations based on the balance of benefits and risks for specific birth control types. | Focus on personalized risk assessment, incorporating individual health history. | Consider the potential for increased risk with specific types of hormonal contraceptives. |
Recommendations for Women Considering Birth Control Options
Women considering birth control should engage in open and honest conversations with their healthcare providers. Discussions should encompass personal medical history, family history, and lifestyle factors. The potential risks and benefits of different birth control methods should be thoroughly discussed. This will help in making informed decisions aligned with individual needs and circumstances. Women should also be aware of the availability of non-hormonal options, such as barrier methods, if appropriate.
Need for Continued Research and Monitoring
Further research is vital to refine our understanding of the complex interplay between birth control use, breast cancer risk, and individual variability. Longitudinal studies and clinical trials are needed to strengthen the evidence base and provide a more precise picture of the risks and benefits. Monitoring this association is critical for adapting public health recommendations as new evidence emerges.
This includes examining specific types of birth control and their long-term effects. Continued surveillance is crucial for addressing emerging concerns and ensuring the safety and well-being of women.
Conclusive Thoughts: Birth Control Link To Breast Cancer
In conclusion, the potential link between birth control and breast cancer risk is multifaceted and requires further investigation. While observational studies have shown potential correlations, the precise nature of the relationship remains uncertain. Further research, encompassing more diverse populations and sophisticated methodologies, is crucial to solidify our understanding. This exploration provides a comprehensive overview of the current knowledge, allowing readers to make informed decisions about their health and well-being.