Black health matters humanity issue is a critical concern that demands our attention. This issue encompasses a multitude of factors, from the historical legacy of systemic racism to the present-day impact of socioeconomic disparities. Understanding these complex interactions is crucial to fostering a healthier and more equitable future for Black communities worldwide. The issue requires examining the deep-rooted historical injustices that have created and sustained health disparities.
We must also analyze the interplay of socioeconomic factors like poverty, housing, and food insecurity, which significantly affect access to quality healthcare and preventative care. This exploration also highlights the critical need for culturally sensitive approaches to healthcare and policies that address environmental injustices.
This comprehensive look at black health matters will explore the historical context of these disparities, the role of socioeconomic factors, access to quality healthcare, specific health issues, cultural factors, public health interventions, environmental influences, intersectionality, and the importance of data and research. Through a detailed analysis, we can better understand the challenges and work towards solutions that promote health equity for Black communities.
Historical Context of Black Health Disparities
The legacy of systemic racism casts a long shadow on the health outcomes of Black communities. Generations of oppression have created and perpetuated significant health disparities, impacting access to quality care, preventative services, and overall well-being. Understanding this historical context is crucial for dismantling these inequities and building a healthier future for all.The pervasive nature of systemic racism has created a complex web of disadvantages that manifest in numerous ways.
From discriminatory housing policies that limit access to healthy environments to biased medical practices that lead to misdiagnosis and inadequate treatment, the effects are deeply ingrained and far-reaching. This historical context necessitates a thorough examination of policies and practices to understand the root causes of these disparities.
Historical Overview of Systemic Racism’s Impact on Black Health
Systemic racism has been a constant throughout American history, deeply impacting Black communities’ health outcomes. From slavery through Jim Crow and into contemporary times, discriminatory practices have shaped the environments and opportunities available to Black individuals, ultimately affecting their health.
Evolution of Policies and Practices Contributing to Disparities
The evolution of policies and practices has significantly shaped the health disparities experienced by Black communities. The following illustrate the historical context:
- Slavery: The brutal conditions of slavery profoundly impacted the health and well-being of enslaved people. Lack of access to basic healthcare, malnutrition, and constant stress resulted in significantly higher rates of illness and mortality. Enslaved people were denied the right to medical care, often treated as property rather than individuals needing care.
- Jim Crow Era: Following the Civil War, the Jim Crow South enforced segregation, creating separate and unequal systems of healthcare. Black individuals were denied access to quality medical care in hospitals and clinics. This period marked a significant escalation in the health disparities faced by Black communities, as limited access to healthcare meant higher rates of preventable illnesses and worse outcomes.
- Mid-20th Century to Present: Although legal segregation ended, implicit bias, discriminatory practices, and unequal access to resources continued. These practices contributed to ongoing health disparities. Factors like housing segregation, environmental racism, and unequal access to quality education have all played a significant role in perpetuating these inequalities.
Key Historical Moments Shaping Current Health Inequities
Certain historical moments serve as stark reminders of the enduring impact of systemic racism on Black health.
- Tuskegee Syphilis Study: This unethical study, conducted from 1932 to 1972, deprived Black men with syphilis of treatment to observe the disease’s progression. This shocking example exposed the profound mistrust of the medical system that continues to impact Black communities today. This event profoundly demonstrated the exploitation and disregard for the well-being of marginalized communities within the medical field.
- Redlining: Residential segregation policies, known as redlining, denied Black families access to mortgages and loans in predominantly white neighborhoods. This limited their ability to secure safe and healthy living environments. The absence of these opportunities often led to overcrowded housing, lack of access to fresh food and other necessities. The effects of redlining continue to impact health outcomes, contributing to environmental health disparities.
Healthcare Access and Quality Comparison Across Time Periods, Black health matters humanity issue
| Time Period | Healthcare Access for Black Communities | Quality of Healthcare |
|---|---|---|
| Pre-Civil War (Slavery) | Denied access to medical care, often treated as property | Nonexistent or rudimentary, based on survival rather than quality |
| Jim Crow Era | Limited access to healthcare in segregated facilities | Substandard care due to segregation and lack of resources |
| Mid-20th Century to Present | Increased access but disparities persist; implicit bias and unequal resource allocation | Improved quality in some areas but persistent disparities in quality of care and access to specialized services |
Socioeconomic Factors Affecting Black Health
The legacy of systemic racism continues to cast a long shadow on the health outcomes of Black communities. Beyond historical injustices, contemporary socioeconomic factors play a crucial role in perpetuating health disparities. Poverty, limited access to resources, and ingrained biases within the healthcare system all contribute to a complex web of challenges that significantly impact the well-being of Black individuals.
Understanding these interconnected factors is vital for developing effective strategies to address the ongoing health crisis within these communities.
The Interplay of Poverty, Housing, and Food Insecurity
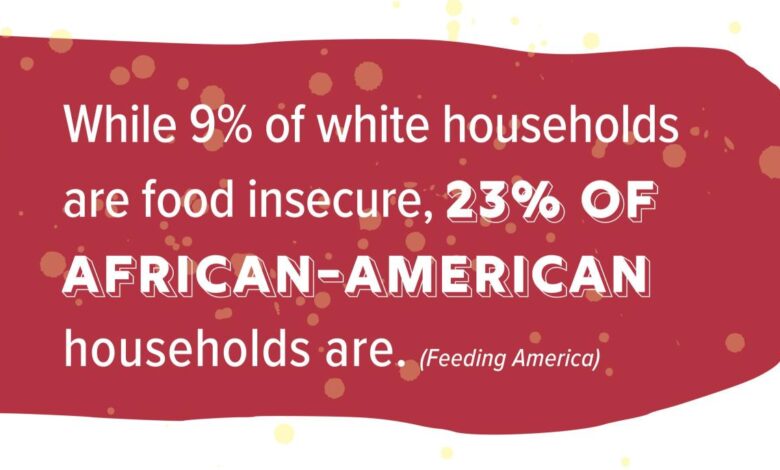
Poverty often leads to inadequate housing conditions, which in turn increase exposure to environmental hazards and limit access to essential resources like clean water and sanitation. These substandard living situations can negatively impact physical and mental health, increasing the risk of various illnesses and exacerbating existing health problems. Food insecurity, a common consequence of poverty, also contributes to poor health outcomes.
Limited access to nutritious food options can result in nutritional deficiencies, impacting growth and development, increasing vulnerability to chronic diseases, and hindering overall well-being. The chronic stress associated with these conditions further compromises the body’s immune response, making individuals more susceptible to illness. For example, areas with high poverty rates often lack access to grocery stores, forcing residents to rely on fast-food restaurants and convenience stores that offer less nutritious options.
Impact of Socioeconomic Status on Healthcare Access
Socioeconomic status significantly influences access to quality healthcare and preventative care. Individuals from lower socioeconomic backgrounds may face financial barriers to accessing medical services, including routine check-ups, vaccinations, and preventative screenings. This lack of access can lead to delayed diagnosis and treatment of illnesses, potentially worsening health outcomes. Furthermore, the quality of care received may differ depending on socioeconomic status.
Lower socioeconomic status can also contribute to disparities in preventative care, with fewer opportunities for regular check-ups and screenings. This can lead to later detection of conditions, hindering timely interventions and potentially worsening the course of the disease.
The Role of Discrimination and Implicit Bias
Discrimination and implicit bias within the healthcare system contribute to the perpetuation of health disparities. Black individuals may experience implicit bias from healthcare providers, leading to misdiagnosis, inadequate treatment, and a lack of trust in the healthcare system. This lack of trust can further limit access to necessary care, exacerbating existing health problems. Furthermore, implicit biases can manifest in disparities in pain management and treatment, where Black patients may be less likely to receive adequate pain relief.
This can lead to chronic pain conditions and poorer overall health.
Correlation Between Socioeconomic Indicators and Health Issues
| Socioeconomic Indicator | Specific Health Issues in Black Communities |
|---|---|
| Poverty | Higher rates of chronic diseases (e.g., diabetes, hypertension), mental health issues, and premature mortality. |
| Inadequate Housing | Increased risk of respiratory illnesses (due to exposure to pollutants), infectious diseases, and trauma. |
| Food Insecurity | Nutritional deficiencies, obesity, and higher rates of chronic diseases (e.g., type 2 diabetes). |
| Limited Access to Healthcare | Delayed diagnosis and treatment of illnesses, poorer health outcomes, and higher rates of preventable hospitalizations. |
| Discrimination and Implicit Bias | Misdiagnosis, inadequate treatment, and lack of trust in the healthcare system, leading to poorer health outcomes. |
Access to Healthcare and Quality of Care

Black individuals face significant disparities in accessing and receiving quality healthcare, stemming from a complex interplay of historical injustices, socioeconomic factors, and systemic biases. These disparities contribute to poorer health outcomes and exacerbate existing health inequities. Understanding these challenges is crucial to developing effective solutions and promoting equitable healthcare for all.
Disparities in Access to Healthcare Services
Historical and ongoing systemic racism has created profound barriers to healthcare access for Black communities. These barriers manifest in various forms, including limited insurance coverage, geographic location, and implicit biases within the healthcare system. Access to primary care, preventative services, and specialized care often differs significantly between Black and other racial groups.
- Limited insurance coverage: Many Black individuals, due to socioeconomic factors and historical discrimination, lack access to comprehensive health insurance, making preventative care and routine check-ups more challenging. This is particularly acute in communities with lower incomes and limited employment opportunities.
- Geographic location: Access to healthcare providers and facilities varies greatly across geographic regions. Black communities, often concentrated in areas with fewer healthcare providers, face longer travel times and reduced access to specialized care, impacting their ability to receive timely and appropriate medical attention.
- Implicit bias: Studies have shown that implicit bias can affect the quality of care received by Black patients. This can manifest in underdiagnosis, delayed treatment, and inadequate pain management, which often leads to poorer health outcomes.
Challenges Faced by Black Patients in Navigating the Healthcare System
Navigating the healthcare system can be exceptionally challenging for Black patients, who may encounter obstacles due to language barriers, cultural differences, and a lack of trust in the system. Communication breakdowns and misunderstandings can lead to inappropriate treatment and exacerbate existing health disparities.
- Language barriers: In some communities, language barriers can create difficulties in communicating medical needs and understanding treatment plans, potentially resulting in misdiagnosis and poor health outcomes. Cultural competency training for healthcare providers is crucial to address this.
- Cultural differences: Cultural differences in healthcare practices and beliefs can also create communication challenges. Black communities have unique healthcare traditions and expectations, which should be considered to ensure culturally sensitive care.
- Lack of trust: Historical mistreatment and discrimination within the healthcare system can foster a lack of trust between Black patients and healthcare providers. Building trust and rapport is essential to ensure open communication and effective treatment.
Comparison of Quality of Care
Studies have shown that Black patients, compared to other racial groups, often receive lower-quality care, including delayed diagnoses, less aggressive treatment for certain conditions, and higher rates of adverse events. This disparity highlights the need for ongoing efforts to address implicit bias and promote equitable healthcare practices.
Geographic Variations in Healthcare Access and Quality
Geographic location significantly impacts access to healthcare services and the quality of care received by Black populations. Differences in provider density, availability of specialized care, and access to preventative services contribute to disparities in health outcomes.
| Geographic Region | Healthcare Access (Black Population) | Quality of Care (Black Population) | Notes |
|---|---|---|---|
| Rural Southern States | Lower | Lower | Limited provider density, increased travel time, and reduced access to specialized care. |
| Urban Northern Cities | Higher | Mixed | Potential for higher provider density but challenges related to language barriers and trust. |
| Coastal Areas | Variable | Variable | Access depends on specific communities and socioeconomic factors within the region. |
“Racial and ethnic disparities in healthcare are not simply the result of individual choices or behaviors, but are rooted in systemic inequities that perpetuate health disparities across generations.”
Specific Health Issues Affecting Black Communities

The disproportionate burden of chronic diseases, maternal health disparities, and mental health challenges within the Black community highlight critical areas requiring urgent attention and intervention. These disparities are rooted in complex social determinants of health, including historical injustices, systemic racism, and socioeconomic factors. Understanding these specific health issues is crucial for developing targeted and effective strategies to improve health outcomes and reduce health inequities.The heightened vulnerability of Black individuals to various health conditions is a stark reality.
Factors such as access to quality healthcare, socioeconomic status, and environmental influences all play a significant role in shaping health outcomes. This necessitates a multifaceted approach that addresses the root causes of these disparities, alongside targeted interventions focused on prevention, early detection, and effective treatment.
Chronic Disease Burden
Chronic diseases, including hypertension, diabetes, and cardiovascular disease, pose a significant threat to the well-being of Black communities. These conditions often manifest earlier and with greater severity in this population compared to other groups. The interplay of genetic predisposition, lifestyle choices, and environmental factors contributes to this elevated risk. Addressing these conditions requires a comprehensive approach encompassing lifestyle modifications, preventative screenings, and accessible, culturally competent healthcare.
Maternal Mortality and Morbidity
Black women experience significantly higher rates of maternal mortality and morbidity compared to their white counterparts. This disparity is rooted in factors such as systemic racism, implicit bias in healthcare settings, socioeconomic disparities, and access to quality prenatal care. Furthermore, existing health conditions and complications during pregnancy may not be adequately addressed, contributing to adverse outcomes. Addressing this critical issue requires comprehensive strategies that include culturally sensitive prenatal care, increased access to specialized maternal care, and addressing the underlying socioeconomic factors that contribute to this disparity.
Mental Health Disparities
Mental health disparities within the Black community are substantial. The impact of historical trauma, systemic racism, and socioeconomic challenges on mental well-being is undeniable. These factors often lead to higher rates of stress, anxiety, and depression in Black individuals. This necessitates culturally sensitive mental health services, accessible resources, and support systems that acknowledge the unique experiences and challenges faced by the community.
Prevalence of Specific Diseases and Conditions
| Demographic Subgroup | Hypertension | Diabetes | Cardiovascular Disease | Maternal Mortality Rate | Mental Health Conditions (e.g., Depression, Anxiety) |
|---|---|---|---|---|---|
| Black Men | Higher | Higher | Higher | Lower (compared to Black Women) | Higher |
| Black Women | Higher | Higher | Higher | Higher | Higher |
| Black Children | Increasing trend | Increasing trend | Increasing trend | Lower (compared to Black Adults) | Higher (relative to other groups) |
Note: Data on specific prevalence rates for each condition within various subgroups of the Black community can be found in the literature from the CDC, NIH, and other reputable sources. This table represents a general overview and should not be considered a definitive statistical analysis. Further research is needed to obtain precise prevalence figures for each subgroup.
Cultural Factors and Health Practices
Cultural beliefs and practices profoundly influence health decisions and outcomes within Black communities. These deeply ingrained traditions, often passed down through generations, can significantly impact how individuals perceive health, illness, and appropriate treatment. Understanding these nuances is crucial for healthcare providers to offer culturally competent care that respects individual beliefs and promotes positive health outcomes. These factors, often intertwined with socioeconomic realities, can create barriers or facilitate access to healthcare, affecting both preventative measures and responses to illness.
The Influence of Cultural Beliefs on Health Decisions
Cultural beliefs significantly impact health decisions, shaping how individuals perceive health issues, seek care, and respond to treatment. Family involvement and decision-making are often central to these processes. Trust in healthcare providers, which is influenced by historical and contemporary experiences, can also play a crucial role in shaping a patient’s comfort level and willingness to engage with the medical system.
Cultural norms around preventative care, such as dietary habits and lifestyle choices, also play a significant part in shaping health outcomes.
Cultural Factors Influencing Health Behaviors
Cultural norms significantly influence health behaviors. Dietary traditions, for example, can lead to increased risk of certain conditions if not aligned with nutritional guidelines. Spiritual beliefs and practices can influence how individuals cope with stress and illness, impacting both mental and physical well-being. Traditional healing practices, while often valuable in addressing immediate needs, may sometimes conflict with modern medical approaches, creating potential challenges for integration into comprehensive care plans.
The ongoing struggle for Black health matters is a crucial humanity issue. We see devastating statistics like alcohol-related deaths doubling in the last two decades, a stark reminder of the complex challenges faced by communities. This alarming trend, as detailed in the article alcohol related deaths double in two decades , highlights the need for more comprehensive strategies to address underlying societal factors and improve health outcomes for all, particularly within the Black community.
It’s a multifaceted problem that demands a holistic approach to truly tackle the issue.
These cultural influences, when not considered, can create barriers to effective healthcare.
Cultural Factors Affecting Access to Care
Cultural factors can also influence access to healthcare. Language barriers, distrust of the medical system, and concerns about cultural sensitivity can all contribute to reluctance in seeking or engaging with healthcare services. The perception of confidentiality, the role of family in healthcare decisions, and the importance of certain rituals or practices can also influence how patients interact with the healthcare system.
Addressing these issues requires cultural sensitivity and an understanding of diverse experiences.
Cultural Sensitivity in Improving Health Outcomes
Cultural sensitivity is paramount in improving health outcomes for Black patients. This involves acknowledging and respecting diverse cultural beliefs and practices, ensuring that communication is effective and respectful, and adapting healthcare delivery to meet the specific needs of the community. Employing culturally competent healthcare providers, offering culturally appropriate materials, and providing language assistance are key components of this approach.
Active listening, empathy, and open communication are crucial in fostering trust and rapport with patients from diverse backgrounds.
Table: Influence of Cultural Beliefs on Healthcare Preferences and Practices
| Cultural Belief | Healthcare Preference | Healthcare Practice |
|---|---|---|
| Importance of family involvement in healthcare decisions | Patient prefers family members to be involved in all discussions and decisions | Healthcare providers should actively include family members in patient care plans. |
| Traditional healing practices are valued | Patient may prefer complementary or alternative therapies alongside conventional treatments. | Healthcare providers should inquire about and understand the patient’s use of traditional healing practices to ensure appropriate integration. |
| Distrust of the healthcare system due to historical experiences | Patient may be hesitant to engage with healthcare providers. | Healthcare providers should build trust by demonstrating cultural sensitivity, active listening, and transparency. |
| Specific dietary traditions | Patient’s diet may differ from recommended guidelines. | Healthcare providers should tailor dietary recommendations to respect the patient’s cultural practices, while ensuring nutritional adequacy. |
Public Health Interventions and Policies
Addressing health disparities among Black populations requires a multifaceted approach that goes beyond individual interventions. Public health interventions and policies play a crucial role in creating systemic change and promoting health equity. These initiatives must consider the complex interplay of historical, socioeconomic, and environmental factors that contribute to these disparities. Effective policies and programs are essential to dismantling systemic barriers and fostering healthier communities.
Existing Public Health Interventions
Various public health interventions are currently employed to address health disparities among Black populations. These initiatives often target specific health issues, such as maternal mortality, cardiovascular disease, and cancer, recognizing the disproportionate burden of these illnesses within the community. Interventions may include community-based health education programs, targeted screening initiatives, and culturally appropriate outreach strategies. For example, community health workers trained in cultural competency are vital in connecting individuals with resources and fostering trust.
Effectiveness of Interventions
The effectiveness of public health interventions in improving health outcomes for Black populations varies. While some interventions have demonstrated positive impacts, others have faced limitations due to factors such as limited resources, inadequate community engagement, and persistent systemic inequities. Evaluation of these programs is critical for understanding their strengths and weaknesses and informing future interventions. Furthermore, evaluating the effectiveness must include long-term follow-up to capture the full impact of interventions.
Need for Policy Changes
Policy changes are essential to address the root causes of health disparities and foster health equity. These policies must consider the historical context of racism and discrimination, which have shaped health outcomes and access to resources. Moreover, policies must address socioeconomic factors, such as poverty and lack of access to quality education, which exacerbate health disparities. Policymakers must prioritize data collection and analysis to identify and track disparities, allowing for evidence-based policy development.
Table of Existing Policies and Programs
| Policy/Program | Description | Examples of Impact |
|---|---|---|
| Healthy Start Programs | These programs provide comprehensive support for pregnant women and new mothers, including prenatal care, nutrition education, and breastfeeding support. | Reduced maternal mortality rates in some communities, improved birth outcomes, and increased breastfeeding rates. |
| Community Health Centers | These centers provide primary care, preventive services, and social support to underserved communities. | Improved access to healthcare, reduced chronic disease rates, and enhanced health literacy among patients. |
| Affordable Care Act (ACA) | The ACA expanded health insurance coverage, making healthcare more accessible to millions. | Increased access to preventative care and treatment for chronic conditions. |
| Targeted Funding for Research | Increased funding for research focused on health disparities among Black populations. | Identifying effective strategies for prevention and treatment, creating new resources for better health. |
The Impact of Environmental Factors on Black Health
Environmental factors play a significant role in shaping health disparities, and Black communities are disproportionately affected by environmental hazards. This vulnerability stems from a complex interplay of historical injustices, socioeconomic factors, and systemic inequities. Understanding these impacts is crucial to developing effective public health interventions and policies aimed at promoting health equity.Environmental injustices, such as the placement of polluting industries near predominantly Black neighborhoods, have created a legacy of adverse health outcomes.
These communities often lack the resources to advocate for their environmental rights and challenge these inequities, exacerbating existing health disparities.
Environmental Hazards and Pollution in Black Communities
Historically, marginalized communities, including Black communities, have been disproportionately exposed to environmental hazards. This is often due to the placement of polluting industries, landfills, and other environmentally hazardous sites in their neighborhoods. These locations, often lacking political power and resources, are less likely to successfully resist such placements. This unequal distribution of environmental hazards contributes significantly to health disparities.
Environmental Injustices Experienced by Black Populations
Environmental injustices take many forms, affecting Black communities in profound ways. One example is the disproportionate presence of polluting facilities near Black neighborhoods. This proximity exposes residents to higher levels of air and water pollution, leading to increased rates of respiratory illnesses, cardiovascular diseases, and other health problems. Moreover, limited access to clean water and sanitation further exacerbates these disparities.
These environmental injustices contribute to the cycle of poverty and poor health within these communities.
Link Between Environmental Factors and Chronic Diseases
Environmental exposures have a strong correlation with chronic diseases that disproportionately affect Black communities. For instance, exposure to air pollution, including particulate matter and other toxic substances, has been linked to increased rates of asthma, cardiovascular disease, and lung cancer. Similarly, contaminated water sources can lead to various waterborne illnesses. These environmental factors contribute to the higher prevalence of chronic diseases in Black communities.
Influence of Environmental Factors on Health Outcomes
The table below illustrates how environmental factors can influence health outcomes in Black communities.
| Environmental Factor | Health Outcome | Example |
|---|---|---|
| Proximity to polluting industries | Increased respiratory illnesses | A community near a chemical plant experiences higher rates of asthma and bronchitis. |
| Lack of access to green spaces | Reduced physical activity and increased stress | A neighborhood with limited parks and recreational areas results in lower levels of physical activity and higher stress levels. |
| Exposure to contaminated water sources | Waterborne diseases and other health problems | A community using contaminated water sources experiences higher rates of gastrointestinal illnesses and other health complications. |
| Exposure to lead-contaminated soil | Neurological damage and developmental problems | Children in a neighborhood with lead-contaminated soil may experience learning disabilities, behavioral problems, and other developmental issues. |
Intersectionality and Black Health
Intersectionality recognizes that social identities like race, gender, sexual orientation, and socioeconomic status interact in complex ways to shape health outcomes. Understanding these intersections is crucial for developing effective policies and interventions that address the unique challenges faced by specific subgroups within the Black community. Ignoring these nuances can lead to ineffective or even harmful approaches.The concept of intersectionality highlights that experiences of discrimination and marginalization are not monolithic.
A Black woman, for example, faces different health challenges than a Black man, or a Black LGBTQ+ individual. These differences arise from the combined effects of various forms of oppression and privilege. Recognizing these intersections is essential for creating a more equitable and just healthcare system.
Intersection of Gender and Race in Black Health
Gender significantly influences health outcomes for Black women and men. Black women, for example, often face disparities in maternal health, experiencing higher rates of maternal mortality and morbidity than their White counterparts. This disparity is often exacerbated by systemic racism and socioeconomic factors. The combination of racial and gender discrimination can create a unique set of challenges in accessing healthcare and navigating the healthcare system.Black men also face unique health challenges.
They are disproportionately affected by certain diseases, such as cardiovascular disease and prostate cancer. These health disparities can be attributed to a combination of socioeconomic factors, such as limited access to healthy food options and lack of resources, as well as the impact of implicit bias within the healthcare system.
Intersection of Sexual Orientation and Race in Black Health
Black individuals who identify as LGBTQ+ often face additional layers of discrimination and marginalization. They may experience discrimination from both the LGBTQ+ and Black communities, leading to unique stressors and health challenges. These compounded factors can result in higher rates of mental health issues, substance abuse, and HIV/AIDS among Black LGBTQ+ individuals. Intersectionality in this case emphasizes that policies and interventions must be inclusive and address the specific needs of Black LGBTQ+ individuals.
Addressing black health disparities is a crucial human issue. Taking proactive steps like making healthy lifestyle choices, like cutting out 200 calories a day and exercising, can significantly contribute to better heart health. This article offers more insights. Ultimately, prioritizing health and well-being for all communities is essential for a healthier future.
Intersection of Socioeconomic Status and Race in Black Health
Socioeconomic status plays a significant role in shaping health outcomes for all populations, but it interacts profoundly with race to create unique challenges for Black individuals. Black communities often experience higher rates of poverty, limited access to quality education and employment opportunities, and exposure to environmental hazards. These factors can result in poorer health outcomes, including higher rates of chronic diseases and premature mortality.
Impact of Multiple Social Identities on Black Health
| Social Identity | Potential Health Impacts | Examples |
|---|---|---|
| Black Women | Higher rates of maternal mortality, poorer reproductive health outcomes, higher rates of certain cancers. | Disparities in access to prenatal care, implicit bias in medical decision-making. |
| Black Men | Higher rates of cardiovascular disease, prostate cancer, and certain types of cancer. | Limited access to preventative care, environmental factors contributing to health problems. |
| Black LGBTQ+ Individuals | Higher rates of mental health issues, substance abuse, HIV/AIDS, discrimination in healthcare. | Stigma from both Black and LGBTQ+ communities, lack of culturally competent healthcare. |
| Black Individuals with Low Socioeconomic Status | Higher rates of chronic diseases, premature mortality, limited access to healthy food, lack of preventative care. | Exposure to environmental hazards, limited access to quality education and employment opportunities. |
This table illustrates the complex interplay of social identities and their impact on health outcomes for Black individuals. It highlights the necessity of addressing the unique needs of different subgroups within the Black community.
Policy and Intervention Considerations
Policies and interventions aimed at improving Black health must consider the intersections of race, gender, sexual orientation, and socioeconomic status. Culturally competent healthcare providers, tailored interventions, and community-based programs are essential to address the root causes of these disparities. A one-size-fits-all approach is inadequate. Acknowledging and addressing the unique needs of specific subgroups within the Black community is crucial for creating effective change.
The struggles of Black health are a critical human issue, impacting countless lives. It’s a systemic problem, and stories like Randy Travis’s long journey back, documented in Randy Travis’s long road back , highlight the complexities of health disparities and resilience. Ultimately, these personal narratives underscore the broader need for equitable access to healthcare and resources for all communities.
Data and Research on Black Health: Black Health Matters Humanity Issue
Understanding the health disparities faced by Black communities requires a robust foundation of data and research. Without meticulous data collection and analysis, effective interventions and policies aimed at improving health outcomes remain elusive. This critical need for evidence-based information fuels the importance of examining existing research and its limitations. Recognizing these limitations allows for the development of more robust and inclusive research methodologies in the future.Data on Black health is crucial for identifying specific challenges, understanding root causes, and tracking progress towards health equity.
This comprehensive approach ensures that interventions are targeted and effective, ultimately improving the health and well-being of Black individuals and communities. Analysis of this data, coupled with understanding of socioeconomic factors and historical context, provides a clearer picture of the complex interplay of factors influencing health outcomes.
Importance of Data Collection and Research
Rigorous data collection and research are essential for understanding and addressing health disparities within Black communities. This systematic approach to data gathering enables the identification of specific health issues and the development of tailored interventions. This, in turn, empowers policymakers and healthcare providers to implement targeted strategies that lead to better health outcomes for Black populations. Data-driven insights are critical for informing public health initiatives and ensuring that resources are allocated effectively.
Examples of Existing Data and Research
Numerous studies have highlighted the significant health disparities affecting Black communities. For instance, research consistently demonstrates higher rates of chronic diseases like hypertension and diabetes in Black populations compared to other racial groups. These findings underscore the need for preventative care and targeted interventions to address these disparities. Studies often analyze socioeconomic factors such as income inequality and access to quality healthcare to explain these observed differences.
Limitations of Current Data and Research Methods
Current data and research methods on Black health often suffer from limitations, including potential biases in study design, sampling, and data interpretation. These biases can lead to inaccurate or incomplete portrayals of the experiences and health outcomes of Black individuals. Addressing these limitations requires a commitment to inclusive research methodologies that consider the complex interplay of social determinants of health.
This necessitates researchers to be mindful of their own biases and actively seek diverse perspectives to improve the validity and reliability of their findings.
Available Data Sources and Research Findings
| Data Source | Specific Black Health Issue | Key Research Findings |
|---|---|---|
| National Health Interview Survey (NHIS) | Chronic Disease Prevalence | Higher rates of hypertension and diabetes among Black adults compared to other racial groups. Data also reveals disparities in access to preventive care. |
| Centers for Disease Control and Prevention (CDC) data on mortality rates | Infant Mortality Rates | Infant mortality rates are consistently higher among Black infants compared to other racial groups, highlighting disparities in maternal and child health. Factors such as access to prenatal care and socioeconomic status are often correlated with these differences. |
| Academic research publications | Mental Health | Studies have shown disproportionate rates of mental health conditions, such as depression and anxiety, within Black communities. These studies also highlight the challenges in accessing mental health services. |
Final Wrap-Up
In conclusion, black health matters humanity issue is a complex and multifaceted problem requiring a multifaceted approach. Addressing historical injustices, socioeconomic factors, access to healthcare, cultural sensitivity, environmental concerns, and intersectional challenges are all crucial steps in fostering a healthier future for Black communities. Data collection and research are essential for understanding the specific needs and developing effective interventions.
Ultimately, promoting health equity for all requires a commitment to systemic change, policy reform, and a profound shift in societal attitudes and practices.
