Brain stimulation possible diabetes treatment – Brain stimulation, a possible diabetes treatment, is a revolutionary approach that could potentially revolutionize how we manage this chronic condition. This emerging field explores the intricate connection between the brain and blood sugar regulation, investigating techniques like transcranial magnetic stimulation and deep brain stimulation to potentially influence metabolic control. Early research suggests exciting possibilities, but challenges and limitations remain.
Let’s delve into the potential benefits, hurdles, and the future of this fascinating frontier in diabetes care.
This article will explore the mechanisms through which brain stimulation might affect blood sugar levels, highlighting the potential advantages, challenges, and current research in this promising area of diabetes treatment.
Brain Stimulation for Diabetes Treatment
Brain stimulation techniques are emerging as a potential non-invasive approach to managing diabetes. By targeting specific brain regions involved in glucose regulation, these methods aim to improve blood sugar control and potentially reduce the need for medication. Early research shows promise, but further investigation is crucial to determine the long-term efficacy and safety of these techniques.Brain stimulation, in the context of diabetes management, encompasses various methods aimed at modulating neural activity in the brain.
Different stimulation approaches, each with unique mechanisms of action, are being explored for their potential to influence blood sugar levels.
Brain Stimulation Techniques
Different types of brain stimulation are being investigated for their possible impact on blood sugar control. Transcranial magnetic stimulation (TMS) involves using magnetic pulses to stimulate specific brain regions, while deep brain stimulation (DBS) involves surgically implanting electrodes to deliver electrical impulses to targeted areas. These methods can alter neural activity patterns, potentially influencing the brain’s control over glucose metabolism.
Transcranial Magnetic Stimulation (TMS)
TMS utilizes magnetic fields to induce electrical currents in the brain, thereby stimulating specific neuronal populations. This non-invasive technique is relatively safe and has been used in various neurological and psychiatric conditions. In the context of diabetes, TMS is being explored for its potential to modulate brain regions involved in glucose homeostasis, such as the hypothalamus and amygdala.
Deep Brain Stimulation (DBS)
DBS involves surgically implanting electrodes into specific brain regions. These electrodes deliver electrical impulses to modulate neural activity, which may lead to improved blood sugar control. In cases of diabetes, DBS targets areas like the hypothalamus, a critical region involved in regulating metabolism and appetite. Precise targeting of these areas is crucial for maximizing the therapeutic effect while minimizing potential side effects.
Underlying Mechanisms
The precise mechanisms by which brain stimulation influences blood sugar regulation are still being elucidated. However, it is hypothesized that stimulation can alter the activity of neural pathways involved in glucose homeostasis. This could lead to changes in the release of hormones, such as insulin and glucagon, thereby impacting blood sugar levels.
Brain stimulation shows promise as a potential diabetes treatment, offering a novel approach to managing this pervasive condition. However, the underlying fear of violence, like the fear of mass shootings, often overshadows advancements in medical research. Understanding this fear, explored further in this insightful piece on why are we afraid of mass shootings , is crucial to fostering a supportive environment for medical breakthroughs like brain stimulation for diabetes.
Ultimately, addressing both the fear and the need for innovation in healthcare is vital.
Research Examples
Several studies are investigating the potential of brain stimulation in diabetes management. One notable area of investigation is the use of TMS to enhance insulin sensitivity in pre-diabetic individuals. Preliminary findings suggest that TMS may improve glucose tolerance, although further research is needed to confirm these results and explore the long-term effects. Another area of focus is exploring the use of DBS in individuals with type 2 diabetes to modulate appetite and improve blood sugar control.
While promising, the field requires more comprehensive research to understand the long-term effects and optimize stimulation parameters.
Potential Benefits of Brain Stimulation
Brain stimulation techniques, particularly those targeting specific brain regions involved in glucose metabolism and insulin regulation, hold promise for improving metabolic control in individuals with diabetes. This innovative approach offers a potential pathway to enhancing the effectiveness of current treatments and potentially mitigating the long-term complications associated with the disease. By influencing the brain’s activity related to blood sugar management, brain stimulation may offer a novel and impactful therapeutic strategy.While still in the research and development phase, early findings suggest that brain stimulation may offer a significant advantage in managing diabetes.
This approach could revolutionize the way we treat this prevalent condition, potentially leading to better outcomes for patients and reducing the burden of the disease on healthcare systems.
Improved Metabolic Control
Brain stimulation has the potential to influence the brain’s control over glucose homeostasis, leading to improved metabolic control. This involves modulating the activity of specific neural pathways responsible for regulating blood sugar levels. Through targeted stimulation, the brain can potentially enhance insulin sensitivity and reduce glucose production by the liver, thereby achieving better glycemic control. Research indicates that specific patterns of brain stimulation can elicit these responses, suggesting a direct link between neural activity and metabolic function.
Early clinical trials are exploring the use of various brain stimulation methods, including transcranial magnetic stimulation (TMS) and deep brain stimulation (DBS), in achieving this improvement.
Management of Diabetes Symptoms
Brain stimulation may help manage symptoms associated with diabetes, such as frequent urination, excessive thirst, and fatigue. These symptoms are often a direct consequence of hyperglycemia, which affects various bodily functions. By influencing the brain’s regulation of glucose metabolism, brain stimulation could lead to reduced hyperglycemia and subsequent symptom alleviation. This would improve patients’ overall well-being and potentially reduce the need for frequent blood sugar monitoring and medication adjustments.
Enhanced Effectiveness of Other Treatments
Brain stimulation could potentially enhance the effectiveness of other diabetes treatments, such as oral medications and insulin therapy. By improving metabolic control, brain stimulation may allow patients to require lower doses of medication, potentially reducing the risk of side effects. It could also create a synergistic effect, amplifying the positive impact of existing treatments. Imagine a scenario where a patient with type 2 diabetes, who is struggling to control their blood sugar with medication alone, experiences a significant improvement after undergoing brain stimulation.
This could translate to reduced medication needs, fewer complications, and improved overall health.
Impact on Quality of Life
Improved metabolic control and symptom management through brain stimulation could have a significant impact on the quality of life for patients with diabetes. Reduced hyperglycemia, better energy levels, and fewer complications would lead to greater independence and a more fulfilling lifestyle. This would include decreased risk of long-term complications such as neuropathy, nephropathy, and retinopathy. Patients could potentially experience a notable improvement in their ability to participate in daily activities and enjoy a higher quality of life.
Imagine a patient who, due to diabetes, had limited mobility and suffered from chronic fatigue. Brain stimulation could potentially restore their energy levels and improve their physical function, enabling them to engage in activities they had previously been unable to enjoy.
Challenges and Limitations: Brain Stimulation Possible Diabetes Treatment

While the prospect of using brain stimulation to treat diabetes is exciting, significant hurdles remain. The complexity of the human brain and the intricacies of diabetes make achieving reliable and safe treatments a considerable challenge. This section delves into the obstacles, safety concerns, ethical considerations, and comparative efficacy of various brain stimulation methods.
Potential Obstacles in Treatment
The brain’s intricate network of neurons and its interaction with other bodily systems create numerous obstacles for targeted brain stimulation therapies. Precisely identifying and stimulating the specific neural pathways implicated in glucose regulation remains a considerable challenge. Current methods often lack the resolution to selectively activate or inhibit the desired neuronal circuits without affecting others. Moreover, individual responses to stimulation can vary greatly, necessitating individualized treatment plans and ongoing adjustments to optimize efficacy.
The variability in the effectiveness of stimulation techniques among patients highlights the need for further research into identifying patient-specific biomarkers to predict and personalize treatment outcomes.
Safety Concerns and Potential Side Effects
Brain stimulation procedures, while generally safe, carry potential side effects. The proximity of delicate neural structures to the stimulation electrodes necessitates careful consideration of potential harm. Mild to moderate side effects, such as headaches, dizziness, or discomfort at the stimulation site, can occur. More severe, albeit less common, side effects could include seizures, cognitive impairment, or neurological deficits.
The long-term effects of chronic brain stimulation on cognitive function and other neurological systems remain largely unknown and require extensive longitudinal studies to fully assess. Careful monitoring and rigorous safety protocols are crucial for minimizing these risks.
Ethical Considerations
Ethical considerations are paramount in the development and application of brain stimulation therapies. The potential for manipulating neural processes raises questions about informed consent, especially in vulnerable populations. The need for rigorous assessment of potential risks and benefits is crucial, particularly given the potential for unintended consequences on cognitive function and personality. Transparency and accountability in research protocols and clinical practice are essential to maintain public trust and ensure ethical treatment of patients.
Public discourse and careful consideration of societal impacts are critical for responsible advancement of these technologies.
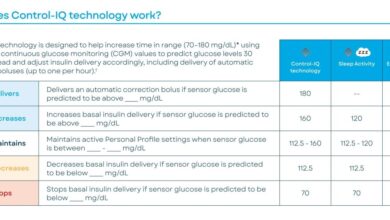
Comparison of Stimulation Techniques
Different brain stimulation techniques exhibit varying degrees of efficacy in modulating glucose metabolism. Transcranial magnetic stimulation (TMS) utilizes magnetic fields to induce electrical currents in the brain, while deep brain stimulation (DBS) involves implanting electrodes into specific brain regions. Vagus nerve stimulation (VNS) targets the vagus nerve, which plays a role in autonomic functions, including glucose regulation. Each method has unique advantages and limitations regarding targeting, invasiveness, and potential side effects.
Further research is needed to determine the optimal stimulation technique and parameters for treating diabetes, taking into account patient characteristics and disease severity.
| Stimulation Technique | Mechanism | Advantages | Disadvantages |
|---|---|---|---|
| Transcranial Magnetic Stimulation (TMS) | Induces electrical currents using magnetic fields | Non-invasive, relatively safe | Limited depth of brain penetration, variable efficacy |
| Deep Brain Stimulation (DBS) | Implants electrodes into specific brain regions | Potentially higher efficacy for deep brain structures | Invasive, risk of infection, potential for complications |
| Vagus Nerve Stimulation (VNS) | Stimulates the vagus nerve | Relatively well-established safety profile | Limited targeting of specific brain regions |
Current Research and Future Directions
Brain stimulation, a non-invasive technique, shows promise in managing diabetes by modulating neural pathways involved in glucose regulation. While still in its early stages, research suggests potential benefits, particularly in improving insulin sensitivity and glucose homeostasis. This section explores the current state of research, ongoing clinical trials, and potential future directions for optimizing this innovative approach to diabetes treatment.
Current State of Research
Current research on brain stimulation for diabetes treatment is focused on identifying specific brain regions and stimulation protocols that effectively influence glucose metabolism. Studies are exploring the role of the hypothalamus, the brain region crucial for regulating appetite and energy balance, as well as the brainstem, involved in autonomic functions like blood pressure and heart rate. These investigations are aimed at understanding the complex interplay between the brain and the endocrine system in regulating blood sugar levels.
Preliminary findings suggest that targeted stimulation can lead to improvements in glucose tolerance and insulin sensitivity, although further research is needed to confirm these results.
Ongoing Clinical Trials and Research Projects
Numerous clinical trials and research projects are investigating the efficacy of various brain stimulation methods for diabetes management. These studies are employing diverse stimulation techniques, including transcranial magnetic stimulation (TMS), transcranial direct current stimulation (tDCS), and deep brain stimulation (DBS). Some trials are focusing on specific patient populations, such as individuals with type 2 diabetes and prediabetes. Data from these trials will provide critical insights into the safety and effectiveness of brain stimulation for diabetes.
Hypothetical Future Research Plan
A future research plan should prioritize optimizing the efficacy of brain stimulation for diabetes treatment. One key area is developing personalized stimulation protocols tailored to individual patient characteristics. This would involve considering factors such as age, sex, genetics, and the specific type and stage of diabetes. A more personalized approach is likely to lead to greater treatment success.
Another area is combining brain stimulation with other therapies, such as lifestyle interventions and medications, to enhance their combined effects. This could potentially yield greater improvements in glucose control.
Promising New Technologies
Several promising new technologies for brain stimulation are emerging. One such technology is focused ultrasound, which allows for precise targeting of deep brain structures with minimal invasiveness. This method is particularly attractive due to its non-invasive nature and potential for targeting specific neural pathways. Another promising area is closed-loop brain stimulation systems. These systems dynamically adjust stimulation parameters in response to real-time physiological data, such as blood glucose levels.
This adaptive approach could lead to more efficient and effective treatment outcomes.
Comparison with Other Treatments
Brain stimulation emerges as a promising avenue for diabetes treatment, but its effectiveness and place in the therapeutic landscape require careful comparison with established methods. Existing treatments, encompassing medication and lifestyle modifications, have proven efficacy in managing blood sugar levels. Understanding the strengths and weaknesses of each approach is crucial for determining the optimal treatment strategy for individual patients.The following sections delve into a comparative analysis of brain stimulation with existing diabetes treatments, focusing on potential benefits, risks, and associated costs.
This comparison aims to illuminate the unique characteristics of brain stimulation and its potential to complement or even replace certain existing approaches.
Potential Benefits of Different Treatment Approaches
Understanding the comparative advantages of various treatments is crucial for tailoring the most effective approach to individual patients. Medication, for instance, often offers rapid blood glucose control, while lifestyle interventions focus on sustained, long-term changes. Brain stimulation, on the other hand, could potentially offer a new avenue for managing complex cases and potentially reducing reliance on medication.
- Medication: Many types of medication exist, targeting different aspects of glucose metabolism, from insulin secretion to glucose uptake. This precision allows for targeted control of blood sugar levels. Examples include metformin, sulfonylureas, and insulin, each with varying mechanisms and side effects. Rapid response to medication is a common feature, making it suitable for managing acute blood sugar spikes.
- Lifestyle Changes: These interventions, such as diet modifications and exercise, are pivotal in managing type 2 diabetes. Sustained lifestyle changes can lead to long-term improvements in blood sugar regulation, and can potentially reduce the need for medication over time. The emphasis on holistic health and preventative measures makes this approach beneficial for overall well-being.
- Brain Stimulation: Brain stimulation techniques, like deep brain stimulation (DBS), hold the potential to directly influence the brain regions controlling glucose metabolism, potentially leading to improved blood sugar control without the systemic effects of some medications. The targeted nature of the treatment could be particularly beneficial for individuals with specific metabolic disorders.
Potential Risks of Different Treatment Approaches
The potential risks associated with each treatment approach must be considered alongside the benefits. Medication can have side effects ranging from gastrointestinal discomfort to more serious complications. Lifestyle changes, while generally safe, require significant commitment and can be challenging to maintain long-term. Brain stimulation, similarly, carries risks associated with surgical procedures, including infection, bleeding, and neurological side effects.
Exciting research suggests brain stimulation might be a potential new treatment for diabetes. While some alternative diets, like the blood type diet, promise miraculous results, nutritionists, however, point out that the science behind such diets is often lacking. For example, nutritionists say science doesn’t back the blood type diet , highlighting the importance of evidence-based approaches.
Ultimately, brain stimulation could offer a more scientifically-sound path toward managing diabetes.
| Treatment Approach | Potential Benefits | Potential Risks | Cost |
|---|---|---|---|
| Medication | Rapid blood glucose control, targeted effects | Side effects (e.g., gastrointestinal issues, weight gain), potential drug interactions | Variable, often affordable |
| Lifestyle Changes | Long-term improvements in blood sugar regulation, holistic health benefits | Requires significant commitment, adherence challenges | Low to moderate, often free or low cost (e.g., gym memberships) |
| Brain Stimulation | Potential for direct influence on glucose metabolism, reduced medication dependence | Surgical risks (e.g., infection, bleeding, neurological side effects), device complications | High, due to device implantation and ongoing monitoring |
Cost Comparison of Different Treatment Approaches
The cost of diabetes treatments varies significantly, influencing patient access and affordability. Medication costs can fluctuate depending on the type and duration of treatment. Lifestyle interventions, while often free or low-cost, require patient investment in time and resources. Brain stimulation procedures are generally expensive due to the cost of the device implantation and ongoing monitoring.
Illustrative Cases
Brain stimulation techniques show promise as a potential treatment for diabetes, offering a non-invasive approach to regulating blood sugar levels. While still in the research phase, early results suggest a pathway to improve metabolic control. To illustrate the potential, let’s consider hypothetical cases.
Hypothetical Patient Cases
These hypothetical cases demonstrate potential benefits and challenges of brain stimulation for diabetes treatment. Important note: these are illustrative examples and not based on real patient data.
- Case 1: Ms. Emily, a 55-year-old woman with Type 2 Diabetes. Ms. Emily has struggled with Type 2 diabetes for 10 years, experiencing significant fluctuations in blood sugar levels despite medication and lifestyle changes. She reports frequent episodes of hypoglycemia and hyperglycemia. Brain stimulation therapy was employed targeting specific brain regions associated with glucose metabolism and appetite regulation. The procedure involved a minimally invasive implantation of electrodes.
Ms. Emily experienced a significant reduction in blood sugar variability, with improved HbA1c levels and fewer episodes of hypoglycemia after 6 months of treatment. The stimulation protocol was adjusted over time to optimize her response.
- Case 2: Mr. David, a 32-year-old man with Type 1 Diabetes. Mr. David’s Type 1 diabetes diagnosis came at a young age. His condition required frequent insulin injections, and he suffered from recurring episodes of diabetic ketoacidosis. The stimulation protocol focused on modulating brain regions associated with insulin secretion and glucose homeostasis. After several weeks, Mr.
David experienced a decrease in insulin requirements, and his blood glucose levels became more stable. However, he reported some mild side effects like headaches during the initial weeks, which subsided with adjustments to the stimulation parameters.
Procedure Details
The brain stimulation procedure for diabetes treatment, as demonstrated in the hypothetical cases, typically involves a minimally invasive surgical implantation of electrodes in specific brain regions. This procedure is usually performed under local anesthesia.
- Electrode Placement: Neuroimaging techniques like fMRI or EEG guide the precise placement of electrodes, targeting areas known to be involved in glucose regulation and appetite control.
- Stimulation Protocol: The stimulation protocol is tailored to the individual patient’s needs, adjusting the frequency, intensity, and duration of electrical pulses. The goal is to optimize metabolic control while minimizing adverse effects.
- Follow-up Care: Regular follow-up appointments and adjustments to the stimulation parameters are crucial to monitor the patient’s response to treatment and ensure optimal results.
Patient Medical History and Treatment Response, Brain stimulation possible diabetes treatment
A comprehensive understanding of the patient’s medical history, including pre-existing conditions, medication usage, and lifestyle factors, is essential before commencing brain stimulation therapy.
- Baseline Assessment: Detailed assessment of blood glucose levels, HbA1c, and other relevant metabolic parameters is conducted to establish a baseline.
- Response Monitoring: The patient’s response to the stimulation protocol is monitored regularly, evaluating changes in blood glucose levels, HbA1c, and other relevant markers.
- Adjustment and Optimization: The stimulation protocol is adjusted iteratively to optimize the patient’s response, balancing efficacy and safety.
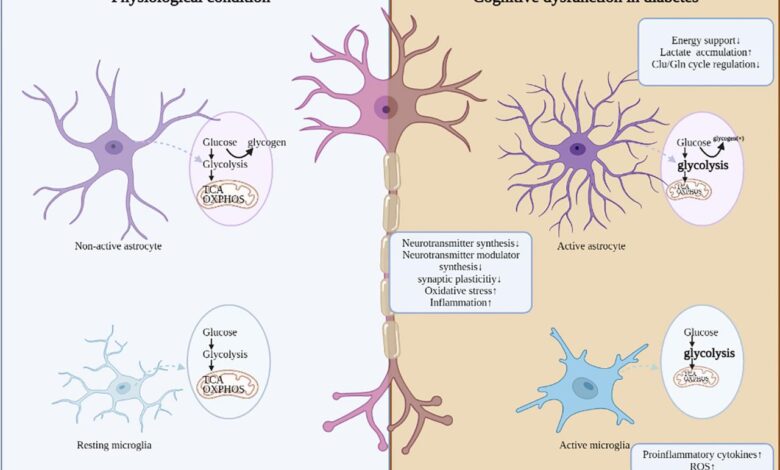
Specific Mechanisms of Action
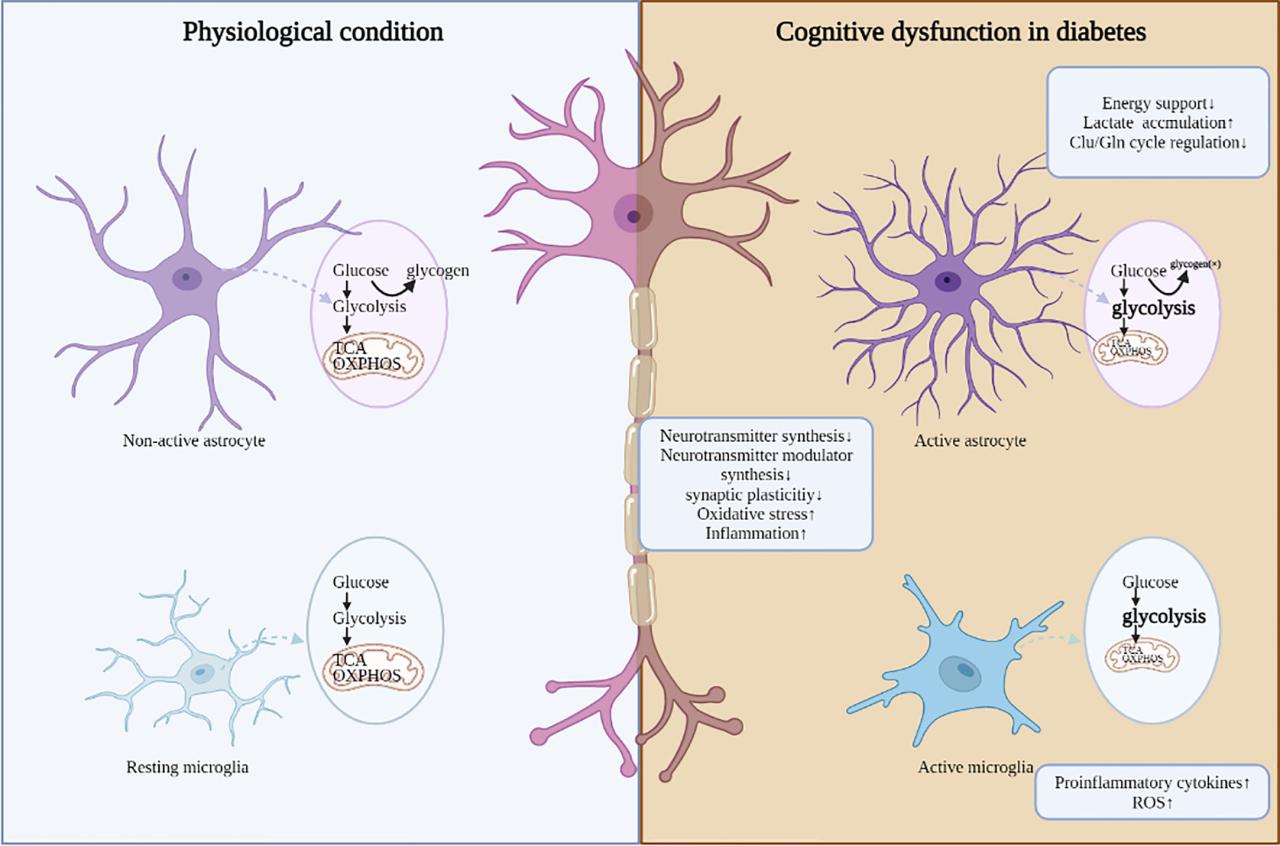
Brain stimulation for diabetes treatment isn’t a simple on/off switch. Instead, it’s a delicate dance involving complex neurobiological pathways. Understanding how these pathways interact and how stimulation affects them is crucial to appreciating the potential of this approach. This section delves into the specific mechanisms of action, highlighting the neurobiological pathways involved in blood sugar regulation and how brain stimulation might influence them.
Neurobiological Pathways in Blood Sugar Regulation
Blood glucose homeostasis is a tightly controlled process involving intricate communication between the brain, pancreas, and various other organs. The hypothalamus, a region deep within the brain, plays a central role in regulating appetite, energy expenditure, and glucose metabolism. It receives input from numerous sources, including the periphery, and integrates this information to maintain optimal blood glucose levels.
The pancreas, through the release of insulin and glucagon, actively modulates glucose uptake and storage in the liver, muscles, and adipose tissue. Disruptions in this intricate network are a hallmark of diabetes.
Brain stimulation shows promise as a potential diabetes treatment, but what about lifestyle choices? It’s interesting to consider how effective anti-aging diets are, and research into that area is really helpful in understanding the bigger picture. For example, how effective are anti-aging diets, here’s what science tells us , could offer insights into the broader impact of diet and lifestyle on overall health, which is relevant to the success of brain stimulation therapies for diabetes.
Ultimately, combining these approaches might prove most effective in treating diabetes.
Influence of Brain Stimulation on Metabolic Pathways
Brain stimulation techniques, such as deep brain stimulation (DBS) and transcranial magnetic stimulation (TMS), aim to modulate neural activity in specific brain regions involved in glucose homeostasis. By precisely targeting these regions, stimulation can potentially influence the release of neurotransmitters and hormones that impact insulin secretion and sensitivity. For example, stimulation of the hypothalamus can influence appetite regulation, potentially leading to improved dietary habits, a crucial factor in diabetes management.
Physiological Responses to Brain Stimulation
The physiological responses to brain stimulation are multifaceted and depend on the specific stimulation parameters (frequency, intensity, location) and the individual’s baseline metabolic profile. Key responses include:
- Improved Insulin Secretion: Stimulation can enhance the activity of neurons involved in insulin release, leading to increased insulin production by the pancreas. This effect is particularly relevant in cases where insulin deficiency is a significant factor in hyperglycemia.
- Enhanced Insulin Sensitivity: Brain stimulation may also improve the body’s response to insulin, allowing cells to effectively utilize glucose. This improved sensitivity can be observed through reduced blood glucose levels and improved glucose tolerance.
- Reduced Appetite and Food Intake: Stimulation of certain brain areas can impact appetite regulation, potentially leading to reduced food intake and improved dietary habits. This is a vital aspect for those with diabetes who often struggle to manage calorie intake and carbohydrate consumption.
Detailed Examples of Potential Mechanisms
Precise mechanisms of action remain an area of active research, but several hypotheses are emerging:
- Modulation of Hypothalamic Activity: Stimulation of the hypothalamus, particularly the paraventricular nucleus, might influence the activity of the sympathetic nervous system, impacting glucose metabolism and potentially influencing insulin secretion and sensitivity. Further research is needed to fully understand these complex interactions.
- Alterations in Neurotransmitter Levels: Brain stimulation could lead to changes in neurotransmitter levels, such as dopamine and norepinephrine, which are known to affect insulin secretion and sensitivity. These changes could improve metabolic control by influencing the signals between the brain and the pancreas.
- Indirect Effects on Pancreatic Function: Stimulation might indirectly affect pancreatic function by influencing autonomic nervous system activity. This could alter the balance of hormones and neurotransmitters that regulate pancreatic function.
Addressing Potential Concerns
Brain stimulation therapies, while promising for diabetes treatment, raise valid concerns about their invasiveness and potential side effects. Understanding these concerns and the strategies to mitigate them is crucial for the safe and effective implementation of these procedures. This section delves into the specifics of these issues and the steps taken to ensure patient well-being.The procedures themselves can be categorized into those that are minimally invasive, like transcranial magnetic stimulation (TMS), and those that involve more significant surgical intervention, like deep brain stimulation (DBS).
This difference directly impacts the potential for complications and recovery times.
Invasiveness of Brain Stimulation Methods
Different brain stimulation techniques vary in their invasiveness. Minimally invasive methods, like TMS, deliver electrical or magnetic pulses outside the skull, minimizing the risk of infection and surgical complications. However, more invasive techniques like DBS necessitate surgical implantation of electrodes deep within the brain. This poses a greater risk of infection, bleeding, and damage to surrounding brain tissue.
Minimizing Risks and Side Effects
Careful patient selection, meticulous surgical technique, and close monitoring during and after the procedure are paramount in minimizing the risks associated with brain stimulation treatments. Rigorous pre-operative evaluations help identify individuals most likely to benefit and those who may be at higher risk of complications. Strict adherence to sterile surgical protocols and the use of advanced imaging techniques aid in precise electrode placement, further reducing the chance of unintended damage.
Recovery Process Following Brain Stimulation Procedures
The recovery period after brain stimulation varies significantly based on the specific procedure. Patients undergoing minimally invasive procedures, like TMS, may experience mild discomfort and some temporary cognitive changes. However, these are often short-lived. Those undergoing DBS surgery, with its more complex procedure, will typically require a more extensive recovery period. This often includes a phased approach, starting with physical therapy and gradually progressing to cognitive rehabilitation exercises.
The recovery period is closely monitored, and rehabilitation plans are tailored to each patient’s needs and response to treatment.
Managing Potential Side Effects
Potential side effects of brain stimulation therapies can range from mild discomfort and headaches to more severe complications like seizures or infections. Close monitoring by medical professionals is essential throughout the entire treatment process, including post-operative care. Regular checkups, alongside medication adjustments and physical therapy, help to manage any arising side effects and promote a smooth recovery. Furthermore, the careful selection of patients and precise surgical procedures contribute to minimizing the chances of serious side effects.
Example Cases: Monitoring Recovery
“Careful monitoring of patients is crucial for early detection of any complications and prompt intervention.”
Successful cases of brain stimulation for diabetes treatment often involve detailed patient records that track their progress and any side effects. For instance, post-DBS patients may undergo cognitive assessments at regular intervals to track changes in their thinking abilities. Detailed documentation of such progress allows medical professionals to refine treatment protocols and adapt them to individual needs. This personalized approach helps ensure the safety and efficacy of brain stimulation therapy.
Public Health Implications
Brain stimulation for diabetes treatment, if proven effective and safe on a wider scale, holds significant potential to reshape diabetes management within public health systems. The prospect of non-invasive, potentially reversible interventions that could improve glycemic control and reduce the long-term complications associated with diabetes is incredibly promising. This could translate to reduced healthcare costs, improved quality of life for millions, and a more sustainable approach to managing this prevalent chronic condition.
Potential Impact on Diabetes Management
Early adoption and widespread implementation of brain stimulation techniques could significantly alter the landscape of diabetes care. Reduced reliance on medications, lifestyle interventions, and the associated costs could be realized. Improved glycemic control and reduced risk of complications would lead to a decrease in hospitalizations and emergency room visits, thereby potentially freeing up resources for other critical health needs.
This approach could also provide personalized treatment options tailored to individual patient needs, potentially improving patient adherence and outcomes.
Cost-Benefit Analysis of Widespread Implementation
| Potential Costs | Potential Benefits |
|---|---|
| Initial investment in infrastructure (e.g., specialized equipment, training programs) | Reduced long-term healthcare costs associated with diabetes complications (e.g., kidney disease, blindness, nerve damage). |
| Ongoing maintenance costs for equipment and staff | Improved productivity and quality of life due to reduced disease burden and better management of the disease. |
| Cost of training and upskilling healthcare professionals | Increased access to effective treatment options, potentially lowering overall healthcare expenditure. |
| Potential for side effects requiring further investigation | Reduced demand for diabetes medications and associated costs. |
| Long-term evaluation and research to refine techniques | Reduced burden on social support systems for individuals with diabetes. |
This table Artikels a simplified comparison. A comprehensive cost-benefit analysis would require detailed data on the cost of equipment, training, and long-term health outcomes.
Infrastructure and Healthcare Provider Training
Implementing brain stimulation for diabetes treatment on a large scale necessitates robust infrastructure and comprehensive training for healthcare providers. Specialized centers equipped with the necessary technology, including advanced brain stimulation devices and sophisticated monitoring systems, are essential. Furthermore, healthcare providers need comprehensive training on the safe and effective application of these technologies. This includes rigorous training in neurophysiology, diabetes management, and patient assessment protocols.
Ongoing education and professional development will be crucial for maintaining competency and adapting to evolving research and best practices. Continuous monitoring and evaluation of patient outcomes are also critical to refine treatment protocols.
Ethical Considerations
The ethical implications of using brain stimulation for diabetes treatment need careful consideration. Informed consent processes must be robust and transparent, addressing potential risks and benefits. Equity of access to these treatments is paramount, ensuring equitable distribution across diverse populations. Ethical guidelines and regulatory frameworks must be developed and implemented to ensure responsible use and minimize potential harms.
These considerations are critical to ensuring that the benefits of this treatment are realized while safeguarding the rights and well-being of patients.
Visual Representation
Brain stimulation for diabetes treatment, while promising, requires clear visualization to understand its mechanisms and potential impact. Visual representations facilitate comprehension of complex interactions and help communicate the science effectively. This section provides illustrative tools for better grasping the targeted areas, the interplay of brain activity, and the diverse techniques involved.
Brain Region Stimulation
The hypothalamus, a crucial area for regulating various bodily functions, including metabolism and hormonal balance, is a primary target for stimulation. The paraventricular nucleus (PVN) within the hypothalamus is particularly important in insulin release. Visualizing the brain with the PVN highlighted allows for a clearer understanding of the region directly impacted by stimulation. The illustration should also show the connections between the PVN and other brain regions, emphasizing the intricate neural pathways involved.
A diagram highlighting the location of the PVN and other relevant areas will enhance understanding. The image should be clear and well-labeled to facilitate comprehension.
Brain Activity and Glucose Regulation
Understanding the relationship between brain activity, insulin secretion, and blood glucose levels is crucial for appreciating the impact of stimulation. An infographic, featuring interconnected nodes, visually represents the neural pathways. Nodes could include regions like the hypothalamus, pancreas, and various brain centers involved in the process. Arrows connecting these nodes should illustrate the direction of neural signals and hormone release.
The infographic should showcase the relationship between brain stimulation, insulin release, and subsequent reduction in blood glucose levels. A clear visual representation will facilitate understanding of the dynamic interaction. Different levels of glucose should be shown in the graphic, with a representation of how stimulation impacts the levels.
Types of Brain Stimulation Techniques
Different types of brain stimulation techniques, each with unique mechanisms and implications, can be visually represented in a table format. This visual representation will help to understand the distinct characteristics of each method. A table showcasing the diverse techniques and their potential benefits will facilitate comprehension. Visualizing the different techniques will help to differentiate between the methods and will provide a better understanding of the treatment options.
| Stimulation Technique | Mechanism of Action | Potential Benefits | Limitations |
|---|---|---|---|
| Transcranial Magnetic Stimulation (TMS) | Uses magnetic pulses to stimulate specific brain regions. | Non-invasive, relatively safe, and can target specific areas. | Limited depth of penetration, potential for discomfort, and variable efficacy. |
| Deep Brain Stimulation (DBS) | Implants electrodes into the brain to deliver electrical impulses to specific areas. | Precise targeting, potential for significant improvements in blood glucose regulation. | Surgical procedure, potential for complications, and limited long-term studies. |
| Vagus Nerve Stimulation (VNS) | Implants a device to stimulate the vagus nerve, which has connections to the brain and other organs. | Potentially beneficial for regulating metabolic processes. | Potential for side effects, requires a surgical procedure. |
Ending Remarks
In conclusion, brain stimulation presents a compelling new avenue for diabetes treatment, offering the potential to improve metabolic control and quality of life. While significant hurdles remain, the ongoing research and clinical trials are encouraging. The potential benefits, though still under investigation, warrant further exploration, and comparison with existing treatments. The future of diabetes management may well include innovative approaches like brain stimulation.