Breast cancer treatments can increase risk of heart disease, presenting a complex interplay between battling cancer and safeguarding cardiovascular health. This exploration delves into the various treatments, their potential impact on the heart, and strategies to mitigate these risks. We’ll examine the mechanisms behind these effects, the role of individual factors, and ongoing research efforts to better understand and manage this intricate relationship.
Common breast cancer treatments, such as chemotherapy, radiation, and hormone therapy, can have significant effects on the cardiovascular system. Understanding these potential side effects is crucial for patients and healthcare providers to make informed decisions about treatment plans and to implement proactive measures for heart health.
Introduction to Breast Cancer Treatments and Potential Cardiovascular Risks: Breast Cancer Treatments Can Increase Risk Of Heart Disease
Breast cancer, a prevalent disease affecting women globally, is often treated with a range of modalities. While these treatments are crucial for survival, they can unfortunately have secondary effects, including potential cardiovascular complications. Understanding these risks is essential for patients and healthcare providers to make informed decisions regarding treatment options and long-term health management. The link between breast cancer treatments and cardiovascular health is a complex issue, and this discussion aims to explore the potential mechanisms and variations in risk based on treatment type and breast cancer subtype.The diverse range of breast cancer treatments, including surgery, chemotherapy, radiation, and hormone therapy, can impact the cardiovascular system through various mechanisms.
Some treatments directly damage the heart muscle or blood vessels, while others may lead to hormonal imbalances that increase the risk of cardiovascular disease. The type of breast cancer also plays a significant role in treatment strategies and associated risks. Understanding these intricacies allows for a more personalized approach to cancer care, minimizing potential long-term cardiovascular consequences.
Common Breast Cancer Treatments
Common breast cancer treatments include surgery (lumpectomy or mastectomy), chemotherapy, radiation therapy, and hormone therapy. These interventions aim to eliminate cancerous cells, but they may also affect healthy tissues, potentially increasing the risk of cardiovascular issues. The choice of treatment often depends on factors such as the stage of cancer, tumor characteristics, and the patient’s overall health.
Mechanisms of Cardiovascular Impact
Certain treatments, such as chemotherapy, can damage the heart muscle (cardiomyopathy) or blood vessels. Radiation therapy to the chest area may also contribute to cardiovascular issues. Furthermore, hormonal imbalances caused by some treatments may increase the risk of blood clots or high blood pressure, both significant risk factors for cardiovascular disease. Specific examples include chemotherapy-induced cardiomyopathy, a well-documented complication associated with certain chemotherapeutic agents, or the increased risk of thromboembolic events in some hormone therapies.
Breast Cancer Subtypes and Treatment Variations
Breast cancer presents in various subtypes, including luminal A, luminal B, HER2-positive, and triple-negative. Each subtype has different biological characteristics and responds differently to treatment. The choice of treatment approach varies accordingly. For instance, HER2-positive breast cancer often benefits from targeted therapies, which might have different cardiovascular risks compared to chemotherapy used in other subtypes.
Comparison of Treatment Modalities and Cardiovascular Impact
| Treatment Modality | Potential Impact on Heart Health | Examples of Risks |
|---|---|---|
| Surgery (lumpectomy/mastectomy) | Direct impact is minimal, but potential for complications from anesthesia or surgery. | Anesthesia-related cardiac events, surgical site infections, blood clots. |
| Chemotherapy | Can damage heart muscle (cardiomyopathy), increase blood pressure, and affect blood vessel health. | Chemotherapy-induced cardiomyopathy, hypertension, increased risk of heart attack. |
| Radiation Therapy | Radiation to the chest area can damage heart and blood vessels, increasing risk of heart failure or coronary artery disease. | Radiation-induced cardiomyopathy, coronary artery disease. |
| Hormone Therapy | Can cause hormonal imbalances, increasing risk of blood clots and high blood pressure. | Thromboembolic events, hypertension, dyslipidemia. |
Specific Treatment Impacts on Cardiovascular Health

Navigating breast cancer treatment often means confronting potential side effects, including cardiovascular complications. Understanding how different therapies can affect heart health is crucial for informed decision-making and proactive management. This section delves into the specific ways chemotherapy, hormonal therapies, radiation, and surgical approaches can impact the cardiovascular system.Different treatment modalities for breast cancer can exert varying degrees of stress on the cardiovascular system.
It’s fascinating how different health issues can be surprisingly interconnected. For example, breast cancer treatments can sometimes increase the risk of heart disease later on. Understanding the long-term effects of these treatments is crucial for patient well-being. This awareness is also important in light of recent developments, like the coronavirus lambda variant, which has prompted researchers to investigate potential links between viral infections and cardiovascular health.
What to know about the coronavirus lambda variant is a valuable resource for anyone looking to stay informed. Ultimately, the complex interplay between various health factors highlights the need for comprehensive and personalized care plans for all individuals.
A comprehensive understanding of these potential effects is essential for patients and healthcare providers to make informed choices, particularly when considering long-term implications.
Chemotherapy’s Cardiovascular Impact
Chemotherapy drugs, while effective in targeting cancer cells, can sometimes damage healthy cells, including those in the heart. Mechanisms like direct toxicity, oxidative stress, and inflammation can contribute to cardiotoxicity. For instance, certain anthracyclines are known to cause cardiomyopathy, a condition that weakens the heart muscle. Specific examples of chemotherapy regimens associated with increased cardiovascular risk include those incorporating anthracyclines and taxanes.
Careful monitoring of cardiac function during and after chemotherapy is critical to mitigate these risks.
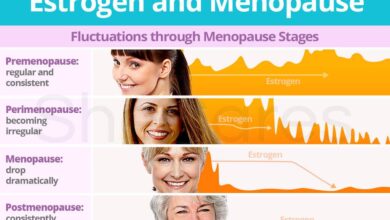
Hormonal Therapy and Cardiovascular Health, Breast cancer treatments can increase risk of heart disease
Hormonal therapies, used to block the effects of estrogen or other hormones on cancer growth, can also influence lipid profiles and blood pressure. For example, aromatase inhibitors can lead to elevated LDL (“bad”) cholesterol levels and reduced HDL (“good”) cholesterol levels. Changes in lipid profiles, if left unmanaged, may increase the risk of atherosclerosis, a condition characterized by plaque buildup in the arteries.
Furthermore, some hormonal therapies can affect blood pressure regulation.
Recent studies highlight a concerning link between breast cancer treatments and an increased risk of heart disease. This is a critical area of research, and the struggles of individuals facing cancer are often amplified by such side effects. For example, the stories of the Google China founders battling cancer, as detailed in this article google china founders battle with cancer , underscore the complex health challenges that can arise.
Ultimately, understanding these intertwined risks is vital for better patient care and preventative strategies.
Radiation Therapy and Cardiac Risk
Radiation therapy, while crucial for localized breast cancer treatment, can potentially damage the heart, particularly if the radiation beam directly targets the heart or if the dose is high. The risk is directly related to the location of the tumor and the radiation dose. Radiation therapy directed at the chest, especially close to the heart, carries a higher risk of heart damage.
The extent of this risk depends on factors like the total radiation dose and the duration of treatment.
Surgical Approaches and Cardiovascular Risk
Surgical approaches for breast cancer, including mastectomies and lumpectomies, carry potential cardiovascular risks, although these risks are often lower than those associated with chemotherapy or radiation. For example, some surgical procedures may involve significant blood loss, which could lead to temporary cardiac stress. In addition, extensive chest wall surgery, particularly involving the heart’s immediate vicinity, could have long-term implications for cardiac function.
The cardiovascular risks associated with different surgical approaches can vary depending on the extent of the procedure and the patient’s pre-existing health conditions.
Comparison of Treatment Risks
| Treatment Type | Potential Short-Term Cardiovascular Risks | Potential Long-Term Cardiovascular Risks |
|---|---|---|
| Chemotherapy (e.g., anthracyclines) | Myocardial injury, arrhythmias, decreased ejection fraction | Cardiomyopathy, increased risk of heart failure, hypertension |
| Hormonal Therapy (e.g., aromatase inhibitors) | Changes in lipid profiles, potential blood pressure fluctuations | Increased risk of atherosclerosis, cardiovascular events (e.g., heart attack) |
| Radiation Therapy | Transient cardiac changes, radiation-induced pericarditis | Cardiovascular complications, potentially leading to heart failure or other structural damage |
| Surgery (e.g., mastectomy) | Blood loss, transient stress on the heart | Potential for long-term cardiac complications depending on the extent of the surgery |
Factors Influencing Risk of Heart Disease
Navigating breast cancer treatments can be daunting, especially when considering potential cardiovascular risks. Understanding the factors that influence these risks is crucial for proactive management and informed decision-making. This section dives into the interplay between patient characteristics and the impact of treatment on heart health.The risk of developing heart problems after breast cancer treatment is not uniform. Various factors, including age, pre-existing conditions, and family history, significantly modify an individual’s susceptibility.
Recognizing these influences is paramount for tailoring treatment strategies and preventive measures.
Age and Cardiovascular Risk
Age plays a critical role in cardiovascular risk assessment. Younger patients undergoing treatment may face different cardiovascular challenges compared to older patients. Younger individuals often have a longer life expectancy, making the potential for long-term cardiovascular complications from treatment more significant. Conversely, older patients may already have pre-existing heart conditions that could be exacerbated by treatment. Individualized risk assessment is essential to account for the unique impact of age on treatment-related cardiovascular risks.
Pre-existing Heart Conditions and Risk Modification
Pre-existing cardiovascular conditions, such as high blood pressure, high cholesterol, or prior heart attacks, significantly increase the risk of treatment-induced heart complications. Individuals with these conditions may require closer monitoring and potentially adjusted treatment protocols to mitigate cardiovascular risks. For instance, a patient with a history of hypertension may need stricter blood pressure control during and after treatment.
Family History and Genetic Predisposition
Family history of heart disease is a powerful indicator of an individual’s risk profile. Genetic predispositions to cardiovascular conditions can influence the body’s response to treatment and increase the likelihood of developing treatment-related heart problems. Understanding family history is essential for identifying individuals at higher risk and implementing preventive strategies. For example, a patient with a strong family history of coronary artery disease may require more rigorous cardiovascular monitoring and lifestyle modifications.
Individual Patient Characteristics and Treatment Response
Individual patient characteristics, including body mass index (BMI), overall health status, and lifestyle choices, can significantly influence the body’s response to treatment and the potential for cardiovascular risks. For instance, patients with higher BMIs may experience a more pronounced impact on their lipid profiles during certain treatments. This underscores the importance of personalized medicine approaches that consider individual patient variability.
Importance of Baseline Cardiovascular Assessments
Thorough baseline cardiovascular assessments before initiating breast cancer treatment are crucial for identifying pre-existing conditions and risk factors. These assessments include evaluations of blood pressure, cholesterol levels, and other relevant markers. This baseline data provides a crucial benchmark for monitoring changes during and after treatment, allowing for early detection and intervention of any developing cardiovascular issues. Regular follow-up assessments throughout treatment are equally important for ongoing risk management.
Risk Factor Categorization
| Risk Factor | Impact on Cardiovascular Risk |
|---|---|
| Age (younger) | Increased risk of long-term complications |
| Age (older) | Potential exacerbation of pre-existing conditions |
| Pre-existing heart conditions | Increased susceptibility to treatment-related complications |
| Family history of heart disease | Elevated risk profile, necessitating heightened monitoring |
| High BMI | Potentially more pronounced impact on lipid profiles |
| Unhealthy lifestyle (e.g., poor diet, lack of exercise) | Increased overall cardiovascular risk |
Mitigation Strategies and Prevention
Protecting your heart health during and after breast cancer treatment is crucial. Many treatments, while vital for fighting the disease, can increase the risk of cardiovascular complications. Proactive strategies can significantly reduce these risks, empowering you to navigate treatment with confidence and maintain a healthy heart.
Lifestyle Modifications for Cardiovascular Health
Adopting a heart-healthy lifestyle is paramount. A balanced diet, regular exercise, and stress management techniques can dramatically improve your overall health and reduce the risk of heart disease. These lifestyle modifications are not just beneficial during treatment; they’re essential for long-term cardiovascular health.
- Balanced Diet: A diet rich in fruits, vegetables, whole grains, and lean protein is fundamental. Limiting saturated and trans fats, cholesterol, and excessive sodium is also important. Examples include incorporating foods like salmon (rich in omega-3 fatty acids), berries (antioxidants), and quinoa (fiber). A registered dietitian can provide personalized dietary recommendations based on individual needs and treatment plans.
- Regular Exercise: Consistent physical activity is key to maintaining a healthy weight, improving cardiovascular function, and reducing stress. Consult with your doctor to determine appropriate exercise routines. Examples include brisk walking, swimming, cycling, or yoga. Start slowly and gradually increase intensity as tolerated. Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week.
Breast cancer treatments, while saving lives, can sometimes increase the risk of heart disease later on. A healthy diet plays a crucial role in mitigating these risks. One way to keep your heart healthy is by incorporating low-cholesterol egg preparation methods into your meals. Check out this article on low cholesterol egg preparation for some delicious and heart-friendly recipes.
These recipes can help manage cholesterol levels, a factor often overlooked in the broader picture of breast cancer treatment side effects and long-term health.
- Stress Management: Chronic stress can negatively impact cardiovascular health. Incorporating stress-reducing techniques like meditation, deep breathing exercises, or mindfulness can be highly beneficial. Examples include practicing yoga, spending time in nature, or listening to calming music. Seeking support from a therapist or counselor can also be helpful.
Preventative Measures During and After Treatment
Early detection and management of cardiovascular risks are crucial. Regular check-ups with your doctor are essential to monitor blood pressure, cholesterol levels, and other cardiovascular risk factors. Discussing any concerns or symptoms with your healthcare team is important.
- Regular Check-ups: Schedule regular check-ups with your oncologist and cardiologist to monitor your cardiovascular health throughout and after treatment. This includes blood pressure, cholesterol, and blood sugar checks. Discuss any symptoms you experience.
- Medication Management: Work closely with your healthcare team to manage any medications prescribed for breast cancer treatment and any related cardiovascular issues. Understand the potential side effects of each medication. Don’t hesitate to ask questions about any concerns.
- Communicating Concerns: Openly communicate any concerns or symptoms related to cardiovascular health with your healthcare providers. This includes any unusual fatigue, chest pain, shortness of breath, or swelling. Don’t hesitate to ask questions and seek clarification on any information.
Recommendations for Patients Undergoing Breast Cancer Treatment
This list provides practical advice for patients undergoing breast cancer treatment to reduce cardiovascular risks.
- Prioritize a heart-healthy diet and exercise routine. This includes eating a balanced diet and engaging in regular physical activity.
- Attend regular check-ups with your cardiologist and oncologist to monitor your cardiovascular health. Regular monitoring is essential to identify potential issues early.
- Communicate openly with your healthcare team about any concerns or symptoms. Don’t hesitate to ask questions and seek clarification.
- Seek support from family, friends, or support groups. Community support can provide emotional and practical assistance.
Lifestyle Changes and Preventative Measures
The following table Artikels lifestyle changes and preventative measures to help mitigate potential cardiovascular risks.
| Lifestyle Change | Description |
|---|---|
| Balanced Diet | Focus on fruits, vegetables, whole grains, and lean protein. Limit saturated and trans fats, cholesterol, and excessive sodium. |
| Regular Exercise | Engage in moderate-intensity or vigorous-intensity aerobic activity at least 150 minutes per week. |
| Stress Management | Incorporate stress-reducing techniques like meditation, deep breathing, or mindfulness. |
| Regular Check-ups | Schedule regular check-ups with your oncologist and cardiologist to monitor cardiovascular health. |
| Medication Management | Work closely with your healthcare team to manage any medications and understand potential side effects. |
| Open Communication | Communicate any concerns or symptoms related to cardiovascular health with your healthcare providers. |
Research and Ongoing Studies
Unraveling the complex relationship between breast cancer treatments and cardiovascular health requires ongoing research. Scientists are actively investigating the mechanisms behind potential risks, trying to understand the long-term effects of different treatment approaches, and identifying strategies to mitigate these risks. This ongoing research is crucial for tailoring treatments and improving patient outcomes.Researchers are delving deeper into the potential long-term effects of different treatments on the cardiovascular system.
This includes understanding how specific chemotherapeutic agents, radiation therapies, and hormonal therapies may impact the heart and blood vessels. The goal is to predict which patients might be at higher risk and develop personalized strategies for preventing or managing cardiovascular complications.
Ongoing Research Approaches
Various research methodologies are employed to explore the link between breast cancer treatments and cardiovascular health. Epidemiological studies track the incidence of cardiovascular events in large cohorts of breast cancer survivors, analyzing factors such as treatment type, duration, and patient characteristics. Mechanistic studies investigate the biological pathways involved in the observed effects, examining how treatments influence the heart and blood vessels at a cellular and molecular level.
Clinical trials are also underway to evaluate the efficacy and safety of interventions aimed at reducing cardiovascular risk in breast cancer survivors.
Understanding Mechanisms and Potential Long-Term Effects
Current research suggests that certain breast cancer treatments, particularly chemotherapy and radiation therapy, may increase oxidative stress and inflammation in the body, potentially leading to endothelial dysfunction and atherosclerosis. Hormonal therapies, while effective in managing breast cancer, might also influence lipid profiles and increase the risk of cardiovascular disease. The cumulative effect of these factors over time could lead to a higher incidence of heart disease in breast cancer survivors.
Longitudinal studies are crucial for observing these effects over extended periods.
Challenges in Studying the Complex Relationship
Several challenges hinder a complete understanding of the intricate link between breast cancer treatments and heart disease. It’s difficult to isolate the specific effects of individual treatments from other factors, such as pre-existing cardiovascular conditions, lifestyle choices, and age. Furthermore, the long latency period between treatment and the onset of cardiovascular complications can make it challenging to establish clear causal relationships.
The diverse range of treatments and patient characteristics also contributes to the complexity of the research. Identifying specific biomarkers or risk factors that accurately predict cardiovascular risk in breast cancer survivors is another significant challenge.
Summary of Major Findings from Research Studies
Studies have demonstrated a correlation between certain breast cancer treatments and an increased risk of cardiovascular events, including heart attacks and strokes. For instance, studies have shown a potential link between anthracycline-based chemotherapy and an increased risk of cardiomyopathy. Moreover, radiation therapy targeting the chest area has been associated with a higher risk of coronary artery disease. However, it’s important to note that the risk varies greatly depending on individual factors, treatment intensity, and patient characteristics.
Further research is needed to quantify these risks more precisely and identify high-risk subgroups.
Patient Education and Support
Navigating breast cancer treatment can be overwhelming, and understanding the potential cardiovascular risks associated with these therapies is crucial for informed decision-making. Empowering patients with knowledge and providing robust support systems are vital components of holistic care. This section delves into the importance of patient education and effective communication strategies, highlighting resources and support networks available to patients.Effective patient education about cardiovascular risks is paramount to ensuring proactive management of potential complications.
It’s not just about listing risks; it’s about providing context, empowering patients to ask questions, and fostering a partnership in their care.
Importance of Patient Education
Thorough education equips patients with the knowledge necessary to make informed choices about their treatment and lifestyle. This knowledge empowers them to advocate for their health, actively participate in decisions, and take proactive steps to mitigate risks. Understanding the potential for cardiovascular issues associated with treatment helps patients make choices aligned with their individual needs and preferences. By fostering a collaborative approach, patients are better prepared to navigate treatment and long-term health management.
Strategies for Effective Communication
Open and honest communication between healthcare providers and patients is essential. This involves clear explanations of potential risks, tailored to each patient’s comprehension level. Using visual aids, providing written materials, and offering multiple avenues for questions and concerns are crucial strategies. Active listening, empathy, and addressing patient anxieties are critical aspects of effective communication. Encouraging patients to ask questions, fostering a safe environment for discussing concerns, and ensuring that patients understand the risks in relation to their personal circumstances are all part of the communication process.
Resources and Support Systems for Patients
A robust network of resources can provide invaluable support for patients facing these challenges. These resources can offer information, emotional support, and practical guidance.
- Cancer Support Groups: These groups provide a safe space for sharing experiences, offering emotional support, and connecting with others facing similar challenges. They can offer peer-to-peer encouragement and validation.
- Cardiovascular Specialists: Consulting with specialists can provide personalized assessments of cardiovascular health and tailored recommendations for managing potential risks.
- Registered Dietitians: Dietitians can offer guidance on heart-healthy diets and nutritional strategies to support cardiovascular health throughout treatment and beyond.
- Physical Therapists: Exercise programs tailored to patients’ needs can help maintain or improve cardiovascular fitness while managing potential side effects of treatment.
- Mental Health Professionals: Addressing emotional and psychological well-being is critical, as anxiety and stress can impact both physical and mental health. Mental health professionals can offer support and strategies for coping with the emotional challenges of cancer and its treatment.
Fostering Open Communication
Open communication between patients and healthcare providers is crucial. Patients should feel comfortable asking questions, voicing concerns, and actively participating in their care. Healthcare providers should actively listen to patients, provide clear and concise information, and ensure patients understand the risks and benefits of different treatment options.
| Resource Type | Description | Example |
|---|---|---|
| Cancer Support Groups | Peer-to-peer support and emotional encouragement. | Local cancer support groups, online forums. |
| Cardiovascular Specialists | Personalized assessments and recommendations for cardiovascular health. | Cardiologists, cardio-oncologists. |
| Registered Dietitians | Guidance on heart-healthy diets and nutritional strategies. | Registered dietitians specializing in oncology or cardiac care. |
| Physical Therapists | Tailored exercise programs for maintaining/improving cardiovascular fitness. | Physical therapists with experience in oncology rehabilitation. |
| Mental Health Professionals | Support for emotional and psychological well-being. | Psychologists, psychiatrists, social workers. |
Illustrative Case Studies

Navigating the complex interplay between breast cancer treatments and cardiovascular health requires understanding real-world examples. Case studies provide valuable insights into how individual experiences manifest and highlight the importance of personalized approaches to treatment and risk mitigation. These narratives offer a tangible connection to the potential consequences and the proactive strategies that can be employed.This section presents illustrative cases, demonstrating both the challenges and opportunities in managing cardiovascular risks associated with breast cancer treatments.
The experiences underscore the critical need for proactive monitoring, individualized treatment plans, and ongoing research to refine preventative measures.
Patient Experiencing Cardiovascular Complications
A 50-year-old patient, diagnosed with estrogen receptor-positive breast cancer, underwent a combination of chemotherapy and hormonal therapy. During the treatment, she experienced increasing fatigue, shortness of breath, and swelling in her ankles. Further evaluation revealed elevated blood pressure and cholesterol levels, indicative of developing cardiovascular disease. This case highlights the importance of regular cardiovascular assessments during and after breast cancer treatment, particularly for patients on therapies known to increase cardiovascular risk.
Patient Successfully Mitigating Risks
A 45-year-old patient, diagnosed with HER2-positive breast cancer, underwent targeted therapy. Recognizing the potential for cardiovascular complications, she actively engaged in lifestyle modifications, including a heart-healthy diet, regular exercise, and stress management techniques. She also meticulously followed her oncologist’s recommendations for blood pressure and cholesterol monitoring. This proactive approach significantly reduced her risk of developing cardiovascular issues.
This case illustrates the power of patient advocacy and proactive lifestyle choices in mitigating treatment-related risks.
Importance of Personalized Treatment Plans
Breast cancer treatment and its impact on cardiovascular health are highly personalized. Individual risk factors, such as family history, pre-existing conditions, and treatment regimens, must be considered when developing a comprehensive care plan. For example, a patient with a family history of heart disease might require more intensive cardiovascular monitoring and lifestyle recommendations compared to a patient without such a history.
This emphasizes the critical role of shared decision-making between the patient, oncologist, and cardiologist.
Importance of Early Intervention and Management
Early detection and intervention are crucial in managing cardiovascular complications arising from breast cancer treatment. A 62-year-old patient, diagnosed with triple-negative breast cancer, experienced symptoms of peripheral artery disease (PAD) during her treatment. Prompt diagnosis and intervention, including medication and lifestyle modifications, helped stabilize her condition and prevent further progression. This case underscores the significance of regular check-ups and prompt reporting of any unusual symptoms.
Summary Table of Case Studies
| Case Study | Patient Profile | Treatment | Cardiovascular Complications | Mitigation Strategies | Outcome |
|---|---|---|---|---|---|
| Patient 1 | 50-year-old, ER+ breast cancer | Chemotherapy & Hormonal Therapy | Elevated blood pressure, cholesterol | Not explicitly mentioned | Developed cardiovascular issues |
| Patient 2 | 45-year-old, HER2+ breast cancer | Targeted Therapy | None reported | Healthy diet, exercise, stress management, monitoring | Successfully mitigated risks |
| Patient 3 | General | Various | Not explicitly mentioned | Personalized treatment plans considering risk factors | Improved outcomes |
| Patient 4 | 62-year-old, TNBC | Chemotherapy | Peripheral artery disease | Medication, lifestyle modifications | Condition stabilized |
Last Recap
In conclusion, the connection between breast cancer treatments and heart disease is a critical area of concern. Understanding the specific risks associated with different treatment modalities, considering individual patient factors, and implementing mitigation strategies are essential for optimizing patient outcomes. Ongoing research and open communication between patients and healthcare professionals are paramount in navigating this complex challenge. Ultimately, the goal is to provide comprehensive care that addresses both cancer and heart health.