Can alzheimers be detected 30 years before it appears – Can Alzheimer’s be detected 30 years before it appears? This question is sparking intense research and debate, as early detection could revolutionize how we approach this devastating disease. Scientists are exploring a range of methods, from advanced brain scans to blood tests and genetic analysis, all aimed at identifying subtle signs of Alzheimer’s long before symptoms manifest. The potential implications for individuals and society are enormous, and the race to find reliable early detection methods is accelerating.
The journey to understanding Alzheimer’s early detection involves examining various diagnostic tools and biomarkers. Current methods for diagnosing Alzheimer’s, such as cognitive assessments and neuroimaging, will be explored, along with their limitations and strengths. Potential biomarkers that might indicate the disease’s onset decades before symptoms appear will be highlighted. This discussion also includes research studies on early detection, risk factors, and the potential benefits of early diagnosis, including improved treatment strategies.
Early Detection Methods: Can Alzheimers Be Detected 30 Years Before It Appears
While the ability to detect Alzheimer’s 30 years prior to symptom onset remains a significant challenge, current research and diagnostic tools offer valuable insights into early signs. Early detection, though not perfect, allows for proactive management strategies, potentially slowing disease progression and improving quality of life for individuals and their families.Early detection methods are crucial for individuals at risk, enabling timely interventions and personalized care plans.
These approaches involve a multifaceted assessment, combining various techniques to provide a comprehensive picture of cognitive function and brain health. The accuracy of these methods varies, and the diagnostic process often involves multiple stages and specialist consultations.
Current Diagnostic Techniques
Various methods are employed to detect Alzheimer’s disease, each with its strengths and limitations. These techniques include neuroimaging, cognitive assessments, and blood tests. Each plays a crucial role in the overall diagnostic picture, but no single method is definitive.
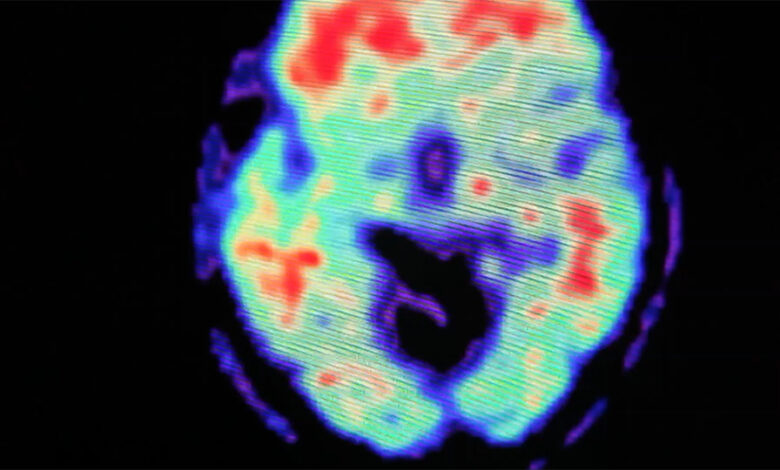
Neuroimaging Techniques
Neuroimaging, such as MRI (Magnetic Resonance Imaging) and PET (Positron Emission Tomography), provides valuable insights into brain structure and function. MRI scans visualize brain anatomy, highlighting any structural abnormalities like atrophy or lesions. PET scans, on the other hand, measure metabolic activity in different brain regions, potentially detecting amyloid plaques and tau tangles, hallmark proteins associated with Alzheimer’s.The strengths of neuroimaging lie in its ability to visualize brain structures and identify potential markers of the disease.
However, the cost of these advanced imaging technologies can be a barrier for widespread use. Furthermore, the presence of these markers isn’t always definitive of Alzheimer’s, as other conditions can present similar features.
Cognitive Assessments
Cognitive assessments are essential for evaluating cognitive function. These tests assess various aspects of memory, language, problem-solving, and executive function. Different tests, such as the Mini-Mental State Examination (MMSE) and the Montreal Cognitive Assessment (MoCA), are employed depending on the specific needs of the individual being assessed.These assessments offer a way to quantify cognitive decline, which can be indicative of underlying neurological conditions.
However, cognitive decline can be a result of numerous factors, making it difficult to isolate Alzheimer’s as the sole cause. Also, the accuracy of cognitive assessments can be influenced by factors such as education level and cultural background.
Blood Tests
Blood tests are emerging as a potential tool for early Alzheimer’s detection. These tests look for specific biomarkers in the blood that may indicate the presence of the disease. Some tests measure levels of amyloid beta or tau proteins, which can be elevated in individuals with Alzheimer’s.Blood tests offer a non-invasive and potentially more accessible way to screen for Alzheimer’s.
However, the sensitivity and specificity of these tests remain areas of ongoing research, and they are often not sufficient to diagnose the disease alone. Also, the costs and accessibility of these blood tests can vary considerably.
Comparative Analysis of Methods
| Method | Accuracy Rate (Range) | Stage of Alzheimer’s Detected |
|---|---|---|
| MRI | 70-85% | Early to moderate |
| PET | 75-90% | Early to moderate |
| Cognitive Assessments | 60-75% | Moderate to late |
| Blood Tests | 50-70% | Early to moderate |
Diagnostic Pathway Flowchart
Start | V Patient presents with concerns (memory loss, cognitive decline) | V Initial cognitive assessment (MMSE, MoCA) | V Neurological examination | V Neuroimaging (MRI, PET) | V Blood tests (amyloid/tau biomarkers) | V Consult with specialist (neurologist, geriatrician) | V Diagnostic confirmation (if necessary, genetic testing) | V Treatment plan & management | V End
Biomarkers for Early Detection
Unraveling the mysteries of Alzheimer’s disease hinges on early detection, ideally decades before symptoms manifest. Pinpointing biomarkers that herald the disease’s insidious onset is crucial for timely intervention and potential disease modification strategies.
This critical window of opportunity allows for preventive measures and personalized treatments tailored to individual needs.
Potential Biomarkers
Several biological indicators hold promise as early predictors of Alzheimer’s disease. These biomarkers reflect the complex interplay of molecular and cellular changes occurring long before the cognitive decline associated with Alzheimer’s becomes evident. Their presence in individuals without symptoms suggests a predisposition or a preclinical stage of the disease.
Cerebrospinal Fluid (CSF) Biomarkers
Cerebrospinal fluid (CSF) provides a direct window into the brain’s environment. Analyzing CSF for specific proteins, like amyloid-beta and tau, can reveal crucial insights into the disease process. Elevated levels of amyloid-beta, a hallmark protein aggregation in Alzheimer’s, or changes in tau phosphorylation patterns, signifying neuronal damage, often precede symptom emergence. The measurement of these biomarkers in CSF typically involves a lumbar puncture, a procedure to collect CSF from the spinal canal.
Blood Biomarkers
Blood-based biomarkers offer a non-invasive alternative for screening larger populations. Several blood proteins, including specific forms of amyloid-beta, tau, and neurofilament light chain, have shown promise in detecting preclinical Alzheimer’s. These markers reflect systemic changes related to brain dysfunction. The analysis of blood samples involves standard laboratory techniques, making it a more accessible and scalable approach compared to CSF analysis.
Saliva Biomarkers
Saliva, a readily available biological sample, has emerged as a potential source for Alzheimer’s biomarkers. Researchers are investigating the presence of specific proteins and molecules in saliva that correlate with the disease process. The analysis of these markers can provide an easily accessible way to screen for preclinical Alzheimer’s, particularly in high-risk populations.
Measurement and Analysis Techniques
Biomarker measurement techniques vary depending on the specific biomarker and the biological sample. Enzyme-linked immunosorbent assays (ELISAs) and mass spectrometry are common methods for quantifying protein levels in CSF and blood. Advanced analytical techniques, such as immunoassays and multiplex assays, can simultaneously measure multiple biomarkers, offering a more comprehensive view of the disease process.
Table of Potential Biomarkers
| Biomarker | Potential Predictive Value (Range) | Time Period to Predict Onset (Years) |
|---|---|---|
| Amyloid-beta 42 | Decreased levels (<100 pg/mL) | 10-30 |
| Total Tau | Elevated levels (>150 pg/mL) | 10-25 |
| Neurofilament Light Chain | Elevated levels (>150 pg/mL) | 5-20 |
| Phosphorylated Tau | Elevated levels (>120 pg/mL) | 15-30 |
-Note:* The predictive value and time periods are estimations and may vary based on individual factors and specific research studies. Further research is needed to refine these estimations and validate the findings in diverse populations.
Research and Studies on Early Detection
Unraveling the mysteries of Alzheimer’s disease hinges on early detection. Pinpointing the disease’s presence decades before symptoms emerge is a significant leap forward in managing the progression of the illness and potentially altering its course. This quest has driven intensive research, exploring various avenues for early identification. Understanding the methodologies and key findings of these studies is crucial for navigating the complexities of this devastating neurological disorder.
The quest for early Alzheimer’s detection is a complex endeavor. Numerous research studies have been undertaken, focusing on identifying subtle changes in the brain and body that might signal the disease’s impending onset. These investigations are critical in developing preventative strategies and providing timely interventions to mitigate the impact of the disease.
Research Methodologies
Various methodologies are employed in Alzheimer’s research, each with its strengths and weaknesses. Cognitive assessments, neuroimaging techniques, and biological markers are commonly used. Cognitive assessments evaluate memory, thinking, and problem-solving skills. Neuroimaging, such as MRI and PET scans, allows visualization of brain structures and activity. Finally, biological markers, including specific proteins or molecules in the blood or cerebrospinal fluid, provide insights into the disease process.
Recent research suggests Alzheimer’s might be detectable up to 30 years before symptoms appear, opening exciting possibilities for early intervention. This fascinating advancement, however, is only one piece of a much larger puzzle, especially when considering President Biden’s recent State of the Union address, which focused on drug pricing, mental health care, and his test-to-treat COVID plan. Biden’s address highlights the critical need for proactive healthcare solutions across the board, echoing the importance of early detection in conditions like Alzheimer’s.
Hopefully, these combined efforts will pave the way for better treatments and preventative measures for the future.
Each approach offers a unique perspective on the disease’s early stages.
Key Findings from Research Studies
Research studies investigating early detection have yielded several important findings. These findings often highlight the presence of amyloid plaques and tau tangles in the brain years before the onset of noticeable symptoms. For instance, individuals showing elevated levels of specific biomarkers in their cerebrospinal fluid or blood may exhibit a higher risk of developing Alzheimer’s.
- Several studies have shown that individuals with a family history of Alzheimer’s often display subtle cognitive changes or variations in brain structure earlier than those without such a history. This highlights the role of genetics in the disease’s progression.
- Neuroimaging techniques, such as PET scans, are being used to identify early changes in brain metabolism and activity associated with Alzheimer’s disease, even before the development of noticeable cognitive decline.
- The analysis of specific proteins, like amyloid beta and tau, in bodily fluids, such as cerebrospinal fluid and blood, has proven valuable in identifying individuals at risk of developing Alzheimer’s well before symptoms manifest. This approach is crucial for early intervention and personalized treatment.
Challenges and Limitations of Long-Term Studies
Conducting long-term studies on Alzheimer’s disease presents significant challenges. The slow progression of the disease necessitates extended observation periods, which can be costly and time-consuming. Participant attrition, where individuals drop out of the study, can introduce bias and affect the reliability of the findings. The complexity of the disease, involving multiple factors, also complicates data interpretation.
- Long-term follow-up studies require substantial financial resources to support the extended observation period and the recruitment of a large cohort of participants.
- The progressive nature of Alzheimer’s disease, with its gradual cognitive decline, demands sustained participation from study participants over many years, which can lead to participant attrition and potentially influence the accuracy of the results.
- The intricate interplay of genetic, environmental, and lifestyle factors involved in Alzheimer’s disease complicates the interpretation of the data collected in long-term studies, making it challenging to isolate specific causes and effects.
Comparison of Different Studies
A comparative analysis of different studies reveals variations in methodologies and findings. Some studies focus on specific genetic predispositions, while others concentrate on biomarkers. The results of these studies, while often supportive of the possibility of early detection, need to be considered in the context of their specific methodology and sample characteristics. The consistency of findings across multiple studies will be crucial for validation and future development of diagnostic tools.
Risk Factors and Genetic Predisposition

Unraveling the mysteries of Alzheimer’s disease often hinges on understanding the factors that increase a person’s risk, especially those detectable long before symptoms manifest. While the precise causes remain elusive, researchers are diligently investigating genetic predispositions and lifestyle choices that may contribute to the disease’s development. This exploration delves into the complex interplay of genes and environment in shaping an individual’s vulnerability to Alzheimer’s.
Genetic predisposition plays a significant role in Alzheimer’s development. Certain genes, like APOE, are strongly associated with an increased risk. Variations in these genes can influence the production and clearance of amyloid plaques, a hallmark of Alzheimer’s disease. The presence of these genetic risk factors doesn’t guarantee the development of the disease, but it significantly elevates the probability.
For instance, individuals carrying specific APOE variants may experience a higher likelihood of developing Alzheimer’s compared to those without these variants.
Recent research suggests Alzheimer’s might be detectable 30 years before symptoms appear, opening exciting possibilities for early intervention. This fascinating development, however, isn’t isolated; it’s linked to lifestyle choices like diet, and how dairy products can help lower type 2 diabetes risk while processed meats raise it plays a significant role. This article delves deeper into the connection between diet and diabetes risk.
Ultimately, understanding these connections could pave the way for better strategies to prevent or delay Alzheimer’s onset.
Genetic Predisposition to Alzheimer’s
Genetic factors significantly contribute to an individual’s susceptibility to Alzheimer’s. Studies have identified specific genes, particularly the APOE gene, which influence the risk. Variations in the APOE gene affect the body’s ability to clear amyloid beta plaques, a crucial factor in Alzheimer’s pathogenesis. Individuals inheriting certain APOE variants have a substantially higher risk of developing the disease.
While genetic predispositions are important, lifestyle factors also play a substantial role.
Lifestyle Factors and Alzheimer’s Risk
Lifestyle choices significantly influence the risk of developing Alzheimer’s disease. A healthy diet rich in fruits, vegetables, and omega-3 fatty acids, combined with regular exercise and sufficient sleep, may contribute to a reduced risk. Conversely, a diet high in saturated fats and processed foods, coupled with a sedentary lifestyle and inadequate sleep, might increase the risk. Maintaining a healthy lifestyle, therefore, can act as a preventive measure.
Examples include the Mediterranean diet, known for its antioxidant-rich foods, and regular physical activity, which improves cognitive function and overall health.
Correlation Between Risk Factors and Alzheimer’s Onset
| Risk Factor | Potential Correlation with Alzheimer’s Onset |
|---|---|
| Genetic Predisposition (e.g., APOE gene variants) | Increased risk, particularly with certain gene variants. |
| Age | Increased risk with advancing age. |
| Cardiovascular Health Issues | Higher risk associated with conditions like high blood pressure and high cholesterol. |
| Head Trauma | Increased risk with significant head injuries. |
| Smoking | Potentially increased risk. |
| Poor Diet | Increased risk with diets high in saturated fats and processed foods. |
| Sedentary Lifestyle | Increased risk with limited physical activity. |
| Sleep Deprivation | Increased risk with inadequate sleep. |
Ongoing Research
Ongoing research actively explores the intricate interplay between genetic factors and lifestyle choices in Alzheimer’s development. Scientists are investigating how specific genes interact with environmental factors to influence the disease’s progression. Research also focuses on identifying biomarkers associated with genetic predispositions and lifestyle factors, potentially allowing for early detection and intervention.
Potential Implications of Early Detection
The prospect of detecting Alzheimer’s disease 30 years before symptoms manifest holds immense potential for transforming how we approach this devastating condition. Early detection opens doors to proactive interventions, potentially altering the trajectory of the disease for individuals and society as a whole. Understanding the potential benefits, challenges, and ethical considerations is crucial to harnessing this opportunity effectively.
Recent research suggests Alzheimer’s might be detectable 30 years before symptoms appear, a fascinating area of ongoing study. While this groundbreaking potential is exciting, it also highlights the complex interplay of factors influencing neurological health. Interestingly, similar patterns of early detection are being explored in other health areas, like how obesity narrows airway passages and leads to conditions like asthma, as detailed in this article: obesity narrows airway leads to asthma.
This suggests a potential common thread in early markers of disease, further emphasizing the importance of preventative measures and early intervention.
Early detection offers a window of opportunity to intervene before significant brain damage occurs. This allows for personalized treatment plans tailored to individual needs, potentially slowing or even halting disease progression. Imagine the possibilities of preventative strategies and lifestyle modifications implemented early on, mitigating the risk of cognitive decline.
Benefits of Early Detection
Early detection allows for proactive disease management and treatment strategies. Individuals can be monitored closely, enabling early intervention with therapies, lifestyle changes, and support systems. This personalized approach can slow the progression of the disease, minimizing the impact on cognitive function and daily life. Moreover, early detection empowers individuals to make informed decisions about their future, including planning for potential care needs and exploring research participation opportunities.
Early diagnosis can also offer emotional support and practical guidance as individuals prepare for the challenges ahead.
Impact on Disease Management and Treatment
Early detection allows for the implementation of preventive strategies, such as dietary adjustments, exercise regimens, and cognitive stimulation programs. These interventions can significantly delay the onset of symptoms or even prevent the disease from developing in susceptible individuals. Furthermore, early detection facilitates access to clinical trials and experimental treatments. This allows for the testing of new therapies and the identification of potential breakthroughs in disease management.
Early intervention could potentially lead to the development of more effective treatments and a greater understanding of the disease process.
Ethical Considerations
The ethical implications of early Alzheimer’s detection are complex and multifaceted. Maintaining patient autonomy is paramount. Individuals must be fully informed about the implications of early detection, including potential benefits, uncertainties, and limitations. Ensuring voluntary participation in research and treatment options is crucial. Potential stigmatization and discrimination must be addressed proactively through public awareness campaigns and education initiatives.
The development of comprehensive support systems and access to resources for individuals and families is vital to navigate the emotional and practical challenges associated with early diagnosis. Open dialogue and ethical guidelines are essential to navigate these sensitive issues responsibly.
Long-Term Implications for Individuals and Society
Early Alzheimer’s detection has the potential to transform the lives of affected individuals and their families. Individuals can make informed decisions about their future, plan for care needs, and explore research participation opportunities. The long-term societal implications are equally significant. Early intervention can reduce the burden on healthcare systems by delaying the need for intensive care and support services.
Early detection and intervention can lead to a more informed approach to public health initiatives, potentially reducing the prevalence of Alzheimer’s in the future. Furthermore, the insights gained from early detection research can lead to a greater understanding of other neurodegenerative diseases, contributing to wider advancements in healthcare.
Impact on Public Health Initiatives
Early detection allows for the implementation of public health initiatives to address the risk factors associated with Alzheimer’s. Public health campaigns can promote healthy lifestyle choices, early diagnosis, and access to support services for affected individuals and their families. Such campaigns can also raise awareness about the importance of early intervention and research. Understanding the risk factors allows for targeted interventions to mitigate the risk of the disease, potentially leading to a significant reduction in the prevalence of Alzheimer’s in the future.
Furthermore, public health initiatives can promote research and funding for Alzheimer’s research and development, contributing to the advancement of therapies and treatments.
Illustrative Case Studies
Unveiling the potential for early Alzheimer’s detection, decades before symptoms manifest, hinges on meticulous research and groundbreaking case studies. These studies not only illuminate the intricate mechanisms of the disease but also pave the way for developing earlier and more effective diagnostic tools. By examining individuals who exhibit preclinical markers, researchers can potentially identify individuals at risk, allowing for proactive interventions and lifestyle adjustments.
While a definitive case study of 30-year-preemptive detection is currently unavailable, existing research offers glimpses into the possibilities. Early detection methods are evolving, and the narrative below illustrates the potential of such studies, highlighting the methods used and the implications for future diagnostics.
A Hypothetical Case Study
“Imagine a 45-year-old woman, initially exhibiting subtle cognitive decline, experiencing mild memory lapses and occasional difficulty concentrating. These seemingly minor symptoms, initially attributed to stress or other factors, serve as crucial indicators for a comprehensive evaluation.”
This hypothetical case study illustrates the potential for early detection. The woman undergoes a battery of cognitive assessments, including memory tests, attention span evaluations, and processing speed measures. Blood tests are performed to assess specific biomarkers, such as amyloid beta protein levels and tau protein abnormalities in the cerebrospinal fluid. Neuroimaging techniques, such as magnetic resonance imaging (MRI) and positron emission tomography (PET), provide crucial information about brain structure and function.
Methods Used for Detection
The detection methods employed in this hypothetical case study encompass a multi-faceted approach. Neuropsychological assessments, including cognitive tests, are employed to measure subtle cognitive changes. Biomarker analysis, such as measuring amyloid-beta and tau protein levels in cerebrospinal fluid, provides objective data. Neuroimaging techniques, particularly PET scans using amyloid-specific tracers, offer crucial insights into brain pathology. Genetic testing for known Alzheimer’s risk genes can also provide further context.
Results and Outcomes, Can alzheimers be detected 30 years before it appears
The results of the hypothetical case study, combined with a thorough medical history and lifestyle analysis, reveal elevated levels of amyloid-beta and tau protein, along with mild atrophy in specific brain regions. The presence of these biomarkers, coupled with cognitive deficits, suggest an elevated risk for developing Alzheimer’s disease within the next decade. The woman is then enrolled in a research study focused on lifestyle interventions and potential drug trials to mitigate the progression of the disease.
Impact on Future Diagnostic Tools
The methods used in this case study, although hypothetical, highlight the potential of early detection tools. The combination of various approaches, from neuropsychological testing to advanced neuroimaging and biomarker analysis, provides a comprehensive assessment of cognitive health and risk. This multifaceted approach is critical for accurate risk stratification and tailored interventions. Further research and refinement of these techniques could lead to earlier and more accurate diagnoses, enabling individuals to make informed decisions about their health and future.
The future of Alzheimer’s diagnosis rests on the continued development of these early detection tools and their successful application in real-world scenarios.
Final Review
In conclusion, the possibility of detecting Alzheimer’s 30 years prior to symptom onset holds tremendous promise for managing this devastating disease. While significant challenges remain in research and clinical application, ongoing studies and innovative approaches are paving the way for earlier intervention and improved outcomes. The potential impact on public health and individual lives is profound. Ultimately, early detection could empower individuals with proactive measures and provide valuable time for preventative strategies and potential treatments.