Can dry eyes cause floaters? This exploration delves into the potential connection between dry eye syndrome and the appearance of floaters in your vision. We’ll examine the symptoms, potential mechanisms, and treatment options for both conditions, offering insights into the intricate workings of your eyes.
Dry eye syndrome, a common ailment, often manifests with symptoms like eye discomfort, redness, and blurry vision. Floaters, on the other hand, appear as dark spots or lines that drift across your field of vision. While seemingly unrelated, could there be a hidden link between these two seemingly different eye issues?
Introduction to Dry Eyes and Floaters
Dry eye syndrome, a common eye condition, affects millions worldwide. It’s characterized by a lack of sufficient tears to lubricate and protect the eyes. This can lead to discomfort, blurry vision, and even long-term complications if left untreated. Understanding the different types of dry eye and their causes is crucial for effective management. Similarly, floaters, those tiny specks or shadows that dance in your field of vision, are a frequent concern for many.
This exploration will delve into the origins and characteristics of both dry eyes and floaters, and highlight their overlapping symptoms.Dry eye syndrome is often caused by an imbalance in tear production or evaporation. Several factors contribute to this imbalance, including age-related changes, certain medical conditions, medications, environmental factors, and even lifestyle choices. The types of dry eye, and the resulting symptoms, vary.
Dry Eye Syndrome Types
Dry eye can be categorized into two primary types: aqueous-deficient dry eye and evaporative dry eye. Aqueous-deficient dry eye occurs when the eyes don’t produce enough tears, leading to a dry, irritated feeling. This is often related to aging, or medical conditions that interfere with tear production. Evaporative dry eye, conversely, arises when tears evaporate too quickly.
This is more commonly caused by factors that affect the tear film’s stability, like environmental conditions (wind, air conditioning), or certain medical conditions. Some individuals may experience a combination of both types.
Floaters: Origins and Characteristics
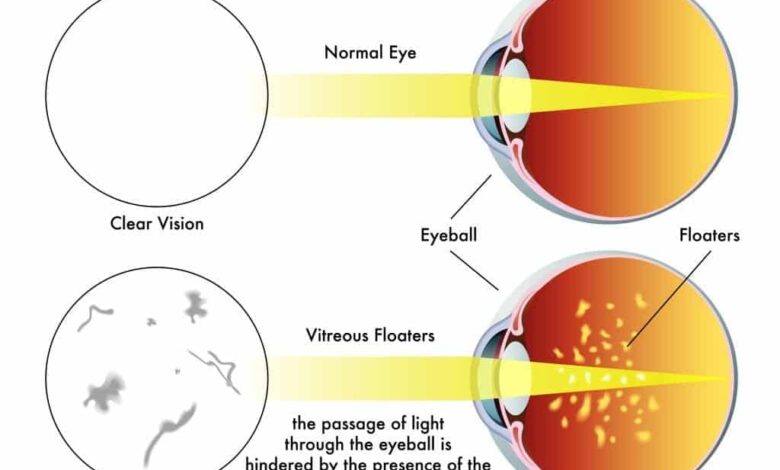
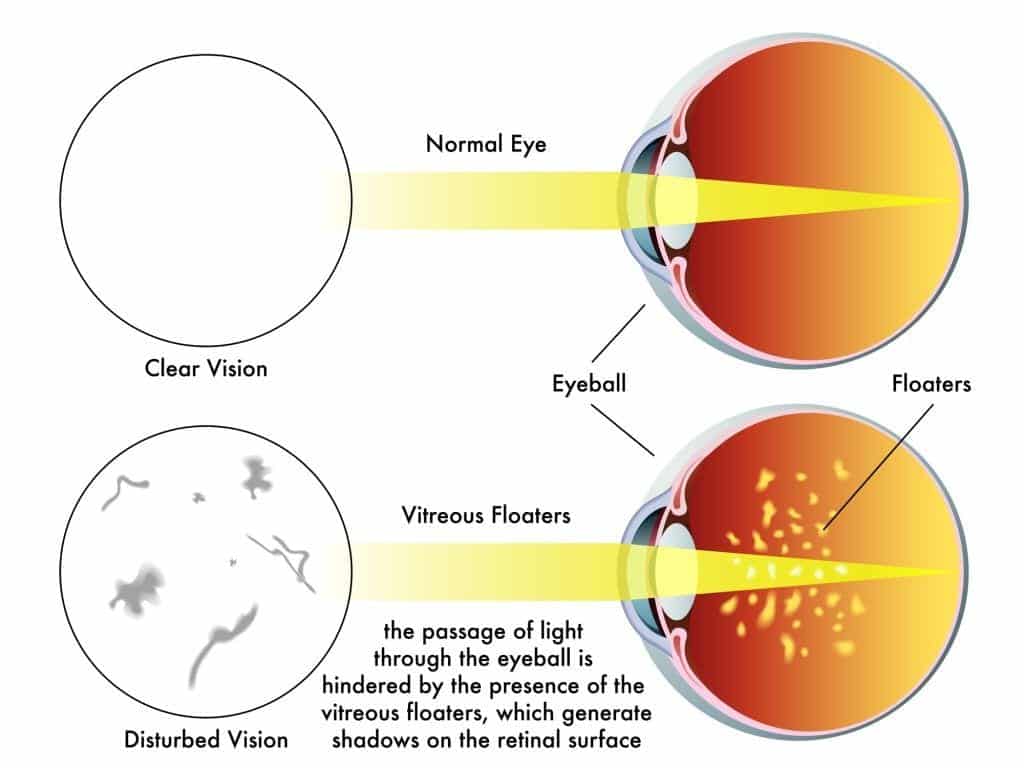
Floaters are small, dark spots or shapes that seem to drift within the field of vision. These are typically caused by debris, such as cellular material or condensation, accumulating in the vitreous humor, the gel-like substance filling the eye’s interior. As we age, the vitreous humor can become more viscous and clump, causing the floaters to become more noticeable.
The size and shape of floaters can vary significantly, and they are often described as cobwebs, spots, or strings.
Common Symptoms of Dry Eyes and Floaters
Both dry eyes and floaters can manifest with similar symptoms, leading to confusion. Common symptoms include eye irritation, discomfort, and a gritty or sandy sensation. Dry eyes can also cause blurred vision, especially in low-light conditions, and excessive tearing. Floaters, while not causing discomfort in themselves, can lead to a diminished visual experience.
Comparison of Dry Eye and Floaters Symptoms
| Feature | Dry Eyes | Floaters |
|---|---|---|
| Primary Symptom | Eye dryness, irritation, gritty sensation | Visual disturbances (spots, shapes, strings) |
| Associated Symptoms | Blurred vision, excessive tearing, sensitivity to light | No significant discomfort, but potentially reduced visual clarity |
| Cause | Tear film imbalance (insufficient production or rapid evaporation) | Vitreous humor changes (age-related or other factors) |
| Impact on Vision | Potentially blurry vision, especially in low light | Reduced visual clarity (perception of spots, shapes) |
Potential Link Between Dry Eyes and Floaters
The relationship between dry eyes and floaters, while not fully understood, is increasingly recognized by ophthalmologists. While not a direct cause-and-effect, there are potential connections between the two conditions that deserve investigation. This exploration delves into the possible mechanisms and anatomical pathways linking these eye issues.The dryness of the ocular surface, a hallmark of dry eye, can potentially impact the delicate balance within the eye’s interior, influencing the formation or aggravation of floaters.
This might occur through changes in the vitreous humor, the gel-like substance filling the eye. The vitreous humor’s composition and viscosity can be influenced by various factors, including the health of the tear film.
Potential Mechanisms Linking Dry Eyes and Floaters
Dry eye conditions, characterized by insufficient tear production or compromised tear film quality, can potentially lead to changes in the vitreous humor. The vitreous humor is a transparent gel that supports the retina and lens. Changes in its hydration or composition might promote the formation of floaters, which are small, dark spots or shapes perceived as moving within the visual field.
Anatomical Connections and Shared Physiological Pathways
The eye’s structure is intricately connected. The tear film, crucial for maintaining a healthy ocular surface, is closely related to the overall eye health. A compromised tear film can lead to inflammation and irritation of the conjunctiva, the membrane lining the inside of the eyelids and the sclera (the white part of the eye). This irritation could, in turn, trigger systemic inflammatory responses.
These responses may indirectly affect the vitreous humor, potentially contributing to the development or worsening of floaters. The delicate balance between aqueous humor (fluid in the anterior chamber) and vitreous humor (gel in the posterior chamber) is vital for maintaining intraocular pressure and the overall health of the eye. Any imbalance, even subtle ones, could have ripple effects throughout the eye’s structure, affecting both the tear film and the vitreous humor.
Environmental and Lifestyle Factors
Environmental factors and lifestyle choices can contribute to both dry eyes and floaters. Prolonged exposure to dry environments (e.g., air conditioning, desert climates) can exacerbate dry eye symptoms, which, in turn, may have an indirect impact on the vitreous humor. Similarly, a diet lacking essential nutrients vital for eye health can contribute to both conditions. For example, a deficiency in antioxidants could affect the stability of the vitreous humor, making it more prone to changes.
Also, certain medications, such as antihistamines and diuretics, can contribute to dry eyes, and indirectly affect the vitreous humor. Smoking, a significant environmental factor, can increase oxidative stress, potentially leading to both dry eyes and floaters, or other eye conditions.
Potential Contributing Factors
| Factor | Dry Eyes | Floaters |
|---|---|---|
| Environmental Factors | Dry air, indoor heating/cooling, smoke, wind | Exposure to pollutants, excessive sun exposure |
| Lifestyle Choices | Lack of blinking, insufficient hydration, poor nutrition | Sedentary lifestyle, inadequate sleep |
| Medical Conditions | Sjögren’s syndrome, rheumatoid arthritis, diabetes | Age-related changes, eye trauma |
| Medications | Antihistamines, diuretics, antidepressants | Certain medications |
Symptoms and Diagnosis
Identifying the specific cause of symptoms is crucial for effective treatment. Overlapping symptoms between dry eyes and floaters can make diagnosis challenging. Understanding the unique characteristics of each condition, along with the diagnostic methods used, is essential for accurate treatment planning.Accurate diagnosis is vital in determining the appropriate treatment for both dry eyes and floaters. A misdiagnosis can lead to ineffective therapies and potentially prolong discomfort.
Proper differentiation between floaters associated with dry eyes and other potential causes is essential for successful management.
Symptoms of Dry Eyes
Dry eyes are characterized by a persistent feeling of dryness, irritation, and discomfort in the eyes. Symptoms often include a gritty or sandy sensation, burning, stinging, and excessive tearing. The eyes may also feel tired or fatigued. In some cases, vision may be blurry or hazy, especially in low-light conditions. These symptoms can fluctuate and worsen with environmental factors, such as air conditioning or prolonged computer use.
Symptoms of Floaters
Floaters are small, dark spots or shapes that appear to drift within the field of vision. These can range from subtle specks to more prominent shapes, and they often appear more noticeable when looking at a bright background. While not painful, floaters can be bothersome and even disorienting. They may appear in varying locations and densities within the visual field, and some individuals may experience a sudden increase in the number of floaters.
While dry eyes can sometimes be a nuisance, a recent discovery about the bigfoot family homemade closed loop ( bigfoot family homemade closed loop ) has got me thinking about the connection to eye health. Although there’s no direct link between those fascinating projects and floaters, the thought process about complex systems and potential causes got me wondering if dry eyes could actually contribute to floaters.
It’s definitely a fascinating rabbit hole to explore further, and something I’ll be researching to understand the connection better.
Overlap in Symptoms
Blurry vision is a common symptom that can overlap between dry eyes and floaters. In cases of severe dry eye, the blurring can be significant and affect daily activities. Similarly, floaters can sometimes cause a perception of blurry vision, particularly if numerous or large. This overlap can complicate initial diagnosis. Careful attention to other accompanying symptoms and a comprehensive eye exam are crucial to distinguish the root cause.
Diagnostic Processes
The diagnostic process for dry eyes typically involves a thorough evaluation of symptoms, patient history, and a comprehensive eye exam. The diagnostic process for floaters, on the other hand, may include dilated fundus examination, optical coherence tomography (OCT) scans, or even specialized imaging to evaluate the vitreous humor.
Diagnostic Tests
| Test | Description | Relevance to Dry Eye | Relevance to Floaters |
|---|---|---|---|
| Schirmer test | Measures tear production | Directly assesses tear volume and quality, crucial for dry eye diagnosis. | Indirectly relevant if evaluating overall ocular health, but not directly related to floaters. |
| Tear osmolarity test | Measures the concentration of solutes in tears | Helpful in determining if tears are too concentrated, a key indicator of dry eye. | Indirectly relevant if evaluating overall ocular health, but not directly related to floaters. |
| Slit-lamp examination | A magnified view of the eye’s structures | Identifies surface dryness, inflammation, and other signs of dry eye. | Evaluates the vitreous humor for abnormalities and signs of retinal detachment, a possible cause of floaters. |
| Dilated fundus examination | Examination of the retina and optic nerve | Not directly relevant to dry eye | Crucial for evaluating the health of the retina and identifying possible causes of floaters. |
| Optical Coherence Tomography (OCT) | High-resolution cross-sectional images of the retina | Indirectly relevant in evaluating the health of the back of the eye. | Used to evaluate the vitreous humor and detect potential issues, such as retinal detachment. |
Differentiating Floaters from Dry Eye-Related Causes
A crucial aspect of diagnosis involves differentiating floaters arising from dry eye from other causes, such as age-related changes, trauma, or underlying medical conditions. A comprehensive history, including the onset and duration of symptoms, any recent eye injuries or surgeries, and any associated medical conditions, is essential for accurate differentiation. For example, if floaters suddenly increase in number or size, it could indicate a potential detachment of the retina.
Importance of Accurate Diagnosis
Accurate diagnosis of dry eyes and floaters is critical for effective treatment. Treatments for dry eyes focus on increasing tear production or improving tear quality, while floaters often require different management strategies. Misdiagnosis can lead to inappropriate treatment and potentially exacerbate the condition. For example, treating floaters with eye drops intended for dry eyes will not address the underlying cause of the floaters and could potentially cause further discomfort.
Treatment and Management: Can Dry Eyes Cause Floaters
Managing dry eyes and floaters involves a multifaceted approach tailored to the individual’s specific needs and the severity of the condition. Effective treatment strategies often combine various methods, from topical remedies to lifestyle adjustments, to achieve optimal comfort and vision improvement. Understanding the different treatment options and their potential benefits and drawbacks is crucial for successful management.Addressing both dry eyes and floaters necessitates a careful consideration of the underlying causes and the potential interplay between the two conditions.
For instance, certain medications that treat dry eyes might have side effects that could exacerbate floaters. Likewise, some lifestyle modifications for floaters might incidentally benefit dry eyes. A personalized approach, guided by a healthcare professional, is essential for navigating these considerations.
Dry Eye Treatment Options
Various treatments are available for dry eyes, ranging from over-the-counter remedies to prescription medications. The best course of action depends on the severity and underlying cause of the dryness.
- Artificial Tears: These are often the first line of defense. They provide a lubricating film on the surface of the eye, relieving dryness and discomfort. They come in various forms, including eye drops, gels, and ointments, each with varying durations of effect. Choosing the appropriate consistency is crucial. For example, gels are best for overnight use, providing sustained moisture, while drops offer more immediate relief.
- Medications: Prescription medications, such as Restasis or Xiidra, can help increase tear production. These medications may take several weeks to show full effect and may have potential side effects. Consult with an ophthalmologist to determine if these options are suitable.
- Lifestyle Adjustments: Several lifestyle factors can contribute to dry eyes. These include environmental conditions (dry air, prolonged computer use), certain medications, and underlying medical conditions. Addressing these factors can significantly improve dry eye symptoms. For example, using a humidifier in a dry environment, taking breaks from screen time, and adjusting medication regimens, if applicable, can make a difference.
Floater Treatment Options
Floaters, often harmless, can be a source of visual discomfort. Treatment strategies depend on the severity and nature of the floaters.
- Observation: Many floaters are benign and resolve on their own over time. If floaters are not causing significant visual impairment or discomfort, observation is a reasonable initial approach.
- Surgery: In cases of severe floaters that significantly impact vision or cause persistent discomfort, surgical removal might be considered. This is usually a last resort after other options have been explored. Procedures like vitrectomy, where the vitreous gel is replaced, can be performed to remove floaters, though potential complications exist.
- Other Interventions: Certain therapies, such as laser treatments, may be considered in specific situations. These interventions should only be undertaken under the guidance of a qualified ophthalmologist.
Comparison of Treatment Strategies
Dry eye and floater treatments differ significantly in their approach. Dry eye treatments primarily focus on lubricating and increasing tear production, whereas floater treatments might involve surgical interventions. However, both conditions can be impacted by lifestyle choices.
Potential Complications and Side Effects
Potential complications of dry eye treatments are generally mild and include temporary irritation, stinging, or redness. More serious complications are rare. Side effects of medications for dry eyes can vary, and it is essential to discuss them with a doctor. Potential side effects of surgical procedures for floaters include infection, bleeding, and vision changes. Always discuss potential risks and benefits with a medical professional.
Step-by-Step Procedure for Managing Dry Eyes and Floaters
A personalized step-by-step procedure for managing both dry eyes and floaters should be developed in consultation with a healthcare professional. This involves a thorough evaluation of the patient’s specific needs and a tailored plan for addressing the underlying causes and symptoms.
While dry eyes can sometimes lead to some pretty uncomfortable symptoms, like floaters, they’re not necessarily a direct cause. It’s a bit like how proper support in a sports bra can improve your workout, a crucial factor in preventing discomfort and injury, as detailed in the ultimate guide to sports bras. Ultimately, it’s still important to talk to your eye doctor about any floaters you might be experiencing, regardless of whether you have dry eyes.
Prevention and Lifestyle Factors

Protecting your eyes from dry eye and floaters involves a proactive approach that combines environmental adjustments, lifestyle modifications, and regular check-ups. A holistic approach to eye health is crucial for maintaining optimal vision and reducing the risk of these conditions. Consistent good habits can significantly decrease the likelihood of experiencing these problems.A combination of preventative measures and healthy habits can help mitigate the development and progression of dry eye and floaters.
Understanding how your lifestyle choices influence your eye health is vital for taking control of your well-being.
Environmental Control Strategies
Maintaining a comfortable and stable environment plays a significant role in preventing dry eyes. Controlling humidity levels, air quality, and exposure to irritants can make a substantial difference.
- Humidity Control: Maintaining a proper humidity level in your home and workplace is crucial. Using a humidifier during dry seasons can help prevent the eyes from drying out. Conversely, excessive humidity can also contribute to eye irritation, so it’s important to find a balanced level that suits your environment.
- Air Quality: Exposure to pollutants, dust, and smoke can irritate the eyes, exacerbating dry eye symptoms. Using air purifiers and avoiding exposure to these irritants can greatly reduce discomfort and inflammation.
- Protective Measures: Protecting your eyes from harsh weather conditions like wind and extreme temperatures is vital. Wearing sunglasses during sunny days and using eye protection in dusty or smoky environments can prevent further irritation and dryness.
Lifestyle Choices and Eye Health
Certain lifestyle choices can significantly impact the health of your eyes. Dietary habits, hydration levels, and overall well-being can either contribute to or mitigate the development of dry eye and floaters.
- Diet and Nutrition: A balanced diet rich in vitamins, antioxidants, and essential fatty acids is essential for overall health, including eye health. Foods high in omega-3 fatty acids, such as salmon and flaxseeds, can support healthy tear production. Adequate intake of vitamins A, C, and E, found in fruits and vegetables, can also help protect the eyes from damage.
- Hydration: Maintaining proper hydration is crucial for overall health, and this includes eye health. Dehydration can lead to reduced tear production, contributing to dry eye. Drinking plenty of water throughout the day can help keep your eyes moist and healthy.
- Sleep Hygiene: Adequate sleep is vital for overall health, and this includes eye health. Insufficient sleep can contribute to eye strain and dryness. Prioritizing a regular sleep schedule can support the health of your eyes.
Regular Eye Examinations
Routine eye examinations are essential for early detection and management of both dry eye and floaters. These check-ups allow for a thorough assessment of eye health and can identify potential problems early on.
- Early Detection: Regular eye exams can help detect early signs of dry eye, allowing for timely intervention and management of the condition. Early detection of floaters can also assist in understanding their potential causes and determining the need for further investigation.
- Proactive Management: Eye doctors can recommend personalized strategies for managing dry eye and floaters, such as specific medications or therapies, based on individual needs.
Lifestyle Recommendations
The table below summarizes key lifestyle recommendations for preventing dry eyes and floaters.
While dry eyes can sometimes lead to annoying floaters, it’s a bit like a messy house affecting your overall well-being. Just like a cluttered space can contribute to feelings of overwhelm, similar to how depression and a clean home are connected, eye health and mental clarity are intertwined. So, if you’re noticing more floaters and feeling a bit down, it might be time to reassess your overall lifestyle and look at potential underlying issues beyond just dry eyes.
In short, a healthy home, both physically and mentally, is key to avoiding issues like floaters.
| Lifestyle Factor | Recommendation |
|---|---|
| Environmental Control | Maintain appropriate humidity levels, control air quality, and use protective eyewear. |
| Diet and Nutrition | Consume a balanced diet rich in vitamins, antioxidants, and essential fatty acids, including omega-3s. |
| Hydration | Drink plenty of water throughout the day to maintain proper hydration. |
| Sleep Hygiene | Prioritize a regular sleep schedule to support overall well-being. |
| Regular Eye Exams | Schedule regular eye exams for early detection and proactive management of potential issues. |
Illustrative Cases and Examples
Understanding the relationship between dry eyes and floaters requires looking at real-world scenarios. This section provides hypothetical and real-life examples to illustrate the potential connections and the varying degrees of severity involved. We’ll examine different dry eye conditions, their impact on floaters, and even situations where a dry eye treatment might unexpectedly trigger floaters.
Hypothetical Case Study of a Patient with Dry Eyes and Floaters
A 45-year-old woman, Sarah, experiences intermittent blurry vision and the sensation of tiny specks or “floaters” drifting in her field of vision. She also reports a persistent dryness and stinging sensation in her eyes, especially after prolonged computer work. Her eye examination reveals signs of mild dry eye, characterized by reduced tear film stability and a slightly inflamed conjunctiva.
Given the symptoms, the ophthalmologist suspects a link between the dry eyes and the floaters. Treatment involves prescription eye drops to increase tear production and improve lubrication, along with lifestyle adjustments to reduce eye strain. Follow-up visits and monitoring of her symptoms are crucial to assess the effectiveness of the treatment and to rule out any other underlying conditions.
Different Dry Eye Conditions and Potential Relationship to Floaters
Various dry eye conditions can influence the presence and severity of floaters. For instance, evaporative dry eye, where the eyes don’t produce enough tears, or aqueous deficient dry eye, where the tear production is compromised, can both lead to inflammation and potentially disrupt the delicate structures within the eye. These disruptions can potentially contribute to the formation or increased visibility of floaters.
Another condition, meibomian gland dysfunction, where the oil-producing glands in the eyelids malfunction, can contribute to instability in the tear film and, as a result, the appearance of floaters.
Varying Degrees of Dry Eye Severity and Impact on Floaters
The severity of dry eye significantly impacts the potential impact on floaters. Mild dry eye, often manageable with over-the-counter remedies, may only cause minor discomfort and minimal changes in floaters. However, moderate to severe dry eye, if left untreated, can lead to more pronounced symptoms, such as significant blurring, and a marked increase in the number and intensity of floaters.
The prolonged irritation and inflammation associated with severe dry eye can disrupt the vitreous humor, the gel-like substance filling the eye, potentially increasing the visibility of floaters.
Comprehensive Case History of an Individual Experiencing Floaters with Underlying Dry Eye Issues
A 62-year-old male patient, David, presented with increasing floaters and occasional blurry vision. He reported experiencing mild dryness and burning in his eyes for several months, particularly after prolonged periods of reading or working on his computer. His medical history revealed no prior eye issues. An eye exam revealed signs of moderate dry eye, specifically meibomian gland dysfunction.
Treatment included warm compresses, punctal plugs (to prevent tear drainage), and prescription eye drops. The patient reported a significant reduction in floaters after several weeks of consistent treatment. This case highlights the importance of a thorough eye examination to diagnose and address underlying dry eye issues that might be contributing to floaters.
Hypothetical Scenario Where Floaters are Triggered by a Particular Dry Eye Treatment
A patient using a specific type of preservative-free artificial tear solution to manage their dry eye experienced a sudden increase in floaters. The patient reported the floaters appeared shortly after starting the new eye drops. The ophthalmologist considered the possibility of an allergic reaction to a component in the new solution, which can cause irritation and inflammation in the eye, potentially affecting the vitreous humor and leading to floaters.
The patient was advised to discontinue the new eye drops and try an alternative solution to manage their dry eye symptoms. This scenario emphasizes the importance of monitoring for adverse reactions to any new eye treatment.
Further Research and Considerations
Unraveling the precise connection between dry eyes and floaters remains a complex area of investigation. While emerging research suggests potential correlations, the underlying mechanisms are not yet fully understood. Further exploration is crucial to establish definitive links and develop targeted treatments.The current understanding of the relationship between dry eyes and floaters is still in its nascent stages. A deeper understanding of the intricate interplay between ocular surface health, vitreous humor composition, and the formation of floaters is vital to refining treatment strategies and preventative measures.
Areas of Ongoing Research
Research into the correlation between dry eyes and floaters is ongoing and multifaceted. Studies are examining the impact of tear film instability and dehydration on the vitreous humor. Scientists are investigating whether changes in the vitreous’s viscosity or composition can be linked to the development of floaters in individuals with dry eye syndrome. Further studies may explore the role of inflammatory mediators in both conditions.
Potential inflammatory pathways linking dry eye and floater formation are being investigated.
Potential for Future Studies, Can dry eyes cause floaters
Future research should delve deeper into the pathophysiological mechanisms that could connect dry eyes and floaters. Clinical trials involving larger cohorts of patients are essential to validate the findings from preliminary studies. Longitudinal studies tracking the progression of both dry eyes and floaters over time could provide valuable insights into the relationship between these conditions. Research on the efficacy of specific treatments for dry eyes in preventing or mitigating the development of floaters is warranted.
Furthermore, investigation into the role of genetics in predisposing individuals to both dry eyes and floaters could reveal important insights.
Other Contributing Factors
It’s crucial to recognize that other factors could contribute to both dry eyes and floaters. Age-related changes in the eye, such as a decrease in tear production or alterations in the vitreous, can play a significant role in both conditions. Systemic health conditions, such as autoimmune disorders or diabetes, can also affect both tear production and vitreous health.
Specific medications, such as certain antihistamines or antidepressants, may also contribute to dry eye symptoms and influence vitreous composition.
Examples of Co-occurring Medical Conditions
Several medical conditions can simultaneously affect both the ocular surface and the vitreous humor. For instance, Sjögren’s syndrome is an autoimmune disease that often presents with both dry eyes and a higher likelihood of floaters. Conditions impacting the immune system, such as rheumatoid arthritis, might also present with similar symptoms. Glaucoma patients, especially those with advanced disease stages, can experience a higher incidence of both dry eyes and floaters.
A comprehensive eye examination, including a detailed medical history, is critical to identify any underlying medical conditions that may be influencing both symptoms.
Research Gaps in Understanding the Relationship
| Research Area | Gap Description |
|---|---|
| Pathophysiological Mechanisms | Limited understanding of the direct link between tear film instability and vitreous changes leading to floaters. |
| Longitudinal Studies | Lack of long-term studies following individuals with dry eye symptoms to determine the risk of developing floaters. |
| Impact of Systemic Conditions | Incomplete data on how various systemic diseases influence both dry eye and vitreous conditions. |
| Specific Treatment Efficacy | Insufficient evidence regarding the efficacy of specific dry eye treatments in reducing the occurrence of floaters. |
| Genetic Predisposition | Limited exploration of genetic factors potentially contributing to both dry eye and floaters. |
Final Wrap-Up
In conclusion, the potential relationship between dry eyes and floaters warrants further investigation. While a direct cause-and-effect link isn’t definitively established, understanding the potential mechanisms and overlapping symptoms is crucial for proper diagnosis and effective treatment. Consulting an ophthalmologist is essential for personalized guidance and management of both conditions.
