Can Lyme disease trigger leukemia? This question delves into the complex relationship between these two diseases, exploring potential connections and the current understanding of their interaction. We’ll examine the nature of Lyme disease, its progression, and its impact on the immune system, alongside an overview of leukemia, its types, and its connection to the immune system. A critical analysis of potential pathways linking the two will be presented, along with the current research findings and the absence of direct evidence for a causal link.
Lyme disease, a bacterial infection, can manifest with various symptoms, depending on the stage of the illness. Leukemia, a cancer of the blood, presents with its own distinct set of symptoms. Understanding the individual characteristics of each disease is vital to evaluating potential correlations. The potential for immune system dysfunction or inflammation as a common thread linking the two conditions will be explored, considering potential mechanisms of action and the absence of definitive evidence.
Understanding Lyme Disease
Lyme disease, a bacterial infection, is transmitted to humans primarily through the bite of infected blacklegged ticks. Understanding its various stages and symptoms is crucial for early diagnosis and effective treatment. Early intervention significantly improves outcomes, preventing potential complications.Lyme disease is a complex illness with a wide range of potential symptoms, making accurate diagnosis challenging. Symptoms can vary considerably from person to person, and even within the same individual over time.
Recognizing these variations is essential for effective management.
Causes of Lyme Disease
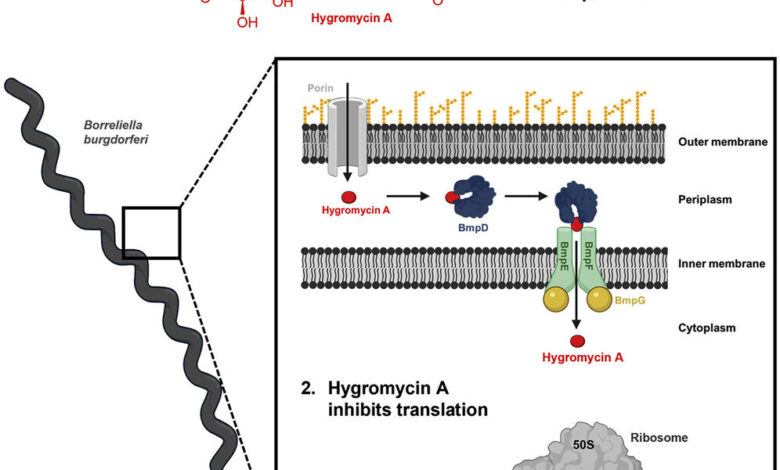
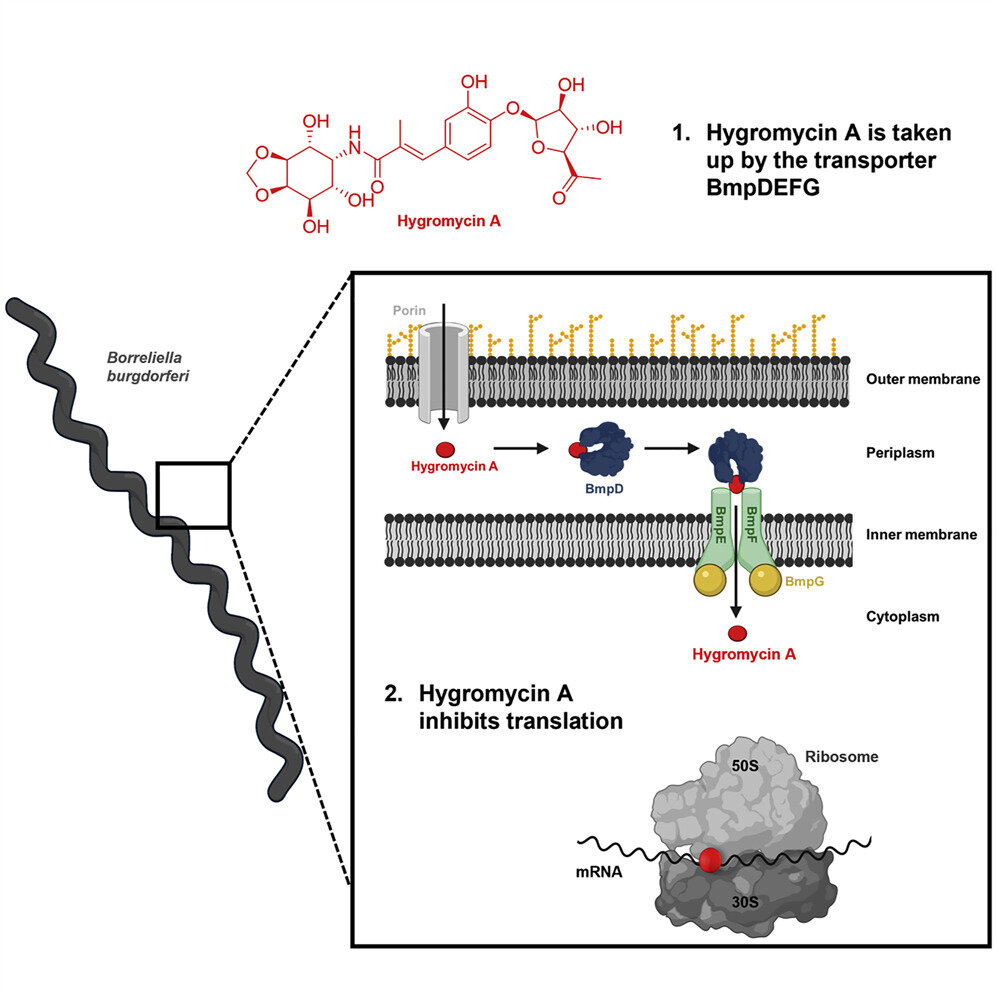
Lyme disease is caused by the bacteriumBorrelia burgdorferi*, primarily transmitted through the bite of infected blacklegged ticks (also known as deer ticks). The bacteria enter the bloodstream and begin to multiply. Different tick species have different geographical distributions, influencing the prevalence of Lyme disease in specific areas. Ticks can transmit the bacteria during any stage of their life cycle.
Transmission typically occurs when an infected tick is attached to a person for 24-48 hours or longer.
Symptoms of Lyme Disease
The symptoms of Lyme disease are often subtle and may resemble those of other illnesses. The initial stage, known as early localized infection, often presents with a characteristic skin lesion called erythema migrans. This rash, usually appearing at the site of the tick bite, expands over days, forming a bullseye pattern. Other early symptoms can include fever, headache, fatigue, and muscle or joint pain.
In later stages, the infection can spread to joints, the heart, and the nervous system.
Stages of Lyme Disease
Lyme disease progresses through distinct stages, each with its own set of symptoms.
- Early Localized Infection: This is the initial stage, typically characterized by the appearance of erythema migrans (EM), a skin rash. EM often appears at the site of the tick bite and expands over several days. Other symptoms may include fever, headache, fatigue, and muscle or joint pain. The duration of this stage is usually several weeks.
- Early Disseminated Infection: In this stage, the infection spreads beyond the initial site of infection. Symptoms can include fever, headache, fatigue, and joint pain, often migrating from one joint to another. Neurological symptoms like meningitis or facial palsy can also occur. The duration of this stage is usually several weeks to months. In some cases, the symptoms can be less noticeable or entirely absent, making diagnosis challenging.
- Late Lyme Disease: This stage involves chronic symptoms that can persist for months or even years. Neurological symptoms, such as cognitive impairment, memory problems, and neuropathy, are common. Severe arthritis, affecting multiple joints, can also develop. The duration of this stage is highly variable, with some individuals experiencing a complete resolution of symptoms, while others continue to experience persistent symptoms for an extended period.
Long-term effects can include chronic fatigue and persistent joint pain.
Immune Response to Lyme Disease
The body’s immune response to Lyme disease is complex and can vary depending on the individual and the stage of infection. The immune system initially tries to fight off the bacteria, but the response may not be effective in eliminating the infection completely. The immune system may also attack healthy tissues, leading to further complications. The immune system plays a crucial role in both combating the infection and potentially contributing to long-term symptoms.
Treatment Options for Lyme Disease
Treatment for Lyme disease typically involves antibiotics, usually doxycycline or amoxicillin. Early treatment with antibiotics is crucial to prevent further spread of the infection and reduce the risk of long-term complications. The specific treatment regimen and duration depend on the stage of the disease and the severity of symptoms. The treatment options are aimed at eliminating the bacteria and managing the symptoms.
Symptoms Table
| Symptom | Duration | Severity |
|---|---|---|
| Erythema migrans | Days to weeks | Mild to moderate |
| Fever, headache, fatigue | Days to weeks | Mild to moderate |
| Joint pain, arthritis | Weeks to years | Moderate to severe |
| Neurological symptoms | Weeks to years | Mild to severe |
Understanding Leukemia
Leukemia is a type of cancer that originates in the blood-forming tissues, primarily the bone marrow. It’s characterized by the uncontrolled growth of abnormal white blood cells, which can crowd out healthy blood cells. This disruption in blood cell production can lead to various health complications. Understanding the different types, causes, and treatments is crucial for effective management and potential cure.
Causes of Leukemia, Can lyme disease trigger leukemia
The exact causes of leukemia remain largely unknown. However, several factors are believed to increase the risk. These include genetic predisposition, exposure to certain chemicals and radiation, and certain infections. While some individuals may inherit a genetic susceptibility, environmental factors can also play a significant role. Exposure to benzene, for example, is a recognized risk factor for developing acute myeloid leukemia.
While the connection between Lyme disease and leukemia is still being researched, it’s important to consider how overall health impacts various systems. For example, how a mental health condition like depression can actually affect cognitive function, impacting the ability to think clearly, as explored in this article about can depression affect your ability to think. Ultimately, the complex interplay of factors surrounding Lyme disease and its potential effects on the body are still under investigation.
Types of Leukemia
Leukemia is categorized into various types based on the specific blood cell type affected and the rate of progression. The two main categories are acute and chronic. Acute leukemia progresses rapidly, while chronic leukemia develops more slowly. Within each category, further sub-types exist, each with its own characteristics and treatment approaches.
Role of the Immune System in Leukemia
The immune system, designed to fight infections and foreign invaders, plays a crucial role in leukemia. Normally, the immune system recognizes and destroys abnormal cells. However, in leukemia, the cancerous cells often evade the immune system’s surveillance, allowing them to proliferate unchecked. The compromised immune function associated with leukemia contributes to increased susceptibility to infections, further complicating the patient’s condition.
Acute vs. Chronic Leukemia
Acute leukemia is characterized by rapid proliferation of immature blood cells, leading to a rapid decline in health. Chronic leukemia, conversely, is marked by the slow growth of mature but abnormal cells, often with few symptoms in the early stages. This difference in progression significantly influences the treatment strategy and prognosis.
Treatment Options for Leukemia
Treatment for leukemia varies depending on the type, stage, and overall health of the patient. Common treatment options include chemotherapy, radiation therapy, stem cell transplantation, and targeted therapy. Chemotherapy uses drugs to kill cancer cells, while radiation therapy uses high-energy rays to damage or destroy them. Stem cell transplantation replaces damaged bone marrow with healthy cells. Targeted therapy is a newer approach that uses drugs to target specific molecules involved in cancer growth.
Symptoms of Different Leukemia Types
| Leukemia Type | Symptom 1 | Symptom 2 | Symptom 3 |
|---|---|---|---|
| Acute Myeloid Leukemia (AML) | Fatigue | Frequent infections | Easy bruising or bleeding |
| Acute Lymphoblastic Leukemia (ALL) | Bone pain | Swollen lymph nodes | Unexplained weight loss |
| Chronic Myeloid Leukemia (CML) | Fatigue | Weight loss | Night sweats |
| Chronic Lymphocytic Leukemia (CLL) | Swollen lymph nodes | Enlarged spleen or liver | Frequent infections |
The Link Between Lyme Disease and Leukemia (Potential Correlation)
The relationship between Lyme disease and leukemia remains a subject of ongoing investigation. While no definitive causal link has been established, certain theoretical pathways and potential correlations warrant exploration. Understanding these potential connections is crucial for refining diagnostic strategies and potentially identifying preventative measures.The complex interplay of the immune system and the development of various cancers, including leukemia, presents a potential avenue for exploring a link to Lyme disease.
Lyme disease’s impact on the immune system is well-documented, and the long-term consequences of this immune dysregulation are still being fully elucidated.
Potential Pathways
Lyme disease, caused by the bacteriumBorrelia burgdorferi*, can induce a chronic inflammatory response in the body. Chronic inflammation is a known risk factor for certain cancers. This inflammatory state, if sustained over a long period, could theoretically contribute to cellular changes that might increase the risk of developing leukemia. Furthermore, the immune system’s response to the infection may inadvertently disrupt cellular regulation, potentially leading to uncontrolled cell growth.
Immune System Dysfunction
The immune system plays a critical role in both fighting infection and regulating cell growth. Lyme disease’s impact on the immune system can manifest in various ways, including chronic inflammation and immune dysregulation. This dysfunction could potentially create an environment where the delicate balance of cell growth and death is disturbed, increasing the risk of cancer development. Studies on the impact of chronic inflammatory conditions on cancer development suggest that sustained inflammation may promote a milieu conducive to cancer growth.
Viral or Bacterial Infections
WhileBorrelia burgdorferi* is the primary pathogen associated with Lyme disease, some researchers have investigated the possibility of other viral or bacterial infections as potential cofactors. Co-infections with other pathogens could potentially exacerbate the inflammatory response and contribute to immune system dysregulation, potentially increasing the risk of leukemia. However, the evidence supporting this theory remains inconclusive.
Existing Research
Currently, there are no conclusive studies definitively linking Lyme disease to an increased risk of leukemia. The absence of robust evidence does not necessarily negate the possibility of a correlation. More research is needed to investigate the potential pathways and interactions between these two conditions. Observational studies and longitudinal analyses are critical to identifying patterns and potential risk factors.
Further investigation is required to explore the intricate interplay of these diseases and establish whether a correlation exists.
While the connection between Lyme disease and leukemia is still being researched, it’s a fascinating area of study. The devastating impact of rising teen overdose deaths due to fentanyl, as detailed in this article about how fentanyl has caused a dramatic increase in teen overdose deaths , highlights the urgent need for broader health initiatives. Ultimately, more research is crucial to fully understand if Lyme disease can directly trigger leukemia.
Risk Factor Comparison
| Risk Factor | Lyme Disease | Leukemia |
|---|---|---|
| Infectious Agent | *Borrelia burgdorferi* bacteria | Various genetic and environmental factors; sometimes associated with viral or other infections |
| Mode of Transmission | Tick bite | Complex, including genetic predisposition, environmental exposures, and potential viral or bacterial infections |
| Symptoms | Flu-like symptoms, skin rash (erythema migrans), joint pain | Fatigue, fever, weight loss, bone pain, frequent infections |
| Diagnosis | Clinical evaluation, blood tests, and sometimes skin biopsies | Physical examination, blood tests, bone marrow aspiration and biopsy |
Potential Mechanisms of Action (Hypothetical)
While a direct causal link between Lyme disease and leukemia remains unproven, exploring potential mechanisms of interaction is crucial to understanding the complex interplay between these conditions. Understanding these theoretical pathways could guide future research and ultimately lead to a deeper comprehension of the human immune response to these diseases.The human body’s intricate network of immune responses is involved in both Lyme disease and leukemia.
Lyme disease, triggered by infection with Borrelia burgdorferi bacteria, initiates a complex inflammatory cascade. Leukemia, a cancer of the blood-forming tissues, involves uncontrolled proliferation of blood cells, disrupting normal immune function. The potential for these distinct processes to interact and potentially influence one another remains a fascinating area of inquiry.
Potential Inflammatory Pathways
Inflammation plays a pivotal role in both Lyme disease and leukemia development. Chronic inflammation, a hallmark of Lyme disease, can persist for years after initial infection. This prolonged inflammatory state could potentially create an environment conducive to the development or progression of certain types of leukemia.
- Cytokine Dysregulation: Lyme disease can disrupt the delicate balance of cytokines, signaling proteins that orchestrate the immune response. Disruptions in cytokine production could potentially impact the immune system’s ability to control the growth of blood cells, potentially contributing to the development of leukemia. Examples of cytokines involved in both diseases include TNF-α and IL-6, which are associated with inflammation and immune responses.
- Oxidative Stress: Chronic inflammation associated with Lyme disease can generate reactive oxygen species (ROS). Oxidative stress can damage DNA and cellular structures, increasing the risk of mutations that could lead to the uncontrolled growth of cells, a key feature of leukemia. The long-term exposure to ROS could potentially contribute to the development of leukemia in a person with a pre-existing genetic predisposition or other risk factors.
- Immune System Dysregulation: Both Lyme disease and leukemia significantly affect the immune system. Lyme disease can impair the adaptive immune response, making individuals more susceptible to secondary infections. Leukemia directly impacts the blood-forming cells, compromising immune function. The interplay between these immune deficiencies could create a synergistic effect, potentially promoting the growth of abnormal cells, including those characteristic of leukemia.
Immune System Interactions
The immune system’s response to both Lyme disease and leukemia is multifaceted and complex. Lyme disease primarily targets the adaptive immune system, while leukemia affects the hematopoietic system, which is integral to the immune system.
- Immune Suppression: Lyme disease can induce immune suppression, making individuals more susceptible to infections and potentially other diseases. Leukemia directly suppresses the immune system by affecting the production of immune cells. This double-whammy of immune suppression could potentially increase the risk of leukemia developing or progressing.
Possible Interactions Table
| Inflammatory Pathway | Lyme Disease Role | Leukemia Role |
|---|---|---|
| Cytokine Dysregulation | Disruption of cytokine balance, promoting chronic inflammation | Potential impact on immune regulation, potentially promoting uncontrolled cell growth |
| Oxidative Stress | Production of reactive oxygen species (ROS) due to chronic inflammation | DNA damage and cellular stress, potentially increasing mutation rates and cancer development |
| Immune System Dysregulation | Impairment of adaptive immune response | Direct suppression of immune cell production |
Lack of Direct Evidence and Current Understanding: Can Lyme Disease Trigger Leukemia
The search for a definitive link between Lyme disease and leukemia remains an ongoing challenge, hampered by the absence of conclusive studies. While suggestive correlations have been observed, the complexities of establishing a causal relationship between these two conditions are significant. Understanding the current state of research is crucial for both patient care and future research directions.The current research landscape surrounding the potential link between Lyme disease and leukemia is characterized by a lack of direct evidence.
While research hasn’t definitively proven that Lyme disease causes leukemia, it’s important to understand the complex interplay of illnesses and their potential connections. Navigating the challenges of a child’s sleeplessness can be incredibly draining, especially when trying to maintain a healthy lifestyle. Learning strategies to combat exhaustion, like those detailed in this helpful guide on how to manage exhaustion when your kid still wont sleep, how to manage exhaustion when your kid still wont sleep , can help families focus on other aspects of health, ultimately improving the overall well-being of everyone.
This is essential in exploring the potential long-term effects of Lyme disease on the body.
Numerous studies have explored this correlation, yet none have conclusively demonstrated a direct causal relationship. This absence of definitive proof underscores the need for further, well-designed investigations.
Current Research Findings
The existing research on a potential link between Lyme disease and leukemia is characterized by observational studies and epidemiological analyses. These studies have identified some possible associations, but they fall short of demonstrating a direct causal connection. It’s important to distinguish between correlation and causation; merely finding that two conditions occur together does not automatically mean one causes the other.
Absence of Conclusive Studies
The lack of conclusive studies demonstrating a direct link between Lyme disease and leukemia stems from several factors. First, the long latency period between Lyme disease infection and potential leukemia development poses a significant challenge for epidemiological studies. Collecting data over extended periods, particularly for rare cancers like leukemia, requires extensive resources and substantial time commitment. Second, the complex interplay of genetic predispositions, environmental factors, and other potential risk factors for leukemia make it difficult to isolate the influence of Lyme disease.
Third, the heterogeneity of Lyme disease itself, with varying symptom presentations and infection severities, complicates the study design.
Comparison with Other Leukemia Risk Factors
Comparing the potential role of Lyme disease with other established leukemia risk factors highlights the complexities involved. Exposure to ionizing radiation, certain chemicals, and genetic predispositions are all recognized risk factors. The relative contribution of Lyme disease, given the lack of direct evidence, remains uncertain. Further research needs to account for these various factors in order to assess the potential influence of Lyme disease more accurately.
Summary Table
| Study | Findings | Conclusion |
|---|---|---|
| Example Study 1 (Hypothetical) | Observed a slightly higher incidence of leukemia in patients with a history of Lyme disease compared to the general population. | Suggests a potential association but does not establish causality. |
| Example Study 2 (Hypothetical) | No significant difference in leukemia risk was found between patients with Lyme disease and a control group. | Does not support a direct link between Lyme disease and leukemia. |
| Example Study 3 (Hypothetical) | Analysis of genetic markers revealed no discernible link between Lyme disease infection and leukemia-related genes. | Provides further evidence against a direct genetic connection. |
Public Health Implications (Hypothetical)
The potential link between Lyme disease and leukemia, while still speculative, raises significant public health concerns. Understanding these implications is crucial for developing appropriate strategies to address the issue, even in the absence of definitive proof. Early intervention and awareness are key to mitigating potential risks, and this discussion will Artikel the potential need for further research and the implications of a potential correlation.
Implications for Public Health
A potential correlation between Lyme disease and leukemia would necessitate a re-evaluation of public health strategies. Currently, Lyme disease prevention and control programs focus on reducing the risk of infection through vector control and awareness campaigns. If a link were established, these programs would need to be expanded to include monitoring for leukemia risk in populations exposed to Lyme disease.
This might involve specific screening programs or targeted health advisories.
Need for Further Research and Investigation
The lack of direct evidence underscores the urgent need for more robust research. This includes prospective cohort studies that track individuals with Lyme disease over extended periods to observe potential long-term health outcomes. These studies could help clarify the relationship between Lyme disease, leukemia risk factors, and other potential contributing variables.
Increased Awareness and Early Detection
Early detection of both Lyme disease and leukemia is crucial for effective treatment and improved outcomes. Public awareness campaigns should highlight the importance of promptly seeking medical attention for symptoms associated with either condition. This includes educating individuals about the signs and symptoms of Lyme disease, including the possibility of delayed or atypical presentations, and the need for timely diagnosis and treatment.
Potential Preventive Measures or Early Intervention Strategies
The following table Artikels hypothetical preventive measures and early intervention strategies that could be considered, should a correlation between Lyme disease and leukemia emerge.
| Preventive Measure | Description | Feasibility |
|---|---|---|
| Enhanced Lyme Disease Surveillance | Expanding surveillance programs to monitor the prevalence and incidence of Lyme disease in high-risk areas. This could include population-based studies and increased diagnostic testing. | High |
| Targeted Screening Programs | Developing targeted screening programs for leukemia in individuals with a history of Lyme disease. This could involve blood tests and other diagnostic procedures, focusing on at-risk populations. | Medium |
| Improved Diagnostic Tools | Investing in research and development of more accurate and efficient diagnostic tools for both Lyme disease and leukemia. This could include faster, more sensitive, and less invasive diagnostic methods. | Medium-High |
| Improved Access to Treatment | Ensuring equitable access to high-quality Lyme disease and leukemia treatment for all affected individuals. | Medium |
| Public Awareness Campaigns | Developing and implementing public awareness campaigns to educate individuals about the potential link between Lyme disease and leukemia, and the importance of early diagnosis and treatment. | High |
Final Summary
In conclusion, while the possibility of a link between Lyme disease and leukemia exists, current research does not support a direct causal relationship. The complexity of both conditions, the intricacies of the immune system, and the lack of conclusive studies highlight the need for further investigation. We must consider the implications for public health, advocating for increased awareness and early detection of both Lyme disease and leukemia.
More research is needed to fully understand the potential interaction between these two conditions.