Can nerve implant help vegetative state? This question probes a frontier of medical innovation, exploring the potential of sophisticated technology to interact with the human brain. Nerve implants, tiny devices that interface with neural pathways, offer a fascinating glimpse into the possibility of restoring function in individuals suffering from severe neurological conditions like the vegetative state. We’ll delve into the science behind these implants, examining their potential applications in revitalizing neural pathways and restoring consciousness in patients in a vegetative state.
We will explore the technicalities, medical implications, and ethical considerations surrounding this groundbreaking field.
The vegetative state, a condition characterized by a loss of awareness and responsiveness, presents a complex challenge to medical science. Understanding the intricate workings of the brain during this state, including the neural pathways and networks affected, is crucial. We will analyze the current state of knowledge about brain function and consciousness to better grasp the potential for nerve implants to interact with the damaged regions of the brain.
Introduction to Nerve Implants
Nerve implants represent a burgeoning field of medical technology, offering the potential to restore lost function and alleviate debilitating conditions. These sophisticated devices aim to bypass damaged neural pathways, transmitting signals directly to the targeted muscles or organs. Their development relies on a combination of sophisticated engineering, material science, and neurosurgical expertise.Nerve implants, essentially artificial neural interfaces, are designed to bridge the gap created by nerve damage or injury.
They mimic the natural function of the nervous system, enabling communication between the brain and the body. This technology holds immense promise for treating a wide range of neurological disorders and enhancing human capabilities.
Materials and Technologies in Nerve Implant Construction
The construction of nerve implants demands a meticulous approach to material selection and technological integration. Biocompatibility is paramount, ensuring the implant does not trigger an adverse immune response in the body. The materials used must be robust enough to withstand the body’s environment and the mechanical forces involved.Common materials include biocompatible polymers, metals like titanium, and specialized composites.
These materials are carefully engineered to ensure long-term stability and maintain electrical conductivity for signal transmission. Advanced manufacturing techniques, including 3D printing and microfabrication, play a crucial role in creating intricate and precise implant structures. The use of advanced materials and fabrication methods allows for the creation of implants that are smaller, more precise, and more efficient than previous generations.
Surgical Procedures for Nerve Implantation
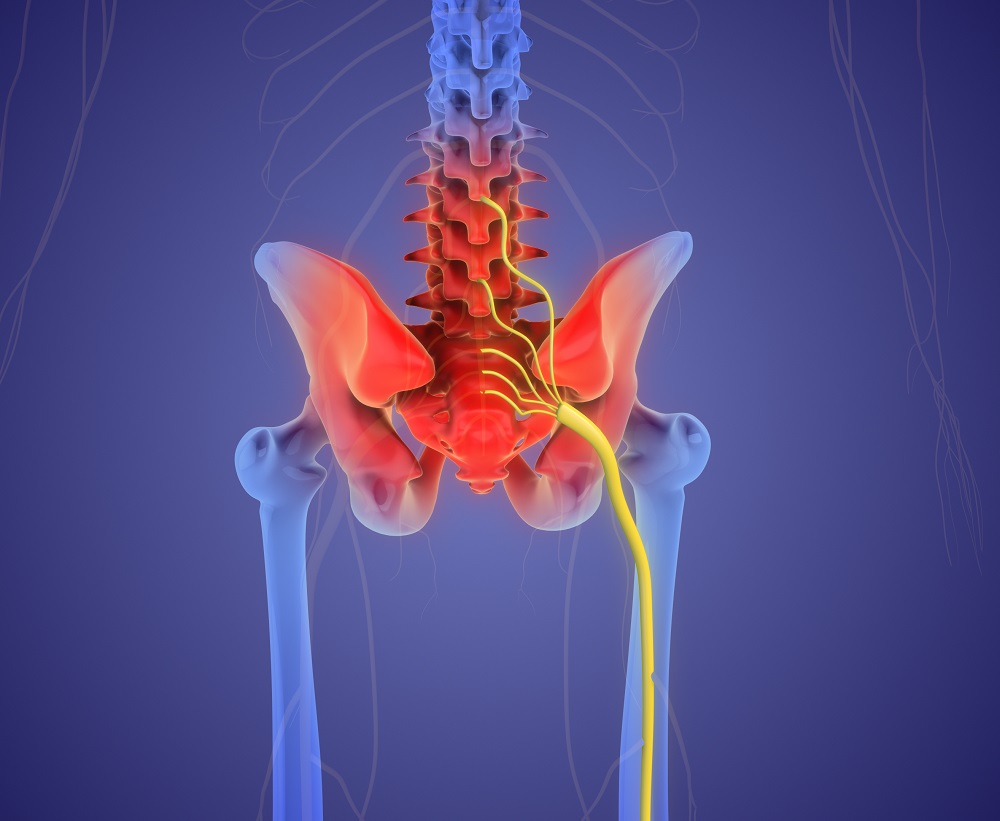
Nerve implant surgery is a complex procedure demanding specialized training and meticulous execution. Precise surgical techniques are crucial to minimize tissue damage and ensure optimal implant placement. Minimally invasive surgical approaches are often preferred to reduce the risk of complications.The procedure typically involves careful identification of the target nerve, precise implant placement, and secure anchoring of the device.
Careful attention to detail and meticulous planning are essential to ensure the implant’s long-term functionality and the patient’s overall well-being. Post-operative monitoring is crucial to assess the implant’s performance and address any potential complications.
Types of Nerve Implants
Different types of nerve implants cater to diverse needs, each with unique features and functionalities. The choice of implant type hinges on the specific nature of the neurological disorder or injury.
- Implants for Peripheral Nerve Repair: These implants are designed to reconnect severed or damaged peripheral nerves, restoring sensory and motor functions. They aim to bridge the gap between severed nerve ends, facilitating signal transmission. Examples include specialized conduits or nerve grafts that encourage nerve regeneration.
- Implants for Spinal Cord Stimulation: These implants are designed to manage chronic pain conditions. They use electrical stimulation to interrupt pain signals in the spinal cord. These implants are particularly helpful for managing neuropathic pain conditions, and the electrical impulses can help to reduce the perception of pain.
- Implants for Deep Brain Stimulation: These implants are used to treat neurological conditions like Parkinson’s disease and essential tremor. They deliver electrical impulses to specific regions of the brain, modulating abnormal neural activity. These implants help to control symptoms associated with these disorders.
Pros and Cons of Different Nerve Implant Types
The efficacy and safety of nerve implants vary based on the specific type. Careful evaluation of potential benefits and drawbacks is essential for informed decision-making.
| Implant Type | Pros | Cons |
|---|---|---|
| Peripheral Nerve Repair | Potentially restores lost function, bridges damaged areas, promotes regeneration. | Requires precise surgery, potential for infection or rejection, long recovery time. |
| Spinal Cord Stimulation | Can effectively manage chronic pain, minimally invasive, and improves quality of life. | Potential for side effects, requires ongoing monitoring, limited effectiveness for all pain conditions. |
| Deep Brain Stimulation | Can alleviate symptoms of neurological disorders, improved quality of life, effective in treating specific conditions. | Requires precise surgical placement, risk of infection or bleeding, potential for device malfunction. |
Vegetative State and Brain Function
The vegetative state, a profoundly debilitating neurological condition, represents a significant challenge in understanding and treating disorders of consciousness. It’s characterized by a loss of awareness and responsiveness to the environment, posing complex questions about the nature of consciousness itself. This condition necessitates a detailed exploration of the brain’s functional changes and the neurological assessments used to diagnose it.Understanding the vegetative state requires a deep dive into the affected neural pathways and networks, coupled with an examination of the brain areas responsible for consciousness and awareness.
The interplay of these elements helps illuminate the complexity of the condition and the potential for therapeutic interventions. A critical analysis of the neurological assessments used in diagnosis provides crucial context, enabling a nuanced understanding of the challenges inherent in assessing such subtle changes in brain function.
Characteristics of a Vegetative State
The vegetative state is defined by a persistent loss of responsiveness to external stimuli. Patients exhibit a lack of awareness of their surroundings and reduced or absent voluntary movements. This state often follows severe brain injury, typically resulting from traumatic events or anoxic brain injury. The impact on brain function is multifaceted, affecting various cognitive and behavioral domains.
The patient may display sleep-wake cycles, but lacks any evidence of comprehension or purposeful behavior.
Neural Pathways and Networks Affected
The vegetative state involves disruptions in numerous neural pathways and networks critical for consciousness and awareness. The precise pathways and networks impacted vary depending on the specific nature and location of the brain injury. These disruptions typically affect the intricate connections between the brainstem, thalamus, and cerebral cortex. The disruption of these pathways can hinder the processing of sensory information, leading to reduced responsiveness and a loss of awareness.
Areas of the Brain Responsible for Consciousness and Awareness
Consciousness and awareness are complex functions intricately linked to specific brain regions. The prefrontal cortex, parietal cortex, and temporal cortex play a critical role in higher-level cognitive functions, including attention, working memory, and self-awareness. The thalamus, a key relay center, processes sensory information and relays it to the cortex. The brainstem, a vital connection between the brain and the spinal cord, is essential for basic life functions and consciousness.
Disruptions in these areas or the communication between them contribute to the diminished awareness observed in a vegetative state.
Neurological Assessments Used to Diagnose a Vegetative State
A variety of neurological assessments are employed to diagnose a vegetative state. These assessments aim to evaluate the patient’s level of responsiveness, awareness, and cognitive function. The Glasgow Coma Scale (GCS) is a widely used tool for evaluating the depth and level of consciousness. It assesses eye opening, verbal response, and motor response. Other crucial assessments include bedside evaluations of the patient’s spontaneous movements, verbalizations, and reactions to stimuli.
Furthermore, electroencephalogram (EEG) monitoring is used to analyze brainwave activity, potentially revealing patterns indicative of consciousness or the absence thereof.
Brain Activity Comparison: Vegetative vs. Conscious State
| Characteristic | Vegetative State | Conscious State |
|---|---|---|
| Awareness | Absent or severely diminished | Present and responsive |
| Spontaneous movements | Limited or absent, often reflexive | Voluntary and purposeful |
| Verbal responses | Absent or non-purposeful | Appropriate and meaningful |
| Cognitive functions | Severely impaired or absent | Intact and functional |
| Brainwave activity (EEG) | May exhibit patterns suggestive of altered states of arousal | Displays characteristic patterns associated with wakefulness and cognitive processes |
Potential of Nerve Implants in Vegetative State Patients
Nerve implants, while still in their early stages of development, hold immense promise for treating a wide range of neurological conditions. The possibility of restoring lost function in patients in a vegetative state is particularly compelling, though significant challenges remain. This exploration delves into the theoretical potential of these implants in this context, considering the specific hurdles and opportunities.Nerve implants, in theory, can stimulate or restore neural pathways that have been damaged or disrupted due to injury or disease.
The effectiveness of this approach hinges on the precise targeting of these implants and their ability to interact with the remaining active neural networks within the brain. The success rate will be highly dependent on the nature and extent of the brain damage in each individual case.
Nerve implants hold promise for treating those in a vegetative state, but navigating the ethical considerations is crucial. A key part of any such procedure is informed consent, which ensures patients (or their legal representatives) fully understand the potential risks and benefits before agreeing to treatment. Understanding what is informed consent is vital to ensure ethical and responsible implementation of these potentially life-changing technologies.
Ultimately, the decision of whether nerve implants can truly help someone in a vegetative state hinges on a thorough understanding of these ethical frameworks.
Types of Nerve Implants and Their Potential
Different types of nerve implants possess varying capabilities in stimulating or restoring neural pathways. Electrochemical implants, for instance, can deliver electrical pulses to stimulate neurons, potentially mimicking natural neural activity. These implants could potentially trigger responses in the damaged brain regions. Conversely, implantable biosensors might provide valuable insights into the patient’s neural activity, aiding in the fine-tuning of stimulation protocols.
Interaction with Damaged Brain Regions
Nerve implants could potentially interact with damaged brain regions in several ways. One possibility involves stimulating residual neural pathways that have not been entirely severed. This stimulation could trigger the reactivation of dormant neurons or the formation of new connections. Another possibility involves using the implants to bypass damaged areas, connecting healthy neural regions to facilitate communication.
Furthermore, the implants could potentially modulate the activity of surrounding neurons, potentially reducing the severity of brain damage and improving overall brain function. The success of this approach will be highly variable, depending on the location and extent of the brain damage.
Potential Benefits and Risks
The potential benefits of using nerve implants in vegetative state patients are significant, potentially restoring lost functions and improving the quality of life. Improved communication, movement, and cognitive abilities are all possible outcomes. However, the risks are also substantial. Complications can arise from the implantation procedure itself, including infection, bleeding, or rejection of the implant. Furthermore, the long-term effects on the brain and body are not fully understood.
Proper risk assessment and careful monitoring of patient responses are critical.
Long-Term Effects on Brain and Body
The long-term effects of nerve implants on the brain and body are still largely unknown. While some studies have shown positive outcomes in animal models, translating those findings to human patients presents numerous challenges. The brain’s plasticity and the potential for both positive and negative adaptations in response to implant stimulation need careful consideration. Potential risks, such as chronic inflammation or the development of unwanted neural pathways, warrant ongoing investigation and monitoring.
Ethical and Societal Considerations
Nerve implants, while holding immense promise for treating the vegetative state, raise complex ethical and societal questions. The potential for profound impact on patients’ lives necessitates careful consideration of the implications beyond the purely medical. These considerations extend to the patient’s autonomy, the role of family and caregivers, and the wider societal implications of this transformative technology.The profound nature of these interventions demands a rigorous ethical framework.
Questions surrounding informed consent, patient autonomy, and the potential for unintended consequences must be addressed proactively. The potential for misuse or exploitation, particularly within vulnerable populations, underscores the need for transparent and responsible development and implementation.
Ethical Implications of Nerve Implants
The use of nerve implants to treat patients in a vegetative state raises critical ethical dilemmas. Crucially, the concept of “quality of life” takes center stage. Can a person in a vegetative state benefit from an implant that might introduce a degree of awareness or responsiveness? Defining and measuring such improvements presents significant challenges.Furthermore, ensuring informed consent in cases where the patient lacks capacity to consent is a significant hurdle.
Determining who speaks on behalf of the patient, balancing the patient’s potential benefits with the risks, and ensuring fairness in access to this technology are vital. The ethical considerations extend to the potential for misuse or exploitation. Robust safeguards are needed to prevent this technology from being used in ways that could harm patients or violate their rights.
Societal Impacts of Nerve Implants
The societal impacts of nerve implant technology are substantial. This technology could revolutionize healthcare, offering possibilities for treating a range of neurological disorders beyond the vegetative state. However, equitable access to such advanced therapies is paramount. Potential disparities in access based on socioeconomic factors or geographical location must be addressed proactively.The potential for enhanced cognitive function or altered consciousness raises profound questions about the nature of humanity and the very definition of personhood.
Societal norms and expectations surrounding human capabilities and limitations may need to adapt to the reality of this technology.
Public Perception and Acceptance
Public perception and acceptance of nerve implant treatments are crucial factors. Open and transparent communication about the technology’s benefits and limitations is essential. Public engagement in discussions about ethical frameworks and societal implications is vital to ensure informed consent. This requires clear, accessible information to foster trust and understanding.
Need for Strict Guidelines and Regulations
Establishing strict guidelines and regulations is paramount to ensure responsible use. Clear legal frameworks are necessary to address issues such as liability, data privacy, and potential misuse. International collaboration and standardized protocols are critical to navigating the global implications of this technology.
Potential Concerns and Challenges
The implementation of nerve implant technology presents several concerns and challenges. One key challenge is ensuring the safety and efficacy of these implants over the long term. The potential for unforeseen side effects or complications needs rigorous evaluation.Another concern is the potential for exacerbating existing inequalities in healthcare access. Ensuring equitable access to these advanced treatments is crucial.
The financial burden of implant procedures and ongoing maintenance could create significant barriers for certain populations.
- Accessibility and Equity: Ensuring equitable access to nerve implant technology for all patients, regardless of socioeconomic status or geographical location, is essential to avoid exacerbating existing health disparities.
- Long-Term Effects: Rigorous long-term studies are necessary to fully understand the potential risks and benefits of nerve implants, including potential side effects, complications, and degradation over time.
- Informed Consent: Robust frameworks for obtaining informed consent from patients, or surrogate decision-makers in cases of incapacity, are crucial to uphold patient autonomy and prevent coercion or exploitation.
- Data Privacy and Security: Protecting patient data associated with nerve implants is paramount to maintain confidentiality and prevent unauthorized access or misuse.
Current Research and Clinical Trials
Nerve implants, while promising, face significant hurdles in the realm of neurological disorders. Translating promising lab research into effective clinical treatments requires rigorous testing and careful consideration of potential risks and benefits. Current research focuses on developing safer and more effective implant designs, as well as improving our understanding of how these implants interact with the nervous system.Ongoing research into nerve implants for treating neurological disorders, including those affecting patients in a vegetative state, is exploring various methods and approaches.
Clinical trials provide crucial data to assess the safety and efficacy of these innovative therapies.
Ongoing Research in Neurological Disorders
Research on nerve implants for treating neurological disorders encompasses a wide range of conditions, beyond the vegetative state. This includes exploring their potential for treating Parkinson’s disease, spinal cord injuries, and stroke recovery. Researchers are working on improving the design and functionality of these implants, striving to minimize invasiveness and maximize therapeutic outcomes. This involves developing biocompatible materials, sophisticated microelectronics, and advanced stimulation protocols.
While nerve implants hold promise for treating conditions like vegetative states, it’s a complex area. Learning how to stay safe while pool hopping, like checking the water depth and ensuring proper supervision, can offer similar careful considerations when dealing with advanced medical interventions. Safety measures, like those outlined in pool hopping staying safe , highlight the importance of cautious planning and preparation for any medical procedure.
Ultimately, exploring the potential of nerve implants for patients in vegetative states requires a similar thoughtful, measured approach to maximizing the chance of positive outcomes.
The goal is to create implants that can reliably and precisely deliver targeted electrical signals to specific nerve pathways.
Clinical Trials in Vegetative State Patients, Can nerve implant help vegetative state
Currently, limited clinical trials directly address the use of nerve implants in patients in a vegetative state. The complexity of this condition, coupled with the ethical considerations surrounding invasive procedures in vulnerable populations, means that research is often exploratory.
While nerve implants show promise in potentially restoring function in patients with severe neurological conditions, like those in a vegetative state, the complexities of such interventions remain significant. Ted Turner’s struggles with Lewy body dementia, detailed in this fascinating article about Ted Turner and Lewy body dementia , highlight the immense challenges in treating such debilitating neurological diseases.
Ultimately, the question of whether nerve implants can effectively treat a vegetative state remains a subject of ongoing research and debate.
Methods Used in Trials
Methods used in trials involving nerve implants in patients with neurological disorders, including those in a vegetative state, typically involve implanting electrodes or other stimulating devices directly into specific brain regions or nerve pathways. These implants are often designed to deliver precisely targeted electrical stimulation, which can modulate neural activity. The stimulation parameters, such as frequency, intensity, and duration, are carefully controlled and adjusted based on individual patient responses.
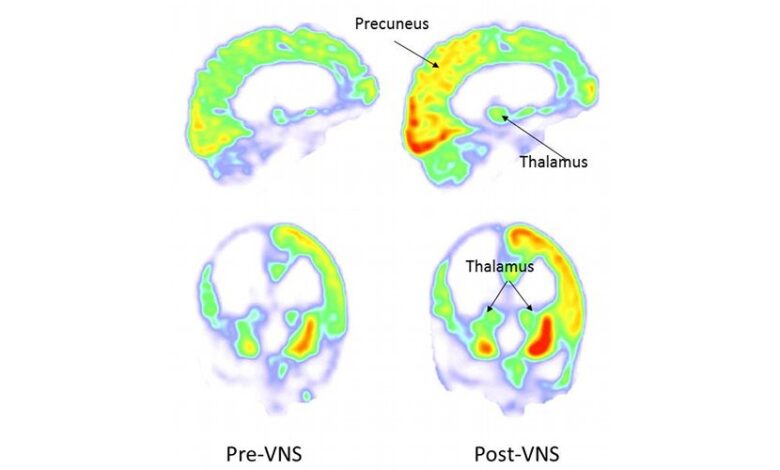
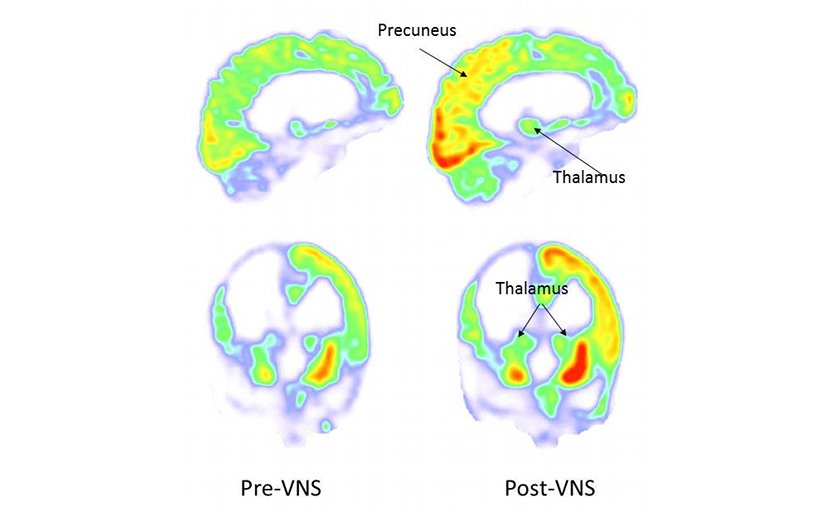
Neuroimaging techniques, like fMRI and EEG, are frequently used to monitor brain activity and evaluate the effects of the implant on neural networks.
Results and Outcomes Observed
Initial results from clinical trials involving nerve implants in patients with neurological disorders are, in many cases, preliminary and not always conclusive. There are challenges in determining meaningful functional improvements in patients with severe neurological impairments. Positive outcomes, when observed, often relate to improvements in basic motor functions or subtle changes in brain activity, rather than dramatic or immediate recoveries.
Further long-term studies are needed to fully assess the potential benefits and risks of this intervention. For instance, a specific trial might show a slight improvement in eye movement, which, when combined with other non-invasive therapies, could potentially improve the patient’s quality of life.
Summary of Key Findings
| Trial | Focus | Methods | Preliminary Results | Limitations |
|---|---|---|---|---|
| Example Trial 1 | Stimulation of specific brain regions | Implantation of electrodes; controlled electrical stimulation | Slight improvements in eye movement; no significant functional recovery | Small sample size; long-term follow-up needed |
| Example Trial 2 | Targeting specific motor pathways | Implantable device delivering electrical impulses | Modest improvements in muscle activation | Limited data on impact on consciousness; further studies needed |
Future Directions and Innovations: Can Nerve Implant Help Vegetative State
Nerve implants, while showing promise in restoring function, face significant hurdles in achieving widespread clinical application. Future advancements will hinge on refining current technologies and addressing existing challenges, pushing the boundaries of what’s possible in stimulating neural activity and ultimately, restoring lost function. This exploration delves into potential future developments, breakthroughs in neural stimulation, and the crucial challenges of improving implant safety and efficacy.The field of neural prosthetics is constantly evolving, driven by a relentless pursuit of more effective and less invasive approaches.
Advancements in materials science, microelectronics, and biocompatibility will be critical in realizing the full potential of nerve implants. These developments promise to enhance the longevity, safety, and performance of these devices.
Potential Breakthroughs in Stimulating Neural Activity
Further advancements in stimulating neural activity will rely on refining the precision and targeting of electrical impulses. Scientists are exploring the use of advanced neuromodulation techniques, such as optogenetics and magnetic stimulation, to enhance the selectivity and efficiency of stimulation. These techniques hold the potential to elicit more nuanced and targeted responses, minimizing unintended side effects. For example, precise stimulation could potentially differentiate between specific motor neurons, leading to more controlled and complex movements.
Further research is also focusing on understanding the intricate interplay of neural networks to more accurately mimic natural signaling patterns.
Challenges in Making Nerve Implants More Effective and Safe
One of the paramount challenges lies in improving the long-term efficacy and safety of nerve implants. Biocompatibility issues, such as tissue rejection and the formation of scar tissue, significantly impact the lifespan of these devices. Future research will focus on developing biocompatible materials and coatings to minimize these adverse reactions. Furthermore, ensuring the stability and reliability of the neural interface over time is critical.
This necessitates the development of robust, durable, and adaptable implant designs. The potential for infection and chronic inflammation around the implant site also poses a considerable concern.
Advancements in Monitoring and Managing Nerve Implants
The ability to continuously monitor the performance and safety of nerve implants is essential for long-term success. Researchers are investigating non-invasive monitoring techniques, such as electroencephalography (EEG) and functional magnetic resonance imaging (fMRI), to track the activity of the implanted system. These methods can provide real-time feedback on the implant’s functionality and help identify any potential complications early.
The development of wireless communication systems will allow for remote monitoring and adjustments to the stimulation parameters, further improving patient management. Furthermore, sophisticated algorithms for analyzing neural data will be crucial for optimizing stimulation protocols and personalized treatment strategies.
Potential Advancements in Monitoring and Managing Nerve Implants
Continuous advancements in wireless communication systems will enable remote monitoring and adjustments of stimulation parameters. This will significantly improve patient management and allow for personalized treatment approaches. Moreover, sophisticated algorithms for analyzing neural data will play a crucial role in optimizing stimulation protocols. This will enhance the accuracy and effectiveness of nerve implants, potentially leading to more personalized and efficient treatment strategies for individuals with neurological impairments.
Long-Term Implications of this Technology
The long-term implications of nerve implant technology are profound. Beyond restoring function in individuals with neurological disorders, such as the vegetative state, these advancements hold the potential to treat a broader range of neurological conditions, including stroke, spinal cord injuries, and even age-related cognitive decline. Ultimately, this technology could transform the way we approach neurological rehabilitation and treatment, offering new hope and opportunities for improved quality of life.
The societal impact will be immense, as these advancements could potentially improve the lives of millions, while simultaneously creating new challenges in ethical considerations and access to care.
Conclusion
In conclusion, the possibility of using nerve implants to treat patients in a vegetative state is a topic filled with both immense promise and significant challenges. While research shows potential for restoring function, significant ethical and practical hurdles remain. Further research, careful ethical consideration, and transparent public discourse are essential for navigating this complex landscape and ensuring that such advancements are utilized responsibly and ethically.
The future of nerve implant technology in treating neurological disorders like the vegetative state remains uncertain, but the ongoing pursuit of innovative solutions holds the key to improving the lives of those affected.
