Can you catch omicron twice what we know now – Can you catch omicron twice? What we know now is that reinfection with Omicron, while possible, is not fully understood. Early data suggests it might happen, but the specifics, like how often, and why, are still being studied. This exploration dives into the current scientific understanding of Omicron reinfection, examining factors like immune response, viral evolution, and potential public health implications.
The factors influencing reinfection rates are complex, encompassing prior infection type, vaccination status, and individual immune system variations. We’ll analyze existing data, identify trends, and discuss the immune response in reinfected individuals, comparing and contrasting vaccinated and unvaccinated groups. Understanding this is crucial for refining pandemic preparedness and potentially predicting future infection waves.
Understanding Reinfection: Can You Catch Omicron Twice What We Know Now
Reinfection with the Omicron variant, and indeed with any variant of the SARS-CoV-2 virus, is a complex issue. While the initial wave of infections sparked considerable concern, the current scientific consensus suggests that reinfection is a possibility, though not necessarily a common occurrence. Understanding the mechanisms behind reinfection is crucial for developing effective public health strategies and informing individual decisions.The current scientific understanding of reinfection with the Omicron variant highlights a nuanced interplay between immune responses and viral evolution.
Reinfection, in the context of the Omicron variant, is not simply a matter of a complete failure of the immune system.
Mechanisms of Reinfection
Reinfection with the Omicron variant can occur due to a variety of factors, including the immune system’s response to the virus. The immune response, though effective against initial infection, might not fully neutralize all Omicron subvariants or lineages, leaving individuals vulnerable to reinfection. Viral evolution plays a significant role, as mutations in the Omicron variant’s spike protein can alter its interaction with host cells, potentially evading the immune system’s recognition and defense mechanisms.
This evolution can contribute to the likelihood of reinfection.
Factors Influencing Reinfection Likelihood
Several factors contribute to the likelihood of reinfection with the Omicron variant. Prior infection type, vaccination status, and individual immune system variations all play a part. Individuals previously infected with other SARS-CoV-2 variants may still have some degree of immunity, but it may not be fully protective against reinfection with Omicron. Vaccination significantly enhances protection against severe disease, but it does not guarantee complete prevention of infection or reinfection.
So, can you get Omicron twice? The current understanding is that reinfection is possible, though the specifics are still being studied. This begs the question of overall health, and how factors like diet might influence our susceptibility. For example, ensuring a nutritious diet, especially for older adults, is crucial for maintaining a robust immune system. Check out this article on quality of diet for older adults has declined heres how to fix it to learn more about how diet plays a role in maintaining health and potentially reducing the risk of reinfection with any virus.
Ultimately, a healthy lifestyle encompassing proper nutrition likely plays a role in preventing reinfection, but more research is needed to fully understand the complexities of viral reinfections.
Individual immune responses differ, and some individuals may have a weaker or less robust immune response than others. This variation in immune system response directly impacts the likelihood of reinfection.
Comparison of Reinfection Rates
Comparing reinfection rates between Omicron and other variants requires careful analysis of epidemiological data. While precise data on reinfection rates for each variant are still being collected and analyzed, ongoing studies are providing insights into these trends. Early data suggest that reinfection rates with Omicron may differ from those seen with other variants, though more research is needed to fully understand these differences.
Severity of Reinfections
The severity of reinfection with the Omicron variant often differs from the initial infection. While reinfection can still lead to mild or moderate symptoms, the severity of reinfection can vary significantly depending on factors like the individual’s overall health and immune response, vaccination status, and the specific Omicron subvariant involved.
Data Analysis and Trends
Analyzing reinfection rates with Omicron is crucial for understanding its long-term impact and developing effective public health strategies. The available data, while still emerging, allows us to begin drawing some preliminary conclusions about the virus’s behavior. Understanding these trends is vital for tailoring preventative measures and resource allocation.
Omicron Reinfection Cases: A Summary
The available data on Omicron reinfections is still relatively limited, making definitive conclusions challenging. However, some reports suggest a notable reinfection rate. Comprehensive data collection and analysis are necessary to fully understand the phenomenon.
| Reported Cases | Geographic Locations | Timeframe |
|---|---|---|
| Limited data currently available | Various countries and regions | Mostly recent months |
Trends in Reinfection Rates
Reinfection rates with Omicron are likely influenced by several factors, including the specific viral variant circulating, the effectiveness of preventive measures, and the overall population’s immunity levels. Identifying potential seasonal patterns in reinfection is also important, as seasonal variations could affect the spread and severity of respiratory infections. Further research is needed to understand these dynamics fully.
Comparison with Other Respiratory Viruses
Comparing Omicron reinfection rates with other respiratory viruses, such as influenza or common cold, can provide context and perspective.
| Virus | Reinfection Rate (Estimated) | Notes |
|---|---|---|
| Omicron | Data is limited, but preliminary reports suggest a possibility of reinfection. | Requires further research to determine precise rates. |
| Influenza | Generally, higher reinfection rates than other respiratory viruses. | Seasonal variations significantly impact reinfection patterns. |
| Common Cold | High reinfection rates due to numerous strains. | Reinfections are often with different strains. |
Effectiveness of Vaccines Against Omicron Reinfection
The effectiveness of vaccines against reinfection with Omicron is an active area of research.
| Vaccine Type | Dosage | Effectiveness Against Reinfection (Preliminary Data) | Notes |
|---|---|---|---|
| mRNA vaccines (e.g., Pfizer, Moderna) | Standard dosage | Data suggests varying degrees of protection, but not complete prevention. | Further research needed to establish precise efficacy. |
| Other vaccine types | Standard dosage | Limited data is available, requiring more research. | Factors like individual immune responses play a role. |
Visual Representation of Data
A bar graph illustrating the limited data on Omicron reinfection rates would show the number of reported cases in different geographic regions over time. The x-axis would represent time (e.g., months), and the y-axis would represent the number of reinfection cases. Different colors could represent various geographic regions, allowing a quick visual comparison of the trends. The graph would clearly highlight the limited data available at this stage, which prevents drawing definite conclusions.
The graph would help to visualize the need for more extensive data collection and analysis.
Immune Response to Reinfection
Understanding how the immune system responds to reinfection with Omicron is crucial for predicting the course of future outbreaks and developing effective strategies for preventing severe illness. Recent research reveals nuanced patterns in the immune response, differing from the initial infection and depending on factors like prior vaccination status. This detailed look will delve into the specific mechanisms and observations surrounding reinfection.The immune system’s response to reinfection with Omicron involves a complex interplay of antibody and T-cell activity.
Antibodies, produced during the initial infection or vaccination, are designed to neutralize the virus. However, the emergence of new variants, like Omicron, can sometimes lead to reduced neutralization capacity, particularly with earlier strains of antibodies. T-cells, a different arm of the immune response, target infected cells directly. They also play a crucial role in the long-term immunity and response to reinfection.
Antibody Response to Reinfection
The antibody response to reinfection with Omicron is characterized by a mix of both reduced and enhanced activity. Studies have demonstrated that some individuals experience a significant boost in antibody production upon reinfection, potentially reflecting the immune system’s ability to adapt and improve its targeting mechanisms. Other individuals might show a more limited response, potentially highlighting the variable nature of the immune system’s adaptation to the specific Omicron variant.
T-cell Response to Reinfection
T-cell responses are also vital in the context of reinfection. T-cells, specifically CD4+ and CD8+ T cells, play a significant role in recognizing and eliminating infected cells. Observations suggest that T-cell responses tend to persist longer than antibody responses and are crucial for controlling viral replication during reinfection. The memory T-cells, primed by the initial infection or vaccination, are activated during reinfection, leading to a faster and more effective immune response.
Recent research is still exploring whether you can get Omicron twice, but it seems likely that reinfection is possible. Considering the importance of keeping kids healthy, especially those with asthma, learning about safe swimming practices for children with asthma is crucial. Swimming for children with asthma can be a fun and healthy activity, but understanding potential respiratory risks is essential.
This knowledge will help us better understand the overall picture of Omicron’s spread and potential for reinfection.
Role of Memory B and T Cells
Memory B cells and T cells are essential for a strong immune response to reinfection. Memory B cells quickly produce antibodies that recognize the Omicron variant, helping to neutralize the virus. Memory T cells also play a vital role, effectively eliminating infected cells before the virus can replicate widely. This highlights the importance of long-term immune memory in protecting against reinfection.
Individuals with robust memory B and T cell responses are more likely to experience milder reinfection symptoms.
Comparison of Immune Response in Vaccinated vs. Unvaccinated Individuals
The immune response to reinfection varies significantly between vaccinated and unvaccinated individuals. Vaccinated individuals, often showing higher antibody titers and robust T-cell responses, tend to experience milder reinfection symptoms compared to unvaccinated individuals. These responses often correlate with a reduced viral load and faster clearance of the virus. The presence of pre-existing immunity, provided by prior vaccination, is critical in mitigating the severity of reinfection.
Duration of Immunity After Initial Infection or Vaccination
Studies on the duration of immunity after Omicron infection or vaccination are ongoing. Early findings suggest that protection against reinfection wanes over time, but the rate and extent of this decline can differ among individuals. Factors like age, overall health, and genetic predisposition influence the duration and intensity of immunity. This highlights the need for ongoing monitoring of immunity levels to reinfection.
Furthermore, booster doses might be required to maintain adequate protection over time.
Public Health Implications
Omicron’s potential for reinfection presents a complex set of public health implications. Understanding these implications is crucial for crafting effective strategies to mitigate the virus’s impact and improve pandemic preparedness. The implications extend beyond individual cases to encompass the overall burden on healthcare systems and the effectiveness of current interventions.The ability of Omicron to reinfect individuals significantly impacts healthcare systems.
Increased hospitalizations and intensive care unit (ICU) admissions could strain resources, especially if the reinfection rate is substantial and leads to more severe illness in some cases. This is particularly relevant for vulnerable populations, who might experience more severe disease trajectories upon reinfection.
Impact on Healthcare Systems
Increased demand on healthcare resources is a primary concern. Reinfection rates will influence the number of patients needing medical attention, potentially overwhelming hospital capacity. This could lead to longer wait times for non-COVID-19 patients, impacting overall healthcare service delivery. The need for surge capacity and contingency plans for healthcare facilities is evident. This also highlights the importance of effective resource allocation strategies.
Implications for Vaccine Strategies and Booster Recommendations
Omicron’s ability to reinfect individuals raises questions about the effectiveness of existing vaccines. The effectiveness of vaccines against reinfection, including the development of new variants, needs careful evaluation. The data on vaccine effectiveness against reinfection with Omicron will be critical in determining the need for new or updated vaccine strategies. Booster shots, including tailored formulations, may be needed to bolster immunity against reinfection.
While we’re still learning about Omicron’s behavior, the current understanding suggests reinfection is possible. This uncertainty highlights the need for continued research, and perhaps, the potential for breakthroughs in other areas like regenerative medicine to bolster our immune systems. Regenerative medicine has bright future holds promise for developing novel therapies that could enhance our body’s defenses against future viral threats, ultimately potentially affecting how easily we can catch Omicron, or similar viruses, again.
So, the answer to whether you can catch Omicron twice remains a bit up in the air for now.
Public health officials will need to carefully consider the efficacy of different vaccine strategies against reinfection.
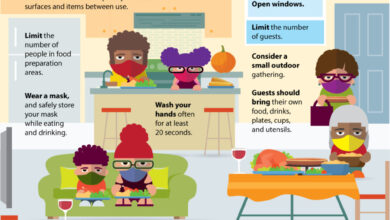
Impact on Infection Control Measures
Infection control measures are crucial in mitigating the spread of the virus. Understanding the reinfection rate will allow for the refinement of infection control strategies. For example, public health authorities may need to adjust guidelines regarding masking, social distancing, and hygiene protocols. Public health strategies may require updated guidelines based on Omicron reinfection rates.
Influence on Future Pandemic Preparedness
The reinfection rate of Omicron will significantly inform future pandemic preparedness. This data will be critical in modeling and anticipating future infection waves. Analysis of Omicron reinfection rates will help in developing strategies for pandemic response. Improved models for predicting future infection waves will be crucial for better resource allocation and efficient public health interventions.
Refining Models Predicting Future Infection Waves, Can you catch omicron twice what we know now
Data on Omicron reinfection rates can refine existing models used to predict future infection waves. By incorporating this data, models can be updated to better reflect the virus’s potential for reinfection and its impact on transmission dynamics. This improved accuracy in prediction will lead to better-informed decisions regarding public health interventions. For example, understanding the reinfection rate of Omicron will help predict the severity and duration of future outbreaks.
This data, combined with historical trends, allows for more precise predictions of future outbreaks and the potential strain on healthcare resources. An example of this in action is the CDC’s use of epidemiological models to predict future trends in disease spread and to develop targeted prevention strategies.
Future Research Directions

Navigating the complexities of Omicron reinfection requires a proactive approach, focusing on crucial knowledge gaps. Understanding the factors influencing reinfection rates, the evolving immune response, and the potential long-term health consequences is paramount for effective public health strategies. This necessitates a robust research agenda.
Identifying Factors Influencing Reinfection
Current research has identified several potential factors influencing Omicron reinfection, such as pre-existing immunity levels, vaccine efficacy, and the specific Omicron variant lineage. Further investigation is crucial to unravel the intricate interplay of these factors. Understanding how individual characteristics, such as age, underlying health conditions, and lifestyle choices, contribute to reinfection risk is essential for targeted interventions.
Analyzing Immune Response Dynamics
The immune response to Omicron reinfection is a dynamic process. Determining the extent to which prior infection, vaccination, or a combination of both, influences the subsequent immune response to reinfection is crucial. Analyzing the specific antibodies generated during the initial infection and subsequent reinfection is essential to determine their neutralizing capacity. Furthermore, investigation into the role of T-cell responses in preventing or mitigating severe disease during reinfection is warranted.
Detailed analysis of immune responses, including B-cell and T-cell responses, over time, is needed to comprehend the effectiveness and duration of these responses in preventing reinfection.
Investigating Long-Term Health Outcomes
The long-term effects of Omicron reinfection remain largely unknown. Determining the prevalence of long COVID symptoms, including fatigue, cognitive impairment, and respiratory issues, after reinfection is critical. Investigating whether specific factors, such as the severity of the initial infection or the time elapsed between infections, correlate with the development of long COVID-like symptoms is necessary. Further research into the mechanisms underlying these potential long-term health consequences is essential.
Specific Research Questions and Methodologies
| Research Question | Study Type | Methodology |
|---|---|---|
| What is the relationship between pre-existing immunity levels (from prior infection or vaccination) and the risk of Omicron reinfection? | Cohort study | Follow a large cohort of individuals over time, tracking their exposure to Omicron and subsequent reinfection rates. Analyze pre-existing immunity levels through antibody testing and/or T-cell assays. |
| How does the specific Omicron variant lineage influence the immune response to reinfection? | Case-control study | Compare individuals infected with different Omicron lineages, analyzing their immune responses and clinical outcomes. Employ genomic sequencing to identify specific Omicron variants. |
| What is the duration and magnitude of neutralizing antibody responses following reinfection with Omicron? | Prospective cohort study | Follow individuals who have been reinfected with Omicron, collecting blood samples at regular intervals to measure antibody levels and neutralizing capacity. |
| What is the correlation between the severity of the initial Omicron infection and the development of long COVID-like symptoms after reinfection? | Longitudinal study | Track individuals who have experienced reinfection, collecting data on the severity of the initial infection and monitoring for long COVID symptoms over an extended period. |
Conclusion

In conclusion, while reinfection with Omicron is a possibility, the full picture is still developing. The available data offers valuable insights, but further research is crucial to fully grasp the complexities of reinfection, including how frequently it occurs, the severity of subsequent infections, and the efficacy of vaccines in preventing it. This understanding is vital for developing effective public health strategies and preparing for future viral outbreaks.