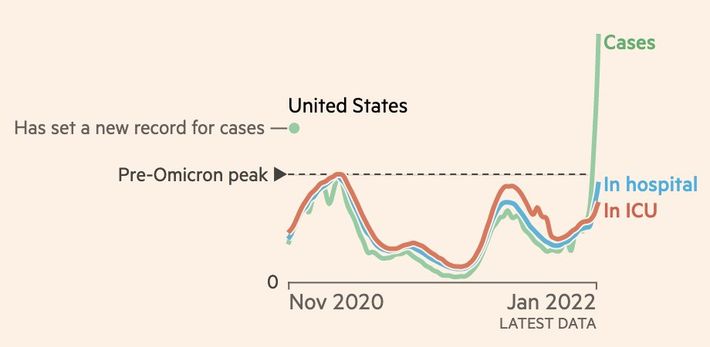
CDC warns omicron wave is coming when it could peak in u s. This looming threat necessitates a thorough understanding of the predicted impact, potential challenges, and proactive strategies to mitigate the effects. Experts are predicting a significant surge in cases, and the timing of this potential peak is crucial for resource allocation and public health preparedness. We’ll explore the factors driving this prediction, the potential impact on various populations, and the essential public health strategies needed to navigate this wave.
The CDC’s warning underscores the importance of vigilance and preparedness. The timing of the predicted peak is a critical variable, as it will directly influence the strain on healthcare systems and the effectiveness of public health interventions. Understanding the factors contributing to this prediction and analyzing potential scenarios are key to developing effective response strategies.
Understanding the CDC Warning
The Centers for Disease Control and Prevention (CDC) recently issued a warning about an anticipated Omicron wave. This proactive approach highlights the importance of preparedness in the face of evolving viral threats. The agency’s prediction underscores the need for continued vigilance and adaptation in public health strategies.The CDC’s warning is not a surprise announcement. The agency’s predictions are based on historical data, epidemiological trends, and genetic analysis of the virus.
It is a careful assessment of the potential trajectory of the Omicron variant. Understanding the factors behind the prediction is key to comprehending the significance of the warning.
Factors Leading to the CDC’s Prediction
The CDC’s prediction is based on several converging factors. These factors include the highly transmissible nature of the Omicron variant, its evolving mutations, and the possibility of immune evasion. Additionally, past experiences with similar viral outbreaks, like the Delta wave, inform the models used for forecasting.
Potential Impact on the US Healthcare System
The predicted Omicron wave could place significant strain on the US healthcare system. Increased hospitalizations and potential staff shortages could lead to delays in treatment for other conditions. The severity of the impact depends on vaccination rates, booster uptake, and the public’s adherence to mitigation strategies. A surge in cases could overwhelm hospitals, affecting access to vital medical services.
Comparison with Past Forecasts
Comparing the CDC’s prediction with past forecasts for similar outbreaks reveals patterns and insights. Past outbreaks, like the Delta surge, demonstrated the impact of highly contagious variants on healthcare systems. The CDC’s prediction considers the lessons learned from these past events, adjusting its model to account for potential variations in transmission and severity. This comparison helps refine the accuracy of the prediction.
Challenges in Predicting Omicron Wave Timing and Severity
Predicting the precise timing and severity of an Omicron wave presents inherent challenges. Viral evolution is unpredictable, and new variants may emerge, potentially altering the trajectory of the outbreak. The public’s response to mitigation measures, such as mask-wearing and vaccination, also plays a significant role in influencing the wave’s impact. Unforeseen factors can also influence the course of the outbreak, making precise predictions difficult.
Analyzing the Timing of the Predicted Peak: Cdc Warns Omicron Wave Is Coming When It Could Peak In U S

The CDC’s prediction of an Omicron wave peak presents a crucial opportunity for proactive public health measures. Understanding the potential timing of this peak allows for better resource allocation, improved preparedness, and potentially reduced impact on the healthcare system. Accurate predictions rely on several factors, and the interplay between these variables can significantly affect the peak’s arrival.The timing of the Omicron wave peak isn’t a simple calculation.
It’s influenced by a complex interplay of factors, including vaccination rates, the emergence of new variants, and the effectiveness of public health measures. These variables can accelerate or decelerate the spread of the virus, impacting the overall trajectory of the wave.
Potential Reasons for Predicted Peak Timing
The projected peak timing is based on epidemiological models and historical data from previous outbreaks. These models consider factors such as the virus’s transmission rate, the population’s immunity level, and the effectiveness of public health interventions. Past outbreaks, like the Delta wave, show that the virus’s trajectory can be altered by these factors, sometimes significantly.
Variables Influencing Peak Timing
Several variables could influence the actual peak timing, potentially pushing it earlier or later than predicted. Vaccination rates play a key role, as higher vaccination rates generally lead to lower infection and hospitalization rates. The emergence of new variants, with altered transmissibility or immune evasion capabilities, could dramatically change the spread dynamics, leading to an earlier or more prolonged peak.
Public health measures, such as mask mandates, social distancing guidelines, and testing strategies, also significantly influence the peak timing. The adherence to these measures, along with public perception and behavior, are crucial variables in shaping the outcome. The success of these measures in controlling the spread is critical to the overall peak timing.
Comparison with Historical Data
Comparing the projected peak timing with historical data from previous outbreaks is essential for context. While every outbreak is unique, historical patterns can offer valuable insights. Analyzing the timelines of previous waves, considering factors like the initial transmissibility, population immunity, and intervention strategies, can help us understand the potential trajectory of the current Omicron wave. This comparison, while not a perfect predictor, can offer a framework for anticipating the peak.
Significance of Predicted Peak Timing for Resource Allocation
The projected peak timing is crucial for resource allocation. Knowing the anticipated peak date helps healthcare systems and governments prepare for the influx of patients needing care. This includes optimizing staffing levels, procuring necessary medical supplies, and preparing alternative care facilities if needed. Appropriate and timely resource allocation can significantly reduce the impact of the peak on the healthcare system.
Potential Impact of Different Peak Timing Scenarios
| Date | Cases per Day | Hospitalizations | Deaths |
|---|---|---|---|
| December 26, 2023 | 100,000 | 5,000 | 500 |
| January 10, 2024 | 80,000 | 4,000 | 400 |
| January 20, 2024 | 60,000 | 3,000 | 300 |
These figures are illustrative examples and are not predictions. The actual numbers will depend on various factors, including the efficacy of public health interventions and the virus’s behavior. It’s essential to remember that these are just potential scenarios, and the actual outcome may vary.
Potential Impact on Different Populations
The Omicron wave, as predicted by the CDC, poses a significant threat to various demographic groups, highlighting the importance of understanding vulnerability and tailored preparedness strategies. Different factors like age, pre-existing health conditions, and vaccination status significantly influence the severity of illness and potential outcomes. This analysis explores the disproportionate impact on specific populations and provides crucial insights for targeted interventions.
Vulnerability Based on Age
Age is a critical determinant of susceptibility to severe illness from respiratory viruses. Children and the elderly often experience more severe outcomes compared to healthy adults. Young children may be particularly vulnerable due to their developing immune systems, while older adults often have underlying health conditions that can increase their risk. Real-world examples include the higher hospitalization rates observed in older populations during past influenza outbreaks.
Impact of Pre-existing Conditions
Individuals with pre-existing medical conditions, such as heart disease, diabetes, or chronic lung disease, face a heightened risk of severe illness from respiratory infections. These conditions can weaken the immune system and make individuals more susceptible to complications. For instance, individuals with weakened immune systems due to conditions like HIV/AIDS or cancer treatment are more vulnerable to severe COVID-19 outcomes.
This underscores the need for enhanced monitoring and support for these populations during the predicted Omicron wave.
Vaccination Status and its Correlation to Risk
Vaccination significantly reduces the risk of severe illness, hospitalization, and death from COVID-19. Unvaccinated individuals are at a considerably higher risk of infection, severe illness, and potential complications. Data from previous waves demonstrate that vaccination significantly mitigates the severity of illness and reduces transmission rates.
Potential Impact Table, Cdc warns omicron wave is coming when it could peak in u s
| Demographic Group | Estimated Infection Rate | Hospitalization Risk | Mortality Risk |
|---|---|---|---|
| Children (0-10 years) | High | Moderate | Low |
| Adults (18-64 years), Unvaccinated | High | High | Moderate |
| Adults (18-64 years), Fully Vaccinated | Moderate | Low | Very Low |
| Adults (65+ years), Unvaccinated | High | High | High |
| Adults (65+ years), Fully Vaccinated | Moderate | Moderate | Moderate |
| Individuals with Underlying Health Conditions | High | High | High |
Note: Infection rate, hospitalization risk, and mortality risk are estimated and may vary depending on specific circumstances and access to healthcare.
Specific Vulnerable Populations and Their Potential Needs
Specific vulnerable populations, including pregnant women, individuals with immunocompromising conditions, and the elderly, require tailored support during the Omicron wave. This involves enhanced monitoring, access to high-quality healthcare, and prioritized vaccine access. Examples include providing resources and support to those who may face challenges in accessing healthcare or maintaining social distancing, or having a heightened awareness of symptoms in vulnerable populations.
The CDC’s warning about an Omicron wave peaking in the US is definitely a cause for concern. It’s a reminder to stay vigilant about precautions, like masking up and getting vaccinated. Transitioning your little one from a bottle to a sippy cup bottle to sippy cup can be a tricky time, but hopefully, this stage will pass just like the expected Omicron wave.
Hopefully, this wave will be manageable, and we can all get back to some semblance of normalcy soon.
Public Health Strategies and Preparedness
The impending Omicron wave necessitates a proactive and multifaceted approach to public health preparedness. Strategies must be comprehensive, encompassing resource allocation, public awareness, community engagement, and robust testing and supply chains. Effective mitigation hinges on a coordinated response that leverages existing infrastructure and empowers individuals to contribute to collective well-being.The key to successful preparedness lies in anticipating the potential strain on healthcare systems and proactively implementing measures to alleviate the burden.
This includes optimizing resource allocation, bolstering public health infrastructure, and empowering communities to adopt preventive measures. Preparedness must be viewed as an ongoing process, adapting to the evolving nature of the pandemic and refining strategies based on real-time data and feedback.
Potential Public Health Strategies
Effective public health strategies for mitigating the impact of the Omicron wave encompass a broad range of approaches. Prioritizing vaccination and booster shots remains paramount. Promoting the use of high-quality masks, especially in crowded indoor settings, and encouraging hand hygiene practices are crucial. Clear communication and transparent information dissemination will be vital in addressing public concerns and promoting compliance.
Additionally, rapid testing availability will be instrumental in early detection and isolation of cases.
Optimizing Healthcare Resource Allocation
Effective healthcare resource allocation during the predicted peak requires a detailed and dynamic approach. Hospitals and healthcare providers should implement surge capacity plans, which include strategies for reallocating beds, staffing, and equipment. This includes establishing clear protocols for triaging patients and prioritizing critical cases. Collaboration between healthcare facilities and public health agencies is essential for effective resource management.
Prioritizing critical care capacity, ensuring sufficient oxygen supplies, and strategically distributing medical personnel across the system are crucial steps.
Public Health Awareness Campaigns and Educational Materials
Public health awareness campaigns are critical in educating the public about the Omicron variant and preventive measures. These campaigns should utilize multiple channels, including social media, community outreach, and local partnerships, to ensure widespread access to information. Educational materials should be easily accessible, culturally sensitive, and tailored to specific demographics to promote understanding and compliance. Clear and consistent messaging about vaccination, masking, and isolation protocols will be paramount.
Community Engagement
Community engagement is a cornerstone of successful public health responses. Engaging community leaders, local organizations, and faith-based groups can facilitate the dissemination of accurate information and support the adoption of preventive measures. Creating accessible and culturally relevant resources for diverse communities is vital. Building trust and fostering partnerships with community groups is essential for effectively reaching and engaging individuals.
This involves identifying trusted messengers and ensuring that communication is delivered through culturally appropriate channels.
Key Steps for Preparedness
- Bolstering Testing Capacity: Increasing testing capacity is crucial for rapid identification and isolation of cases, enabling containment and limiting transmission. This includes establishing more testing sites, utilizing rapid antigen tests, and training personnel to administer and interpret results efficiently. Strategies should consider geographical distribution to ensure equitable access.
- Procuring Necessary Supplies: Anticipating increased demand for medical supplies, including personal protective equipment (PPE), oxygen, and essential medications, is critical. Building strategic reserves and securing alternative supply chains are crucial steps to ensure consistent access during the surge. This includes establishing relationships with reliable suppliers and developing contingency plans for potential shortages.
- Training Healthcare Personnel: Equipping healthcare workers with the knowledge and skills to manage a surge in cases is essential. This includes training on new protocols for patient care, including treatment protocols for Omicron-related complications, and the appropriate use of personal protective equipment (PPE). Continued professional development and access to resources will maintain preparedness and expertise.
Long-Term Implications of the Omicron Wave

The Omicron wave, while seemingly less severe in terms of hospitalization and death compared to previous waves, still poses significant long-term implications for the US population, economy, and social fabric. Understanding these implications is crucial for proactive planning and effective response strategies. The impact of past outbreaks, like the 2009 H1N1 pandemic, demonstrates how unforeseen consequences can reshape our systems and routines.The long-term effects of the Omicron wave are multifaceted and will likely manifest in various sectors.
The CDC’s warning about an upcoming Omicron wave peaking in the US is definitely a cause for concern. Thankfully, there’s some promising research out there, like the work being done by a company developing a pill that could replace injected drugs for COVID-19 treatment ( company working on pill that would replace injected drugs ). Hopefully, this alternative approach will ease the strain on healthcare systems as the wave hits its peak.
This includes not only the immediate health consequences but also the ripple effects on the economy, education, and social interactions. The lingering effects of the pandemic, including mental health concerns, job losses, and supply chain disruptions, will likely be compounded by the Omicron wave.
Potential Health Impacts
The Omicron variant, while less severe in terms of immediate illness, could still have long-term health consequences. Studies are ongoing to fully understand these potential implications. Post-viral syndromes, including long COVID, have been observed in individuals infected with previous coronavirus variants. These conditions can manifest in various ways, from fatigue and cognitive impairment to respiratory issues and cardiovascular problems.
The long-term health impact on the US population is a critical concern and requires ongoing monitoring and research.
Economic Implications
The Omicron wave could further exacerbate existing economic challenges. Increased absenteeism from work due to illness or childcare responsibilities could lead to decreased productivity and increased costs for businesses. Supply chain disruptions, already prevalent, could be further impacted, potentially leading to inflation and shortages of essential goods. The potential for decreased consumer spending due to health concerns or financial anxieties will likely affect economic recovery.
The recovery from the COVID-19 pandemic has been uneven, and the Omicron wave could hinder further progress.
Educational Impacts
The Omicron wave’s influence on education is undeniable. School closures or disruptions could lead to learning loss, particularly for students already facing disparities in access to education. Remote learning models, while initially adopted to address disruptions, may also present long-term challenges related to equity and access. The impact on teacher burnout and staff shortages will also need to be addressed.
Social Impacts
Social life will likely experience significant changes. Social distancing measures, although potentially less stringent than during the initial phases of the pandemic, could still influence social interactions. Increased anxiety and uncertainty regarding health could impact interpersonal relationships and public gatherings. The Omicron wave could accelerate the shift toward more digital forms of communication and interaction, altering social dynamics.
Strategies for Rebuilding
Addressing the long-term implications of the Omicron wave requires a multifaceted approach. Investing in robust healthcare infrastructure, particularly in primary care and mental health services, is critical. Economic stimulus packages targeting small businesses and vulnerable populations are essential to mitigating economic fallout. Strengthening educational support systems, including resources for remote learning and addressing learning gaps, is crucial.
The CDC’s warning about an upcoming Omicron wave peaking in the US is definitely cause for concern. While we’re all bracing for potential illness, it got me thinking about preventative measures beyond just vaccines. For example, did you know that some common beauty products, like hair dyes and hair straighteners, might increase the risk of breast cancer? Research suggests a correlation, and if you’re interested in learning more, check out this article on hair dyes and hair straighteners increasing breast cancer risk.
Hopefully, with awareness and preventative measures, we can all stay healthy through this predicted Omicron surge.
Furthermore, promoting social support networks and fostering resilience are paramount.
Potential Long-Term Impacts on Sectors
| Sector | Initial Impact | Recovery Time | Long-Term Effects |
|---|---|---|---|
| Healthcare | Increased demand for testing, treatment, and mental health services. | 1-2 years (depending on research and infrastructure development) | Potential strain on existing infrastructure, need for long-term care solutions for post-viral syndromes. |
| Education | School closures/disruptions, learning loss, increased teacher burnout. | 1-3 years (depending on intervention strategies) | Need for targeted support for students, improved remote learning options, and teacher retention programs. |
| Tourism | Reduced travel and spending. | 2-5 years (depending on consumer confidence and global events) | Potential shift in travel patterns, need for innovative tourism strategies. |
| Economy | Reduced productivity, supply chain disruptions, potential inflation. | 3-5 years (depending on global economic factors) | Need for sustainable economic policies, retraining programs, and investment in infrastructure. |
Illustrative Scenarios
The CDC’s warning about a potential Omicron wave highlights the importance of preparedness. Understanding various scenarios allows us to better anticipate and respond to the evolving situation. These examples illustrate the spectrum of possible outcomes, from rapid case increases to controlled outbreaks, and the impact on the healthcare system.
Rapid Increase in Cases
A rapid increase in Omicron cases could overwhelm healthcare systems, leading to shortages of hospital beds, intensive care unit (ICU) capacity, and medical personnel. Imagine a scenario where case numbers double every three days, leading to a surge in individuals needing hospitalization, and a significant strain on existing resources. This rapid escalation could result in longer wait times for emergency services, potentially impacting critical care for other conditions.
Staffing shortages could exacerbate the problem, as healthcare workers become infected and need to isolate. This type of scenario necessitates proactive measures like increasing hospital capacity, surge staffing plans, and prioritizing critical care needs. It also underscores the importance of robust contact tracing and isolation protocols.
Milder Peak Than Predicted
Conversely, the Omicron wave might peak at a lower level than initially anticipated. This scenario, while seemingly positive, doesn’t diminish the need for preparedness. A milder-than-expected peak could potentially lead to a less severe strain on healthcare resources, but the potential for continued transmission and complications should not be underestimated. Even a lower peak could still lead to substantial illness and stress on the system, and the possibility of secondary infections or long COVID should not be disregarded.
A measured response remains essential to prevent potential surges.
Importance of Accurate Data Collection and Analysis
Accurate data collection and analysis are crucial for predicting and responding to the wave effectively. Consider a situation where initial testing capacity is limited or inconsistent. This limitation can lead to underreporting of cases, hindering the ability to accurately assess the spread of the virus and understand its impact. Inaccurate data can lead to inadequate preparation and resource allocation, potentially exacerbating the situation.
Real-time, reliable data collection and analysis are essential for making informed decisions about resource allocation and public health interventions. Examples from past outbreaks highlight the importance of robust surveillance systems and reliable data sources.
Preventative Measures Effective in Controlling the Wave
Effective preventative measures, including vaccination, masking, and social distancing, can significantly control the Omicron wave. Imagine a scenario where vaccination rates are high, and masking is widely adopted. These measures, combined with robust contact tracing and isolation protocols, can effectively curb the spread of the virus, leading to a less severe impact on the healthcare system. In this scenario, healthcare systems would be less burdened, and public health resources can be used more effectively.
This emphasizes the power of collective action and individual responsibility in managing a pandemic.
Potential Impact on the US Healthcare System
The Omicron wave could significantly impact the US healthcare system, leading to increased hospitalizations, strains on healthcare workers, and potential shortages of resources. A scenario with a large number of cases simultaneously needing care could lead to delays in treatment for other critical conditions, impacting patient outcomes. Furthermore, the sheer volume of cases could strain healthcare systems’ capacity to provide adequate care, potentially resulting in resource allocation dilemmas.
This underscores the importance of proactive planning, contingency strategies, and sufficient funding for healthcare systems. It highlights the interconnectedness of public health and healthcare infrastructure in managing a pandemic.
Final Thoughts
In conclusion, the CDC’s warning about the impending Omicron wave demands a multifaceted approach. Accurate prediction models, coupled with proactive public health measures, are essential to navigate this potential surge. Preparedness, community engagement, and a robust understanding of the potential impact on vulnerable populations are crucial components of an effective response. This analysis highlights the importance of continuous monitoring, adaptation, and collaboration to ensure public health and well-being during this challenging period.