Changing healthcare industry makes hospitals obsolete. The traditional hospital model, a cornerstone of healthcare for decades, is facing unprecedented pressure from a rapidly evolving landscape. Technological advancements, shifting patient expectations, and financial pressures are all converging to reshape the delivery of care, potentially rendering traditional hospital settings obsolete. This article delves into the factors driving this transformation and explores the rise of alternative healthcare models.
The changing healthcare industry is characterized by a move away from the traditional hospital model. This shift is being fueled by several interconnected factors, including technological innovations that enable remote patient monitoring and telemedicine, increasing patient demands for convenience and accessibility, and evolving financial realities impacting hospital profitability. This evolution is compelling hospitals to adapt and explore alternative care models to stay relevant.
Defining Obsolescence in Healthcare
The healthcare industry is undergoing a rapid transformation, with technology and patient preferences driving fundamental shifts in how care is delivered. This evolution is challenging the traditional hospital model, leading to a perception of obsolescence for some facilities. This discussion delves into the meaning of obsolescence in this context, comparing traditional hospital models with emerging systems, and examining the factors driving this perceived change.Traditional hospital models, built around inpatient care and a centralized structure, are facing increasing pressure to adapt.
Emerging healthcare delivery systems, encompassing telehealth, virtual care, and community-based clinics, offer alternative approaches to patient care, often more convenient and cost-effective.
The changing healthcare landscape is making traditional hospitals feel a bit outdated. Imagine a future where personalized care is the norm, and virtual consultations are as common as sweet potato toast recipes. Finding innovative ways to deliver healthcare, like focusing on preventative care and telehealth, will be crucial for hospitals to stay relevant. And while we’re on the topic, have you tried any of the delicious sweet potato toast recipes out there?
This evolution of the healthcare industry will inevitably render some hospitals obsolete, a stark reality in the face of new technologies and approaches.
Defining Hospital Obsolescence
Obsolescence in the context of hospitals refers to the diminished relevance and effectiveness of traditional hospital models in meeting the evolving needs of patients and the healthcare system. This decline is not necessarily about the physical building becoming outdated, but rather about the underlying operational model losing its competitive edge. The shift toward patient-centered care, accessibility, and cost-effectiveness creates a paradigm shift, leading to a re-evaluation of the hospital’s role.
Comparison of Traditional and Emerging Healthcare Delivery Systems
Traditional hospital models typically focus on inpatient care, requiring patients to visit the facility for procedures and extended stays. Emerging systems prioritize outpatient services, telehealth consultations, and preventative care, allowing patients to access care more easily and efficiently from their homes or local community centers.
- Traditional hospitals often have high overhead costs due to extensive facilities and staffing needs for inpatient care. Conversely, emerging systems frequently leverage virtual platforms and remote monitoring, leading to potentially lower costs and improved accessibility.
- Inpatient care, while vital, is not always the most effective or cost-efficient approach for all conditions. Emerging models can offer alternative, less intrusive care options, reducing costs and improving patient satisfaction.
- Traditional models often struggle with access issues, particularly for patients in rural areas or with limited mobility. Emerging systems address these challenges by providing convenient telehealth options and community-based clinics, improving accessibility.
Factors Contributing to Perceived Hospital Obsolescence
Several factors contribute to the perception of hospital obsolescence:
- Rising Costs: Traditional hospital models often face escalating costs due to high staffing needs, advanced medical equipment, and extensive facility maintenance. This pressure to maintain high levels of service, coupled with limited reimbursement models, leads to financial strain.
- Technological Advancements: Telemedicine, remote monitoring, and digital health platforms offer alternative, more efficient approaches to diagnosis, treatment, and ongoing patient management. This creates a compelling alternative to traditional, facility-based care.
- Changing Patient Expectations: Patients increasingly expect convenient, accessible, and personalized healthcare experiences. The rise of patient portals and online scheduling highlights a preference for self-service and remote interactions, potentially diminishing the need for traditional hospital visits.
Technology and Digital Health in Healthcare Transformation
Technological advancements are transforming healthcare delivery, empowering patients and providers alike. Digital health tools are playing a pivotal role in enabling remote monitoring, virtual consultations, and personalized treatment plans.
- Telemedicine allows healthcare providers to connect with patients remotely, offering consultations, diagnoses, and follow-up care. This reduces the need for in-person visits, particularly for routine checkups and non-emergency situations.
- Remote patient monitoring systems provide continuous data collection on vital signs and other health indicators, enabling proactive intervention and early detection of potential issues. This empowers patients to actively manage their health and reduces the reliance on periodic hospital visits.
- Digital health platforms offer personalized treatment plans, medication reminders, and access to health information. This empowers patients to take an active role in their care, promoting self-management and improving health outcomes.
Disruption of Traditional Hospital Operations
The changing healthcare industry is disrupting traditional hospital operations in various ways. The emphasis on preventative care, outpatient services, and remote monitoring is altering the focus of hospitals from solely providing inpatient care to a more comprehensive and integrated approach.
- Shifting Revenue Streams: The rise of telehealth and virtual care is impacting traditional hospital revenue streams, which are increasingly tied to inpatient procedures. Hospitals must adapt by diversifying revenue sources to include virtual services, community clinics, and other related initiatives.
- Redefining Service Models: Hospitals are facing pressure to adapt their service models to incorporate telehealth, virtual consultations, and community-based care. This requires investment in technology and training for staff to effectively utilize these new tools and approaches.
- Staffing Changes: The transition to a more integrated and remote care model requires a shift in the skills and training of hospital staff. Healthcare professionals need to adapt to new technologies and adopt a more comprehensive approach to patient care.
Healthcare Industry Transformations Impacting Hospitals
| Transformation | Impact on Hospitals |
|---|---|
| Rise of Telemedicine | Reduced need for in-person visits, increased virtual consultations, potential for decreased inpatient admissions |
| Emphasis on Preventative Care | Focus on wellness programs, community health initiatives, reduced reliance on reactive care |
| Remote Patient Monitoring | Continuous data collection, proactive intervention, improved patient engagement, potential for reduced hospital readmissions |
| Increased Patient Access to Information | Empowered patients, more informed decision-making, greater demand for personalized care |
Impact of Technological Advancements

The healthcare industry is undergoing a rapid transformation, driven largely by technological advancements. These innovations are reshaping the traditional hospital model, impacting everything from patient care to resource allocation. The rise of telemedicine, remote monitoring, and artificial intelligence is challenging the very definition of “hospital” and suggesting a future where the need for extensive in-patient stays may diminish.
Telemedicine and Remote Patient Monitoring
Telemedicine and remote patient monitoring are significantly altering the roles of hospitals. These technologies allow for virtual consultations, remote monitoring of vital signs, and the delivery of healthcare services outside the confines of a physical hospital. This shift allows for earlier intervention and management of chronic conditions, reducing the need for unnecessary hospital admissions. Hospitals are adapting to this new reality by re-evaluating their infrastructure and services, becoming more focused on specialized care and coordination with remote monitoring systems.
Technological Innovations Diminishing the Need for Traditional Hospital Stays
Several technological innovations are reducing the dependence on traditional hospital stays. Examples include at-home blood glucose monitoring systems for diabetics, wearable devices tracking vital signs, and remote monitoring systems for patients with chronic conditions. These advancements enable proactive management of health issues, preventing complications that might otherwise require hospitalization. Early detection and intervention through these technologies allow for more effective management of conditions, leading to fewer hospitalizations and better health outcomes.
AI and Machine Learning in Healthcare
Artificial intelligence (AI) and machine learning (ML) are revolutionizing healthcare in numerous ways. AI-powered diagnostic tools can analyze medical images, identify patterns, and assist in faster and more accurate diagnoses. Machine learning algorithms can predict patient risk factors and tailor treatment plans, enabling proactive interventions. This leads to improved accuracy in diagnoses, personalized treatment plans, and more efficient hospital workflows.
For instance, AI-driven systems can analyze patient data to identify high-risk individuals, enabling early intervention and potentially preventing hospital readmissions.
Wearable Technology’s Impact on Healthcare Delivery
Wearable technology is changing the landscape of healthcare delivery. Smartwatches and fitness trackers monitor vital signs, activity levels, and sleep patterns. This continuous data collection allows for early detection of potential health issues, enabling timely interventions. Hospitals are increasingly integrating data from wearable devices into patient records, providing a comprehensive view of patients’ health status and facilitating more proactive care.
This data can help predict potential problems and allow for preemptive actions to avoid hospitalizations.
The changing healthcare landscape is rapidly making some hospitals feel obsolete. Advances in home healthcare and telemedicine are changing how we access care, and frankly, some hospitals are struggling to keep up. It’s interesting to see how this trend mirrors personal struggles like Ann Hathaway’s recent pregnancy announcement, after experiencing fertility challenges ann hathaway reveals pregnancy after fertility struggles.
While this is a very personal journey, it highlights a broader shift in how we approach healthcare, potentially diminishing the need for certain types of hospitals in the future.
Data Analytics and Hospital Efficiency
Data analytics is playing a crucial role in optimizing hospital efficiency and resource allocation. By analyzing vast amounts of patient data, hospitals can identify patterns, predict demand, and optimize staffing levels. This leads to more efficient use of resources, improved patient flow, and reduced costs. Data analytics can help hospitals identify areas where resources are over-utilized or under-utilized, optimizing bed allocation, and streamlining workflows.
Table: Technological Advancements Impacting the Hospital Model
| Technological Advancement | Impact on Hospital Model |
|---|---|
| Telemedicine | Reduces need for in-person visits, expands access to care, allows for remote monitoring. |
| Remote Patient Monitoring | Enables continuous health monitoring, facilitates proactive interventions, reduces hospital readmissions. |
| AI/Machine Learning | Improves diagnostic accuracy, personalizes treatment plans, optimizes resource allocation. |
| Wearable Technology | Provides continuous health data, allows for early detection of issues, enhances proactive care. |
| Data Analytics | Optimizes resource allocation, predicts demand, improves patient flow, reduces costs. |
Shifting Patient Expectations
The healthcare landscape is undergoing a dramatic transformation, driven not only by technological advancements but also by evolving patient expectations. Patients are increasingly demanding a more personalized, convenient, and accessible healthcare experience, which is fundamentally reshaping the traditional hospital model. This shift necessitates a deep understanding of these expectations and a proactive adaptation by healthcare providers to meet these evolving needs.Modern patients are less tolerant of lengthy wait times and complex bureaucratic processes.
Convenience and accessibility are paramount, influencing their choices of healthcare providers and impacting hospital utilization rates. This changing dynamic is forcing hospitals to rethink their infrastructure, service delivery models, and overall approach to patient care.
Patient Preferences for Convenience and Accessibility
Patients are prioritizing convenient access to healthcare services. This includes readily available appointments, virtual consultations, and online tools for managing their health information. Remote monitoring technologies and telehealth platforms are increasingly important in facilitating this accessibility. The rise of on-demand healthcare services underscores the patient’s desire for prompt and easily accessible care. For example, many individuals now expect to be able to schedule appointments and access their medical records online through user-friendly portals, minimizing the need for in-person visits to the hospital.
Impact of Patient Engagement and Empowerment
Patient engagement and empowerment are driving significant changes in the traditional hospital structure. Patients are actively involved in their own healthcare decisions, seeking information and participating in their care planning. This shift emphasizes shared decision-making and empowers patients to take a more proactive role in managing their health. The use of patient portals and online platforms has enabled patients to communicate with their healthcare providers more efficiently and access information readily, further strengthening this dynamic.
Increasing Importance of Preventative Care
The focus on preventative care is growing, driven by patients’ desire to proactively manage their health and reduce the risk of chronic illnesses. This trend is impacting hospital utilization, as patients seek preventative screenings, vaccinations, and lifestyle counseling to maintain well-being. Hospitals are adapting by offering preventative care services, such as health workshops and wellness programs, alongside their traditional services.
Evolving Role of Patient Portals and Online Healthcare Platforms
Patient portals and online healthcare platforms are becoming integral components of the modern healthcare experience. These tools provide patients with secure access to their medical records, appointment scheduling, communication with providers, and access to educational resources. These platforms are not only improving patient convenience but also facilitating greater transparency and control over their health information.
Patient Expectations Influencing Healthcare Transformation
- Convenience and ease of access: Patients expect quick appointment scheduling, online access to records, and multiple communication channels.
- Personalized care: Patients desire tailored treatment plans and individualized attention to their specific needs and preferences.
- Transparency and control: Patients expect clear explanations of their conditions, treatment options, and access to their medical records.
- Proactive health management: Patients are seeking tools and resources to actively participate in managing their health and preventing illness.
- Cost-effectiveness: Patients are increasingly aware of healthcare costs and want transparent pricing and value-based care options.
The evolving preferences of patients are demanding a shift in how hospitals operate. These expectations emphasize the importance of proactive engagement, accessible technology, and a focus on preventative care.
Comparison of Traditional Hospital Experience and Modern Patient Expectations
| Aspect | Traditional Hospital Experience | Modern Patient Expectations |
|---|---|---|
| Accessibility | Limited appointment hours, in-person visits required | 24/7 access, virtual consultations, online scheduling |
| Communication | Limited communication channels, often delayed updates | Multiple communication channels, real-time updates, easy access to information |
| Engagement | Limited patient involvement in care decisions | Active participation in care decisions, shared decision-making |
| Convenience | Complex processes, lengthy wait times | Simple processes, fast and efficient service |
| Technology | Limited use of technology in patient interactions | Extensive use of technology for appointment scheduling, communication, and information access |
The traditional hospital experience often falls short of these modern expectations. This necessitates hospitals to adapt and embrace new technologies and models to better serve the needs of today’s patients.
Financial and Economic Pressures

The healthcare industry is facing unprecedented financial pressures, pushing hospitals to the brink of obsolescence. Rising costs, changing reimbursement models, and patient expectations are creating a complex and challenging landscape. Hospitals, once viewed as pillars of community health, are now grappling with the need to adapt or risk being left behind. The traditional model of hospital care, while valuable, is proving increasingly unsustainable in the face of these economic realities.Hospitals are struggling to maintain profitability in a system where costs are constantly rising, while reimbursement rates often lag behind.
This creates a vicious cycle, making it difficult for hospitals to invest in necessary upgrades, new technologies, and improved patient care. Alternative models, offering more streamlined and efficient care, are emerging as potentially more viable solutions. Understanding these financial pressures is crucial to appreciating the potential for hospitals to adapt and thrive, or to transform into something new altogether.
Rising Costs of Healthcare and Impact on Hospital Profitability
The escalating costs of medical technology, pharmaceuticals, and personnel are significant contributors to the financial strain on hospitals. Increased demand for specialized procedures and complex treatments, coupled with the rising cost of labor, further exacerbates the issue. This pressure manifests as reduced operating margins, hindering the ability of hospitals to reinvest in infrastructure, equipment, and staff training. The impact on profitability can be substantial, often leading to a decline in net income and a decreased ability to provide quality care.
Comparison Between Traditional Hospital Care and Alternative Models
Traditional hospital care often involves high overhead costs, including large physical spaces, extensive equipment, and a complex administrative structure. Alternative models, such as outpatient clinics, urgent care centers, and telehealth platforms, tend to have lower overhead costs. Telehealth, for example, allows for remote consultations, reducing the need for expensive in-person visits and hospital infrastructure. These alternative models often prioritize efficiency and cost-effectiveness, enabling them to offer competitive pricing and potentially higher profit margins.
The difference in cost structures between traditional and alternative models is a critical factor in understanding the changing healthcare landscape.
Impact of Insurance Regulations and Reimbursement Models on Hospital Sustainability
Insurance regulations and reimbursement models significantly influence hospital sustainability. Complex insurance claim processes and fluctuating reimbursement rates can make it difficult for hospitals to predict their financial future. Changes in insurance policies, including increased emphasis on value-based care, often lead to reduced reimbursements for procedures and services. These factors can negatively impact hospital cash flow and long-term financial health.
This illustrates the vulnerability of the traditional hospital model in a changing regulatory environment.
Role of Value-Based Care Models in Affecting Hospital Revenue Streams
Value-based care models, which incentivize hospitals to focus on preventative care and improved patient outcomes, are altering revenue streams. These models often reward hospitals for delivering high-quality care at a lower cost. Hospitals are being pressured to adopt value-based care models to ensure long-term financial sustainability. However, successful implementation of these models requires significant changes in hospital operations and a shift in mindset.
Need for Hospitals to Adapt to Changing Financial Pressures
Hospitals need to adapt to these changing financial pressures by embracing innovation and efficiency. This involves exploring new service models, investing in technology, and streamlining operations. Diversifying revenue streams by offering services beyond traditional inpatient care, such as outpatient services or preventative care, is crucial. These changes are essential for long-term survival in the increasingly competitive healthcare landscape.
Financial Pressures Comparison Table, Changing healthcare industry makes hospitals obsolete
| Factor | Traditional Hospital Care | Alternative Models (e.g., Outpatient Clinics, Telehealth) |
|---|---|---|
| Overhead Costs | High (large facilities, complex equipment, extensive administrative staff) | Low (smaller facilities, less complex equipment, streamlined processes) |
| Reimbursement Models | Historically fee-for-service, now facing pressure from value-based care | Potential for more predictable and potentially higher reimbursement rates through value-based care models |
| Staffing Costs | High (specialized staff, large support teams) | Potential for lower staffing costs due to less specialized roles, or specialized but not requiring large numbers of staff |
| Profitability | Historically high, but facing increasing pressure due to rising costs and changing reimbursement models | Potential for higher profitability through efficiency and cost-effectiveness |
| Adaptability | Can be slower to adapt due to large infrastructure and established processes | More agile and adaptable to changing market demands |
Alternative Healthcare Models: Changing Healthcare Industry Makes Hospitals Obsolete
The healthcare landscape is undergoing a seismic shift, with traditional hospital models facing increasing pressure. Alternative care settings are emerging as viable options, offering patients greater accessibility and choice. These models are responding to evolving patient preferences, technological advancements, and economic realities, reshaping how healthcare is delivered.
Outpatient Surgery Centers
Outpatient surgery centers have experienced significant growth, providing a more convenient and often less expensive alternative to inpatient procedures. This shift reflects a preference for shorter hospital stays and a focus on quicker recovery times. The impact on hospital operations is considerable, as hospitals must adapt to the competition and potentially re-allocate resources to maintain their market share.
The changing healthcare landscape is making traditional hospitals feel a bit outdated. With advancements in telehealth and at-home care, some argue that the need for large, brick-and-mortar hospitals is diminishing. This shift in healthcare delivery raises interesting questions, like whether or not pregnant women should be held accountable for their choices during pregnancy. For instance, should pregnant women be jailed for drinking?
This complex issue highlights the ethical and societal implications of evolving healthcare standards. Ultimately, the changing healthcare industry, while pushing hospitals towards adaptation, is also prompting important societal debates.
Many hospitals are now investing in or partnering with outpatient surgery centers to offer a wider range of services and cater to this growing demand.
Virtual Care
Virtual care, encompassing telehealth platforms and remote monitoring technologies, is rapidly transforming the healthcare industry. Virtual consultations, remote patient monitoring, and online appointment scheduling are becoming increasingly commonplace. This model is particularly valuable for patients in geographically remote areas, improving access to specialists and routine care. The integration of virtual care into existing hospital systems is crucial for maintaining patient engagement and reducing wait times.
Urgent Care Clinics
Urgent care clinics provide a vital service, addressing immediate health concerns that don’t require hospitalization. Their growth is closely linked to the increasing demand for convenient and timely access to care. Urgent care clinics often act as a buffer for hospital emergency rooms, reducing overcrowding and improving wait times for serious conditions. The relationship between urgent care clinics and hospital services is symbiotic, as they complement each other by managing different levels of patient need.
Concierge Medicine
Concierge medicine, a subscription-based model, provides patients with enhanced access to their primary care physician. This model often involves a monthly fee in exchange for prioritized appointments, extended office hours, and more personalized care. While concierge medicine is not a replacement for traditional hospital care, it is an alternative that appeals to individuals seeking a more tailored and accessible experience.
The impact on hospital usage is less direct but can lead to fewer emergency room visits if patients feel adequately supported by their concierge physicians.
Innovative Healthcare Models
Several innovative healthcare models are emerging as viable alternatives to traditional hospitals. These models include community health centers, which focus on preventative care and addressing health disparities, and integrated care networks, which bring together different healthcare providers under a unified system. The emergence of these models demonstrates a broader shift toward a more integrated and community-oriented approach to healthcare delivery.
Examples include mobile clinics, telehealth platforms tailored to specific populations, and care coordination systems that leverage technology to connect patients with the right resources.
Comparison of Traditional Hospitals and Alternative Healthcare Models
| Feature | Traditional Hospitals | Outpatient Surgery Centers | Virtual Care | Urgent Care Clinics | Concierge Medicine |
|---|---|---|---|---|---|
| Location | Typically centralized, often in urban areas | Often located in suburban or convenient areas | Can be delivered anywhere with internet access | Located in accessible locations for immediate care | Primarily focused on patient’s location |
| Patient Volume | High volume, diverse patient population | Lower volume, specialized procedures | Potentially high volume, depending on the platform | Moderate volume, immediate care needs | Lower volume, focused on specific patient base |
| Cost | Generally higher due to infrastructure and staffing | Often lower than inpatient procedures | Potentially lower due to reduced overhead | Lower than emergency rooms for non-emergencies | Higher initial cost, but potential for lower long-term costs |
| Accessibility | Can be challenging, depending on location and availability | Generally more accessible than hospitals | Extremely accessible, anytime, anywhere | Accessible for urgent needs | High accessibility through scheduled appointments |
| Focus | Comprehensive care, acute and chronic conditions | Specific procedures and surgeries | Remote diagnosis and treatment | Diagnosis and treatment of immediate needs | Personalized care and preventative health |
Societal and Cultural Shifts
The healthcare landscape is undergoing a profound transformation, driven not only by technological advancements but also by significant societal and cultural shifts. These shifts are reshaping the way healthcare is delivered, prompting a re-evaluation of traditional hospital models and emphasizing the importance of community-based approaches and preventative care. Understanding these evolving trends is crucial for navigating the future of healthcare.
Impact of Aging Populations on Hospital Demands
The global population is aging at an unprecedented rate. This demographic shift directly impacts hospital demands. Older adults often require more frequent and complex medical interventions, leading to increased utilization of hospital services. Chronic conditions like diabetes, heart disease, and arthritis are more prevalent in older populations, demanding specialized care and potentially longer hospital stays. This trend underscores the need for alternative care models that cater to the unique needs of an aging population, such as geriatric care facilities and home healthcare services.
Growing Awareness of Preventative Health
A growing awareness of preventative health is altering the role of hospitals. Patients are increasingly prioritizing wellness and proactive measures to maintain good health. This trend is reflected in the rise of preventative health programs and initiatives. Individuals are more actively engaged in managing their health through lifestyle choices, such as diet and exercise, and are seeking early screenings and preventative measures.
As a result, hospital visits for acute illnesses may decrease, while demand for wellness centers and preventative care clinics may increase.
Importance of Community Health Initiatives
Community health initiatives play a vital role in the evolving healthcare landscape. These initiatives focus on addressing health disparities within specific communities, promoting healthy lifestyles, and increasing access to preventative care. Examples include community health workers, mobile health clinics, and public health campaigns that focus on addressing specific health issues prevalent in the community. Community-based care reduces reliance on hospitals, particularly for non-emergency situations, and improves overall health outcomes for the population.
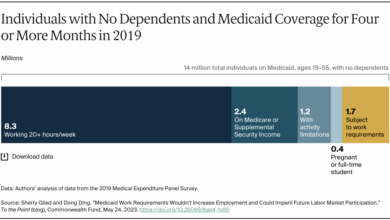
Influence of Health Disparities and Access to Care
Health disparities and inequities in access to care are significant factors influencing healthcare delivery. These disparities can be attributed to socioeconomic status, race, ethnicity, and geographic location. Individuals with limited access to healthcare often face higher rates of chronic diseases and poorer health outcomes. To address these disparities, healthcare systems must implement strategies to increase access and affordability of care, including targeted outreach programs, culturally sensitive services, and improved transportation options.
Growing Need for Healthcare Accessibility and Affordability
The need for accessible and affordable healthcare is paramount. Many individuals and families face significant financial barriers to accessing necessary medical care. This issue necessitates innovative solutions, such as expanding insurance coverage, implementing financial assistance programs, and exploring alternative payment models. Increasing accessibility and affordability fosters a healthier and more equitable society, leading to improved health outcomes and reduced reliance on hospital-based care.
Societal Shifts Influencing Healthcare Delivery
| Societal Shift | Impact on Healthcare Delivery |
|---|---|
| Aging Population | Increased demand for specialized care, longer hospital stays, and alternative care models |
| Growing Preventative Health Awareness | Decreased hospital visits for acute illnesses, increased demand for wellness centers and preventative care |
| Importance of Community Health Initiatives | Reduced reliance on hospitals for non-emergency situations, improved health outcomes |
| Health Disparities and Access to Care | Need for targeted outreach programs, culturally sensitive services, and improved transportation options |
| Healthcare Accessibility and Affordability | Need for innovative solutions like expanding insurance coverage, financial assistance programs, and alternative payment models |
Final Review
In conclusion, the changing healthcare industry is undeniably transforming the landscape. While hospitals remain vital components of the system, their traditional roles are being redefined and challenged. The emergence of alternative models, driven by technology, patient preferences, and financial realities, is creating a dynamic and multifaceted healthcare ecosystem. Hospitals must adapt to thrive in this new environment, embracing innovation and finding ways to integrate into the evolving landscape to ensure continued relevance and patient-centered care.