Christian health cost sharing programs growing in wake of obamacare are gaining significant traction. These programs, rooted in faith-based principles, offer an alternative to traditional insurance models, and their rise since the Affordable Care Act has sparked considerable interest. They provide a unique approach to healthcare affordability and access, drawing participants for various reasons. Understanding the mechanics, motivations, and potential impact of these programs is crucial for navigating the evolving healthcare landscape.
This article explores the history, financial structures, community aspects, legal considerations, and future projections of Christian health cost-sharing programs. It delves into the core principles, highlighting how these programs differ from traditional insurance plans. We’ll examine the reasons behind their growth, analyze the financial implications for participants, and discuss the potential impact on healthcare access and affordability.
Introduction to Christian Health Cost Sharing Programs
Christian health cost-sharing programs are gaining popularity as an alternative to traditional health insurance, particularly in the wake of the Affordable Care Act (ACA). These programs are based on shared responsibility and community support, often rooted in Christian values of mutual aid and caring for the vulnerable. Participants typically contribute to a fund from which members access healthcare expenses.
These programs offer a unique approach to healthcare access, often appealing to individuals and families seeking an alternative to the complexities and costs of conventional insurance.These programs are driven by a desire for a more holistic and faith-based approach to healthcare. The core motivation stems from a belief that healthcare should be accessible and affordable while aligning with Christian principles.
This often involves a commitment to sharing resources and supporting one another in times of need. This approach contrasts with the profit-driven model of traditional insurance.Christian health cost-sharing programs differ significantly from traditional insurance models. Traditional insurance plans typically involve premiums paid to an insurance company, which then covers a portion of medical expenses. In contrast, cost-sharing programs often involve contributions to a shared fund, which members use to offset healthcare costs.
The focus shifts from individual financial responsibility to communal support, reflecting the core principles of these programs.
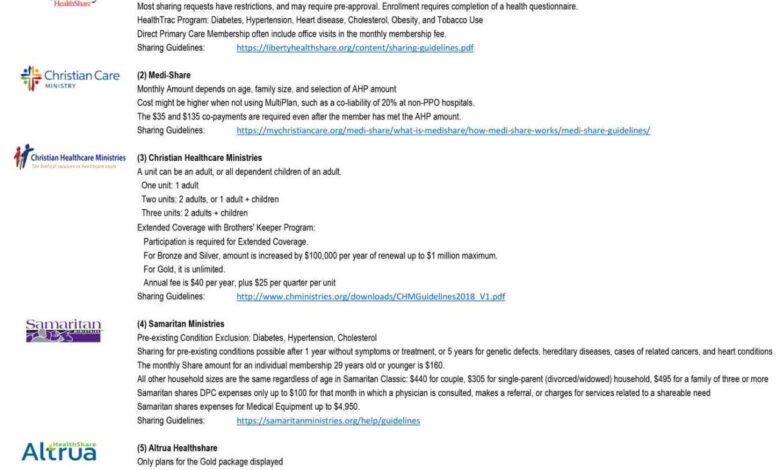
Comparison of Program Types
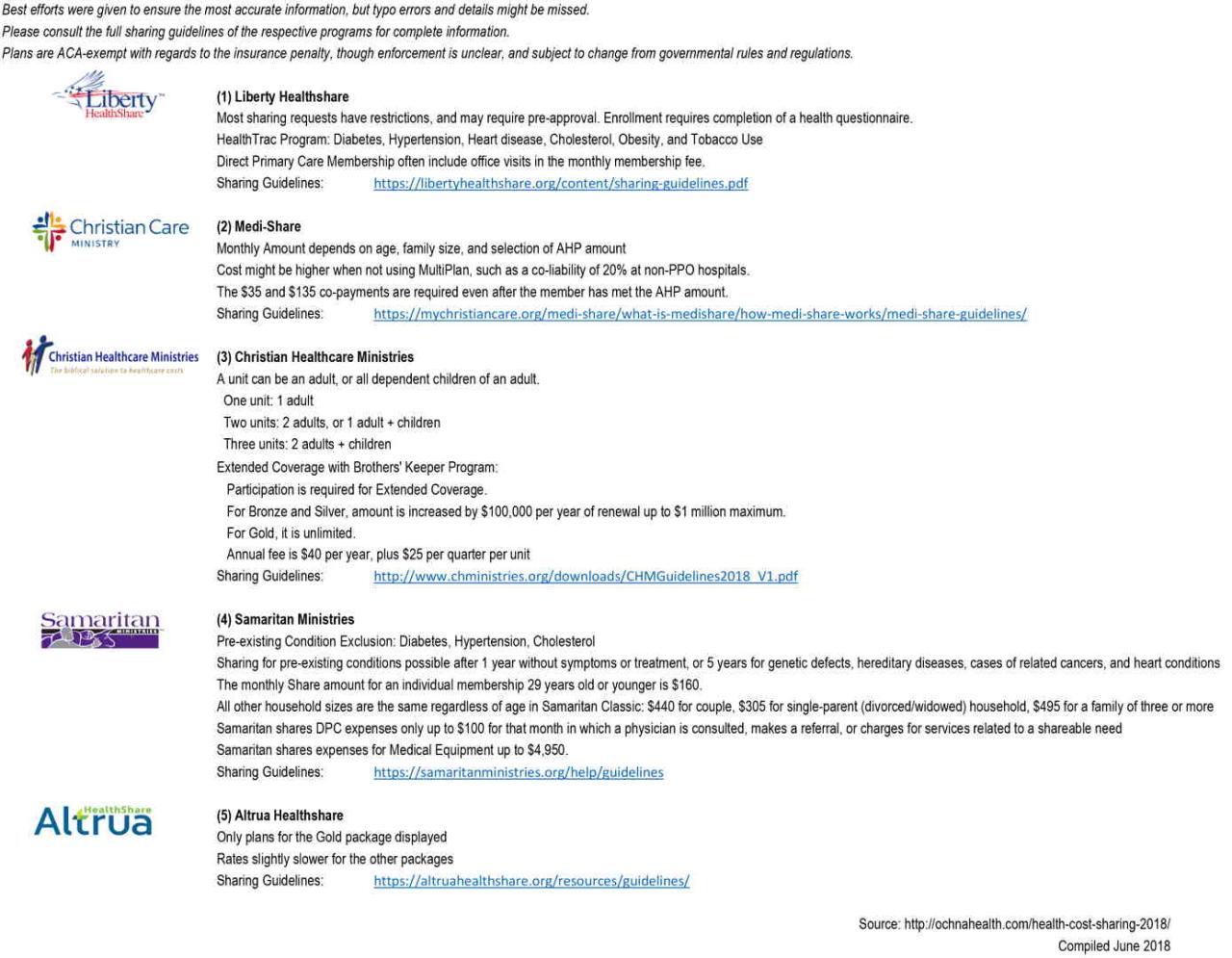
A key difference between these programs and traditional insurance lies in their structure and how they handle healthcare expenses. The following table Artikels some key features:
| Program Type | Coverage Details | Financial Structure | Religious Affiliation |
|---|---|---|---|
| Christian Health Cost Sharing Program | Coverage varies widely by program. Some may cover preventative care, while others may offer limited coverage for specific medical conditions. Often, these programs have lower out-of-pocket costs than traditional insurance plans, but coverage may be less comprehensive. | Participants contribute to a shared fund from which members access healthcare expenses. The fund may be managed by a church or community organization. Often, contributions are based on ability to pay, reflecting a communal approach to healthcare costs. | Programs are typically rooted in Christian values and principles, often facilitated by churches or faith-based organizations. Membership may be restricted to those who share similar religious beliefs. |
| Traditional Health Insurance | Comprehensive coverage for a range of medical services, including preventive care, emergency care, hospital stays, and physician visits. Coverage details depend on the specific plan chosen. | Premiums are paid to an insurance company. The insurance company covers a portion of medical expenses. Deductibles, co-pays, and coinsurance are common features. | Not specifically tied to a particular religious affiliation. Plans can be purchased by individuals or groups regardless of religious beliefs. |
The Rise of Christian Health Cost Sharing Programs Post-Obamacare
Christian health cost-sharing programs, often based on biblical principles of shared responsibility and community care, have a long history. These programs, structured differently than traditional insurance, often emphasize voluntary contributions and shared financial burdens for healthcare costs. Before the Affordable Care Act (ACA), they existed primarily as faith-based networks, sometimes with limited access and coverage.The ACA, aiming to expand health insurance coverage, inadvertently created a new landscape for these programs.
While the ACA’s mandate for most Americans to have health insurance increased access for many, it also led to a perceived need for alternative approaches, particularly for those who felt traditional insurance conflicted with their values or financial situations. This new environment fostered the growth of Christian health cost-sharing programs, as an alternative for individuals who sought healthcare coverage without compromising their faith-based principles.
Historical Context of Christian Health Cost Sharing Programs
Prior to the Affordable Care Act, Christian health cost-sharing programs often functioned as smaller, community-based networks. They were typically associated with specific denominations or faith-based organizations, with limited access and often relying on volunteer contributions and community support. Coverage was often less comprehensive than traditional insurance, with greater emphasis on preventative care and shared responsibility for expenses.
Impact of the Affordable Care Act
The Affordable Care Act (ACA) had a significant impact on the health insurance market. The law’s mandate that most Americans have health insurance increased access for many, but also created a perception of cost increases and bureaucratic complexities. This, combined with the desire for greater financial control and faith-based principles, likely contributed to the rise of Christian health cost-sharing programs as an alternative for those who wanted an alternative to traditional insurance.
Factors Contributing to Post-Obamacare Growth
Several factors contributed to the noticeable increase in Christian health cost-sharing programs after the ACA. Increased awareness of the programs, fueled by online resources and community outreach, played a key role. Furthermore, the ACA’s focus on individual responsibility for health care choices, while intended to promote wellness, potentially created a sense of autonomy for individuals seeking to manage their own healthcare costs and align their choices with their faith.
The perceived complexity and cost of traditional insurance, as well as a desire for more community-oriented and faith-based approaches, also likely contributed to this shift.
Christian health cost-sharing programs are definitely on the rise since Obamacare, offering an alternative to traditional insurance. It’s interesting to see how this plays out, especially given recent news about fake face mask exemption cards – feds warn that face mask exemption cards are fake. This highlights a broader trend of navigating complex regulations and seeking affordable healthcare options, which is likely contributing to the growth of these Christian-based programs.
Motivations for Choosing Christian Health Cost Sharing Programs
Individuals choosing Christian health cost-sharing programs over traditional insurance often have specific motivations. Understanding these motivations helps contextualize the appeal and limitations of these programs.
| Program Type | Reasons for Choice | Potential Drawbacks | Alternative Considerations |
|---|---|---|---|
| Christian Health Cost Sharing Program | Alignment with faith-based values, desire for shared responsibility, potential for lower upfront costs, emphasis on preventative care. | Limited coverage compared to traditional insurance, potential for high out-of-pocket expenses, variability in plan designs, potential challenges with accessing specialized care. | Traditional health insurance, High-deductible health plans (HDHPs) with health savings accounts (HSAs), or other alternative insurance options that offer greater coverage but potentially higher premiums. |
Financial Implications and Structures
Christian health cost-sharing programs, a growing alternative to traditional insurance, operate on a unique financial model. Understanding these mechanisms is key to evaluating the program’s suitability for various individuals and families. These programs rely on a different approach to healthcare financing, often with significant implications for individual financial burdens.These programs, by design, emphasize shared responsibility for healthcare costs.
This shared responsibility is reflected in how funds are collected and distributed, and how that affects the financial burden on participants compared to traditional insurance plans. The programs are structured in a way that aims to lower overall costs by reducing administrative expenses and promoting a more communal approach to healthcare.
Christian health cost-sharing programs are definitely on the rise since the Affordable Care Act. It’s interesting to consider how this trend connects to the struggles many Americans face with everyday health, like the fact that more than half of American workers struggle to make their lunch healthy. Ultimately, these cost-sharing programs are likely filling a gap in healthcare access for many, reflecting a broader need for affordable and potentially faith-based health solutions.
Financial Mechanisms
These programs typically operate on a system of contributions and reimbursements, often structured around the concept of cost-sharing. Participants contribute funds to a shared pool, which is then used to cover eligible healthcare expenses. The contribution amount varies depending on the program, the participant’s needs, and the overall cost of healthcare services.
Fund Collection
Funds are collected from participants through regular contributions, which can be monthly or annual payments. These payments are often determined based on factors such as family size, income, and the chosen level of coverage. In some programs, participants might contribute a fixed amount each month, while others might have a tiered system where contributions increase with higher anticipated healthcare costs.
Fund Distribution
The funds collected are then used to cover eligible healthcare expenses. The process of distributing these funds often involves a system of reimbursements. When a participant incurs a qualifying healthcare expense, they submit a claim to the program. The program reviews the claim and, if deemed eligible, reimburses a portion or all of the expense, based on the predetermined coverage guidelines.
Comparison with Traditional Insurance
A key difference lies in the level of pre-existing conditions coverage. Traditional insurance often has a pre-existing condition exclusion or a waiting period, but these cost-sharing programs may have different approaches. While traditional insurance plans provide a more comprehensive safety net for unexpected high costs, the financial burden on participants in cost-sharing programs can vary significantly depending on the program’s specific rules and the amount of individual contributions.
Cost-sharing programs generally have lower monthly premiums, which can reduce the immediate financial burden. However, the out-of-pocket expenses for participants can be higher if their healthcare needs are significant.
Cost Comparison Table
| Program Type | Estimated Annual Cost | Typical Deductibles | Out-of-Pocket Maximums |
|---|---|---|---|
| Christian Health Cost-Sharing Program (Low Coverage) | $500 – $1,000 | $500 – $1,000 | $5,000 – $10,000 |
| Christian Health Cost-Sharing Program (Medium Coverage) | $1,000 – $2,000 | $1,000 – $2,000 | $10,000 – $20,000 |
| Christian Health Cost-Sharing Program (High Coverage) | $2,000 – $3,000 | $2,000 – $3,000 | $20,000+ |
| Traditional Health Insurance (Family of Four, Bronze Plan) | $1,500 – $3,000 | $2,000 – $5,000 | $8,000 – $15,000 |
Note: These are estimates and can vary significantly depending on individual circumstances, location, and the specific program.
Impact on Healthcare Access and Affordability
Christian health cost-sharing programs, emerging in the wake of the Affordable Care Act (ACA), are presenting a unique approach to healthcare access and affordability. These programs, often rooted in faith-based principles, offer an alternative to traditional insurance models, potentially impacting both individual and market dynamics. Understanding their impact on healthcare access and affordability is crucial to assessing their role in the broader healthcare landscape.These programs, while offering a potentially lower cost option for some, raise questions about access to a wide range of services.
Do they adequately cover essential care? How do they affect the overall healthcare market, potentially influencing the availability and cost of services for everyone? Examining the specifics of access and affordability will provide a clearer picture of these programs’ impact.
Impact on Access to Healthcare Services
These programs often focus on preventative care and emphasize personal responsibility for health. This approach, while potentially beneficial for long-term health, can lead to limitations in access to specialized care, emergency services, and treatments for chronic conditions. Participants may face challenges accessing care for conditions that require ongoing management or specialized expertise. For instance, someone with a pre-existing condition might find coverage for ongoing treatment less comprehensive than a traditional insurance plan.
Comparison of Healthcare Access for Individuals Using Christian Health Cost-Sharing Programs versus Traditional Insurance
Traditional insurance plans typically offer comprehensive coverage, including preventive care, acute care, and chronic disease management. They frequently provide coverage for a broader range of services, including mental health care and substance abuse treatment. Christian cost-sharing programs, on the other hand, may have varying levels of coverage, sometimes excluding certain procedures or services. This difference in coverage can impact the quality and quantity of care individuals receive.
The access to specialist care, hospital stays, and specialized equipment may vary considerably.
Effect on Affordability of Healthcare for Participants, Christian health cost sharing programs growing in wake of obamacare
One of the primary draws of these programs is their potential for lower monthly premiums compared to traditional insurance. This reduced cost is often a significant factor for individuals and families seeking more affordable healthcare options. However, the absence of guaranteed coverage for all expenses can lead to substantial out-of-pocket costs during times of illness or injury. This is a key difference from traditional insurance that typically covers a large portion of expenses, though deductibles and co-pays still apply.
How These Programs May Affect the Overall Healthcare Market
The rise of these programs could influence the overall healthcare market in several ways. Increased competition from cost-sharing models could potentially put downward pressure on premiums for traditional insurance plans. It might also encourage a shift in the healthcare industry toward more preventative care approaches, as these programs frequently emphasize preventative health. Further, it could potentially impact the demand for specific services and the way providers structure their pricing.
This is an evolving situation, and long-term effects are still being observed.
Community and Social Aspects
Christian health cost-sharing programs, emerging in the post-Obamacare era, often incorporate strong community elements. These programs leverage faith-based networks and shared values to provide not just financial assistance, but also a support system for members navigating healthcare challenges. This emphasis on community fosters a sense of belonging and shared responsibility, creating a unique environment for healthcare access and affordability.These programs are not simply about cost-savings; they’re about fostering a supportive network within a shared belief system.
The strength of community support can be a significant factor in improving health outcomes and overall well-being. It’s a powerful social dynamic, impacting both the individual and the broader community.
Role of Faith and Community
Faith plays a central role in these programs, providing a moral compass and a framework for shared values. A sense of shared purpose and spiritual connection can motivate members to support one another in times of need, especially in healthcare-related matters. Community members, often sharing similar values and experiences, can offer practical and emotional support, fostering a sense of belonging and trust.
The religious underpinnings often emphasize compassion and care for one another, creating a strong foundation for community support within these programs.
Potential Benefits and Drawbacks of Community-Based Support Systems
Community-based support systems in these programs can offer substantial benefits. Members benefit from a network of peers who understand their experiences, providing practical advice, emotional support, and shared resources. This shared experience can also reduce feelings of isolation and empower members to actively participate in their own health journeys. However, potential drawbacks exist. Community standards and expectations, while intended to be supportive, might inadvertently create pressure or exclude individuals who don’t fully conform to those norms.
This can sometimes limit individual autonomy in healthcare decisions. Furthermore, maintaining long-term sustainability requires careful management of community dynamics and ensuring inclusivity.
Examples of Community Support in Action
| Program Type | Community Support | Potential Challenges | Long-Term Sustainability |
|---|---|---|---|
| Small, rural church-based program | Strong bonds of trust and shared values. Members actively help each other with transportation, childcare, and home-cooked meals during illness. Regular prayer meetings and encouragement are a significant aspect of support. | Potential for limited resources, especially in smaller communities. Maintaining confidentiality and avoiding judgmental attitudes among members is crucial. | Sustainability relies on maintaining active participation from church leaders and members. Ensuring the program adapts to changing community demographics and needs is vital. |
| Large, urban, denomination-based program | Access to a broader range of resources and expertise, including health professionals and financial advisors. Members can connect with support groups and mentors through online platforms. | Maintaining a sense of community connection among a larger and more diverse membership. Potential for logistical challenges in coordinating activities and ensuring equitable access to support. | Sustainability requires establishing clear governance structures, securing reliable funding streams, and diversifying leadership to address evolving needs. |
| Online, faith-based program | Provides access to a larger network of support from across geographical boundaries. Members can connect through online forums, video calls, and shared resources. | Potential for miscommunication or misinterpretations online. Ensuring the online community fosters a safe and respectful environment is critical. | Sustainability hinges on maintaining active participation, developing effective online communication channels, and recruiting and training online moderators. |
Legal and Regulatory Landscape
Christian health cost-sharing programs, while often perceived as faith-based solutions, operate within a complex legal and regulatory framework. Navigating these legal considerations is crucial for the sustainability and effectiveness of these programs. Understanding the nuances of state regulations and potential legal challenges is vital for both program administrators and participants.The legal environment surrounding these programs is not monolithic.
Differences in state laws and interpretations of existing regulations can significantly impact how these programs function. This creates a patchwork of legal standards across the United States, requiring a careful analysis of specific state regulations to ensure compliance. Furthermore, the intersection of religious freedom, healthcare access, and consumer protection creates unique challenges and opportunities for these programs.
Legal Considerations in Different States
State laws regarding religious exemptions and healthcare regulations can vary significantly. This difference in regulation can have profound implications for the structure and operation of Christian health cost-sharing programs. Some states may have explicit provisions allowing for religious exemptions in healthcare, while others may not.
Christian health cost-sharing programs are definitely gaining traction in the wake of Obamacare. It’s interesting how, alongside these developments, adopting a healthy diet like the Mediterranean diet could significantly impact brain health. This could be a huge factor for long-term health, especially when considering how these cost-sharing programs are growing in popularity to support people’s health needs. how healthy diets like the mediterranean diet help protect brain health Choosing healthier eating habits, along with these cost-sharing plans, might offer a powerful combination for overall well-being.
Regulatory Frameworks and Potential Implications
The regulatory landscape for Christian health cost-sharing programs is not always straightforward. Some states may have regulations that affect the programs’ ability to operate, while others may offer more favorable legal environments.
| State | Key Regulations | Potential Implications | Recent Legal Developments |
|---|---|---|---|
| California | Stricter regulations on health insurance alternatives, potentially impacting the structure of cost-sharing programs. Specific legal precedents may limit the scope of religious exemptions. | Potential for increased scrutiny and regulatory hurdles in program design and operation. | Recent court cases have highlighted the need for clear legal distinctions between cost-sharing programs and traditional insurance. |
| Texas | More lenient regulatory environment towards religious exemptions in healthcare. Potential for greater flexibility in structuring cost-sharing programs. | Lower regulatory burden and more opportunities for innovation in program design. | Recent legislative activity suggests an ongoing debate on the balance between religious freedom and consumer protection in healthcare. |
| New York | Complex regulatory framework with significant emphasis on consumer protection. Potential for specific requirements for transparency and disclosure. | Need for heightened compliance with disclosure and consumer protection laws. | Recent regulatory guidance has clarified the need for clear documentation of program structures and operations. |
| Florida | Regulations related to charitable organizations and non-profit entities could apply to cost-sharing programs. Specific provisions for religious exemptions may be less developed. | Compliance with tax regulations and charitable organization requirements may be crucial. | Recent cases have addressed the tax implications of similar faith-based health initiatives. |
Examples of Relevant Legislation and Court Cases
Several pieces of legislation and court cases have addressed the complexities surrounding religious exemptions in healthcare. These examples often provide insight into the potential legal challenges faced by cost-sharing programs.
“The Religious Freedom Restoration Act (RFRA) of 1993, for instance, has played a role in shaping legal interpretations regarding religious freedom in healthcare.”
These legislative acts and court rulings demonstrate the dynamic interplay between religious freedom and healthcare regulation. The evolving nature of this legal environment underscores the importance of ongoing monitoring and adaptation for Christian health cost-sharing programs.
Future Trends and Projections
Christian health cost-sharing programs are poised for continued growth and adaptation in the evolving healthcare landscape. Their resilience stems from a core principle of shared responsibility and faith-based values, which resonate with many individuals seeking alternative healthcare solutions. This ongoing evolution is driven by both internal program adjustments and external market pressures.The future of these programs hinges on their ability to navigate the complexities of healthcare reform, technological advancements, and changing community needs.
Addressing financial sustainability, accessibility, and regulatory compliance will be crucial for long-term success.
Projected Growth and Development
The continued growth of these programs is likely to be influenced by a number of factors, including increasing dissatisfaction with traditional insurance models, a desire for greater control over healthcare costs, and the ongoing need for affordable healthcare options. These programs will likely adapt and expand to serve a wider range of needs and demographics. Innovative approaches to cost-sharing mechanisms and program design are likely to emerge as these programs seek to optimize their effectiveness.
Potential Challenges
One major challenge will be maintaining financial sustainability. These programs often rely on a relatively small membership base, which can make them vulnerable to fluctuations in the healthcare market. Ensuring adequate reserves and exploring diverse funding models will be critical. Maintaining compliance with existing and emerging regulations will also be essential. Ensuring that the programs meet the legal requirements of healthcare cost sharing while maintaining the principles of faith-based cost sharing will require ongoing vigilance and adaptation.
Opportunities for Improvement
These programs have opportunities to expand their service offerings. Partnerships with local healthcare providers, including clinics, hospitals, and pharmacies, could expand access to care and potentially reduce costs. Additionally, focusing on preventative care and wellness initiatives could further improve the health and well-being of program members. Furthermore, the potential for developing a wider range of specialized services, like mental health care, could enhance the appeal and value proposition of these programs.
Impact of Healthcare Market Changes
Changes in the healthcare market, such as the rising cost of prescription drugs, the growing prevalence of chronic conditions, and the increasing demand for telehealth services, will likely influence the development of these programs. Programs may need to adapt their cost-sharing structures and benefit packages to reflect these market changes. For example, programs might introduce tiers of coverage or incorporate telehealth services into their offerings.
This proactive approach will be crucial to maintain competitiveness and member satisfaction.
Evolving Healthcare Technologies
The integration of new healthcare technologies, such as telehealth and personalized medicine, presents both opportunities and challenges for these programs. Telehealth can increase access to care and reduce costs, potentially making these programs more attractive. Personalized medicine, with its potential to predict and prevent diseases, could lead to improved health outcomes and lower healthcare costs. These programs may need to incorporate these technologies into their offerings to remain relevant and effective in the future.
However, ensuring equitable access to these technologies and navigating their potential impact on the cost-sharing model will be key.
Final Conclusion: Christian Health Cost Sharing Programs Growing In Wake Of Obamacare
In conclusion, the growth of Christian health cost-sharing programs presents a fascinating case study in the evolving healthcare landscape. While offering a potentially more affordable alternative, these programs also present unique challenges and considerations. The interplay of faith, community, and financial structures shapes their appeal, and their long-term viability depends on various factors, including regulatory environments and the evolving healthcare market.
The programs’ future trajectory is uncertain, but their continued growth and impact are undeniable.