Chronic pain can worsen mental health what can be done sets the stage for this exploration, delving into the complex interplay between physical suffering and emotional well-being. This isn’t just about managing pain; it’s about understanding how chronic pain impacts every aspect of life, from daily routines to relationships, and how we can address the mental health challenges that often accompany it.
This journey will cover the physiological connections, the impact on daily life, effective management strategies, and the crucial role of the healthcare system in providing comprehensive support.
The discussion will cover various types of chronic pain, examining how they affect mental health differently. We’ll explore the common mental health conditions often linked to chronic pain, like depression and anxiety, and compare the impact of acute versus chronic pain. We’ll also delve into practical strategies for coping with the daily challenges and the importance of seeking support.
Understanding the Connection
Chronic pain isn’t just a physical ailment; it often intertwines deeply with mental well-being. The constant discomfort, unpredictable nature, and limitations imposed by chronic pain can significantly impact mood, thoughts, and overall emotional health. This exploration delves into the intricate relationship between chronic pain and mental health, examining the physiological mechanisms, different pain types, and associated mental health conditions.The experience of chronic pain activates complex physiological pathways that extend beyond the immediate pain response.
Neurochemicals involved in the body’s stress response, like cortisol and norepinephrine, are often elevated, contributing to heightened anxiety and irritability. Prolonged pain can also disrupt sleep patterns, further exacerbating mental health issues. The constant worry about the pain’s persistence, the uncertainty about future limitations, and the difficulty managing daily activities can lead to feelings of helplessness, hopelessness, and depression.
Physiological Mechanisms
The brain’s pain processing system isn’t isolated; it’s interconnected with the regions responsible for mood, emotion, and memory. Chronic pain stimulation can lead to long-lasting changes in these brain areas, potentially altering neurotransmitter balances and creating a vicious cycle. For instance, chronic pain can trigger a cascade of inflammatory responses, which can also affect the brain and its function, influencing mood and behavior.
This connection highlights the importance of considering the mental health implications when managing chronic pain.
Different Types of Chronic Pain
Chronic pain manifests in various forms, each with its own unique impact on mental well-being. Neuropathic pain, arising from nerve damage, can often lead to heightened anxiety and fear due to the unpredictable nature of the pain signals. Musculoskeletal pain, stemming from issues with muscles, joints, or bones, can contribute to feelings of frustration and hopelessness as daily tasks become increasingly difficult.
The impact of each type is nuanced and individual, but the common thread is the disruption of daily life and the associated emotional distress.
Dealing with chronic pain can really take a toll on your mental well-being. Finding healthy coping mechanisms is key, and sometimes that involves exploring different lifestyle choices. For example, while some people wonder if sparkling water could contribute to weight gain, can sparkling water cause weight gain , the focus should still be on finding healthy, sustainable ways to manage pain and improve your overall mental health.
Ultimately, addressing chronic pain holistically is crucial for better mental well-being.
Common Mental Health Conditions
Chronic pain is frequently associated with several mental health conditions. Depression is a common co-occurring disorder, often stemming from the persistent pain, the limitations it imposes, and the associated feelings of helplessness. Anxiety disorders, characterized by excessive worry and fear, are also frequently linked to chronic pain. Post-traumatic stress disorder (PTSD) can develop in individuals who have experienced a traumatic injury or event, which can lead to long-term pain and mental health challenges.
Acute vs. Chronic Pain
Acute pain, a temporary response to injury or illness, typically doesn’t have the same long-term impact on mental health as chronic pain. While acute pain can certainly cause temporary distress, the prolonged nature and unpredictable aspects of chronic pain lead to a much greater and more sustained impact on mental well-being. The continuous threat of pain, its effect on sleep, and the perceived limitations it imposes significantly differ from the temporary nature of acute pain.
Comparison of Pain Types
| Pain Type | Common Mental Health Impact | Potential Contributing Factors | Treatment Approaches |
|---|---|---|---|
| Neuropathic Pain | Increased anxiety, fear, irritability, difficulty concentrating | Unpredictable pain patterns, sensory disturbances, nerve damage | Pharmacological interventions, nerve blocks, psychological therapies |
| Musculoskeletal Pain | Depression, frustration, hopelessness, decreased quality of life | Physical limitations, difficulty with daily tasks, chronic inflammation | Physical therapy, exercise, pain management techniques, psychological support |
| Fibromyalgia | Chronic fatigue, sleep disturbances, mood swings, anxiety | Complex interplay of genetic, environmental, and psychological factors | Multidisciplinary approach including medication, exercise, cognitive behavioral therapy |
Impact on Daily Life
Chronic pain significantly impacts every aspect of daily life, often creating a cascade of challenges that extend far beyond the physical discomfort. The constant presence of pain can reshape routines, relationships, and overall well-being, leading to feelings of isolation and despair. Understanding these impacts is crucial for developing effective coping strategies and support systems.
Interference with Daily Activities
Chronic pain can make even the simplest tasks feel overwhelming. Basic activities like showering, dressing, or preparing meals can become arduous or impossible to complete without significant effort. This disruption can lead to a decrease in productivity at work or school, impacting financial stability and overall quality of life. The inability to engage in hobbies or recreational activities further diminishes enjoyment and contributes to a sense of helplessness.
Effects on Relationships and Social Life
Chronic pain can strain relationships with family members and friends. The unpredictability and intensity of pain can lead to irritability, mood swings, and difficulty communicating effectively. Individuals experiencing chronic pain may withdraw from social activities, fearing judgment or the inability to participate fully. This isolation can worsen mental health issues and create a cycle of loneliness and despair.
Impact on Sleep Patterns and Physical Function
Chronic pain often disrupts sleep patterns. The discomfort can make it difficult to fall asleep, stay asleep, or experience restorative sleep. This lack of adequate sleep further exacerbates pain, fatigue, and other physical symptoms. The resulting decline in physical function can make daily tasks even more challenging, creating a vicious cycle of pain and disability.
Financial Burdens
Chronic pain can impose significant financial burdens. Medical expenses, including doctor visits, medications, and therapies, can be substantial. Lost wages due to missed work or reduced productivity can create financial strain. The need for assistive devices or home modifications can also contribute to increased expenses.
Social Support and Isolation
Social support is crucial for managing chronic pain and its associated mental health challenges. A strong support network can provide emotional comfort, practical assistance, and a sense of belonging. However, individuals experiencing chronic pain may struggle to maintain social connections due to limitations in their ability to participate in social activities. Isolation can amplify feelings of loneliness, hopelessness, and depression, further compounding the impact of chronic pain.
Table: Daily Activity, Impact of Chronic Pain, Coping Strategies, and Resources, Chronic pain can worsen mental health what can be done
| Daily Activity | Impact of Chronic Pain | Strategies for Coping | Resources Available |
|---|---|---|---|
| Personal Care (showering, dressing) | Can be significantly challenging and time-consuming, potentially leading to feelings of frustration and isolation. | Explore assistive devices, adjust routines, prioritize self-care, and consider pain management techniques. | Physical therapists, occupational therapists, home healthcare agencies. |
| Work/School | Reduced productivity, missed work/school days, difficulty concentrating, impacting financial stability. | Communicate with employers/teachers, explore flexible work arrangements, utilize pain management strategies, and seek accommodations. | Employee assistance programs (EAPs), disability services, vocational rehabilitation. |
| Social Activities | Difficulty participating fully, social withdrawal, feelings of isolation and loneliness. | Identify social support systems, engage in activities that are manageable, explore support groups, and prioritize mental well-being. | Support groups, online forums, community centers, mental health professionals. |
| Sleep | Disrupted sleep patterns, leading to fatigue, irritability, and worsening pain. | Establish a regular sleep schedule, create a relaxing bedtime routine, use relaxation techniques, and explore pain management strategies. | Sleep specialists, pain management clinics, sleep aids (with doctor’s approval). |
Management Strategies
Chronic pain isn’t a sentence; it’s a challenge that requires a multifaceted approach. Effective management involves addressing the physical symptoms, understanding the emotional toll, and creating a supportive environment. This section explores various strategies to help individuals navigate the complexities of chronic pain and improve their overall well-being.Managing chronic pain requires a holistic strategy that considers both physical and emotional needs.
This includes exploring various treatment options, building a supportive network, and developing coping mechanisms to effectively manage the pain and its associated stressors.
Medication Management
Medication plays a crucial role in managing chronic pain. However, it’s essential to remember that medication alone is rarely a complete solution. Pain management often requires a combination of approaches, and medications are tailored to the individual’s specific needs and pain type. Different types of medications, including over-the-counter pain relievers, opioids (used cautiously), and other prescription medications, are employed to reduce pain intensity and improve function.
It’s vital to discuss medication options with a healthcare professional to determine the most suitable course of action, considering potential side effects and interactions with other medications.
Physical Therapy
Physical therapy is an essential component of chronic pain management. Physical therapists develop personalized exercise programs to improve strength, flexibility, and mobility. These programs aim to reduce pain, improve function, and enhance overall physical well-being. Specific exercises, manual therapy techniques, and assistive devices can significantly contribute to pain reduction and improved quality of life. A physical therapist can also provide education on proper body mechanics and pain-management techniques.
Dealing with chronic pain can really take a toll on your mental well-being. Finding ways to manage it is crucial. Sometimes, seemingly unrelated issues, like the causes of miscarriages, can also be linked to underlying health conditions that impact overall well-being. For example, testing for potential causes of miscarriages can provide valuable insight into the body’s responses to stress and potential underlying conditions, and this knowledge can be incredibly helpful in managing chronic pain.
Ultimately, focusing on holistic approaches and seeking professional help are key to improving both physical and mental health.
Alternative Therapies
Alternative therapies, such as acupuncture, massage therapy, and mindfulness-based practices, can complement conventional treatments. Acupuncture involves inserting thin needles into specific points on the body, believed to stimulate energy flow and reduce pain. Massage therapy can relieve muscle tension and improve circulation, often leading to reduced pain and increased relaxation. Mindfulness practices, such as meditation and yoga, can help manage stress and pain perception, fostering a sense of calm and well-being.
While these therapies can be helpful, they are often best used in conjunction with other treatments and should be discussed with a healthcare provider.
Support Groups and Counseling
Support groups and counseling are crucial for individuals experiencing chronic pain. These platforms offer a safe space to share experiences, receive emotional support, and connect with others facing similar challenges. Support groups provide a sense of community and understanding, while counseling can provide tools and strategies to cope with the emotional and psychological impact of chronic pain. Group therapy settings, individual therapy sessions, or a combination of both, can offer valuable insights and strategies to improve emotional well-being.
Mindfulness and Stress Reduction Techniques
Mindfulness and stress reduction techniques, such as meditation, deep breathing exercises, and progressive muscle relaxation, can significantly impact both pain perception and mental health. Mindfulness practices help individuals become more aware of their thoughts and feelings without judgment, fostering a sense of calm and acceptance. Stress reduction techniques help to manage the physiological responses to stress, which can contribute to pain exacerbation.
By incorporating these techniques into daily routines, individuals can better manage both their pain and emotional well-being.
Dealing with chronic pain can take a serious toll on your mental well-being. Finding ways to manage the pain is crucial, but sometimes, seemingly unrelated factors can play a role. For example, a recent study suggests that changes in your sense of smell could be an early indicator of multiple sclerosis progression, highlighting the interconnectedness of physical and mental health.
sense of smell could be a signal of ms progression. This underscores the importance of open communication with healthcare professionals and exploring all potential avenues for managing chronic pain, as mental health is intrinsically linked to physical health.
Self-Care and Healthy Routines
Self-care is essential for individuals with chronic pain. Establishing healthy routines, including regular sleep patterns, balanced nutrition, and adequate physical activity (when possible), is crucial for overall well-being. These routines help regulate mood, reduce stress, and improve the body’s ability to heal and manage pain. Creating a supportive environment and incorporating activities that promote relaxation and joy are also key components of self-care.
Coping Mechanisms for Emotional Distress
Developing coping mechanisms for emotional distress related to chronic pain is vital. These mechanisms may include journaling, creative expression, spending time in nature, connecting with loved ones, or pursuing hobbies. Journaling can help individuals process emotions and identify patterns. Creative expression, such as painting, writing, or music, can provide an outlet for emotional release. Connecting with loved ones and engaging in hobbies can provide a sense of purpose and fulfillment.
Building a support system is vital in navigating the challenges of chronic pain.
Healthcare System and Support
Navigating the healthcare system with chronic pain can be incredibly challenging, often exacerbating the very issues it’s meant to address. Individuals with chronic pain frequently face hurdles in accessing appropriate care, communicating their needs effectively, and finding support systems that understand the complex interplay between physical and mental well-being. This section delves into the systemic issues, gaps in current models, and available resources to better support those living with this condition.The healthcare system often struggles to adequately address the multifaceted nature of chronic pain.
Traditional models often prioritize short-term solutions and objective measures, overlooking the significant role of psychosocial factors. This can lead to frustration, misdiagnosis, and a lack of personalized care, ultimately hindering the patient’s journey towards improved well-being.
Challenges in Accessing Care
Chronic pain patients often encounter difficulties accessing specialized pain management services, including timely appointments with pain specialists. Insurance coverage limitations, geographical constraints, and long waitlists for appointments can create significant barriers to receiving appropriate care. Communication breakdowns between patients, primary care physicians, and specialists are also prevalent.
Communication Barriers
Effective communication is paramount in managing chronic pain effectively. However, patients often face communication barriers with healthcare providers. This can stem from a lack of understanding of the complex experience of chronic pain, difficulties in expressing the nuances of their symptoms, and disparities in cultural backgrounds. Misunderstandings can lead to inadequate treatment plans and further emotional distress.
Gaps in Current Healthcare Models
Current healthcare models often fail to address the intricate connection between chronic pain and mental health. Treatment approaches may focus solely on the physical symptoms, neglecting the psychological impact of persistent pain. This separation can hinder the development of comprehensive care plans that address both the physical and emotional aspects of the condition. There’s a critical need for interdisciplinary teams that incorporate pain specialists, psychologists, and other healthcare professionals.
Available Resources for Patients
Fortunately, various resources are available to support individuals experiencing both chronic pain and mental health issues. These include patient advocacy groups, support groups, online forums, and telehealth platforms. These resources provide a vital network for connecting with others who understand the challenges, sharing experiences, and gaining emotional support.
Examples of Successful Interdisciplinary Pain Management Programs
Numerous successful interdisciplinary pain management programs demonstrate the efficacy of integrated care approaches. These programs often incorporate physical therapy, occupational therapy, psychological counseling, and medication management, tailored to the individual’s needs. By bringing together various specialists, these programs can offer a more holistic and personalized approach to pain management.
Table: Healthcare System and Support
| Healthcare Service | Potential Barriers | Solutions | Success Stories |
|---|---|---|---|
| Pain Specialist Access | Limited availability, long waitlists, insurance coverage restrictions | Expanding access to specialists, telehealth options, increased funding for pain clinics | Some hospitals have successfully implemented programs to shorten wait times and improve access to specialists, reducing patient distress. |
| Effective Communication | Lack of understanding of chronic pain, difficulties expressing symptoms, cultural disparities | Specialized training for healthcare providers on chronic pain management, patient-centered communication strategies, interpreter services | Programs emphasizing patient-centered care and open communication have seen positive outcomes in patient satisfaction and treatment adherence. |
| Interdisciplinary Care | Lack of coordination between specialists, fragmented care models | Formation of interdisciplinary pain management teams, clear communication protocols, shared care plans | Multidisciplinary pain clinics, with coordinated care from various specialists, have shown impressive results in improving patients’ overall well-being and reducing pain intensity. |
Future Directions: Chronic Pain Can Worsen Mental Health What Can Be Done
The journey toward better understanding and management of chronic pain’s impact on mental well-being is an ongoing one. Exciting advancements in research and technology hold the promise of more effective interventions, ultimately leading to improved quality of life for those living with this complex interplay of physical and emotional suffering. Future directions must focus on integrating pain and mental health care more seamlessly, moving beyond a fragmented approach to a holistic model.Emerging research and evolving treatment strategies offer promising pathways to a more supportive and personalized experience.
The goal is to move beyond symptom management to address the underlying causes of the pain-mental health connection, paving the way for long-term well-being.
Emerging Research and Potential Advancements
Research into the intricate neural pathways connecting pain signals to emotional responses is expanding rapidly. Scientists are exploring the role of the central nervous system in both processing pain and influencing mood, which holds the key to developing more targeted therapies. These insights can lead to the creation of novel interventions tailored to individual needs, focusing on mechanisms beyond just pain relief.
Potential Approaches to Integrated Care
Integrating pain management and mental health care demands a collaborative approach. This means breaking down silos between healthcare professionals, fostering communication and shared decision-making. Creating multidisciplinary teams that include pain specialists, mental health professionals, and other relevant experts can improve care coordination and patient outcomes. Examples of this integrated approach are already emerging, with successful programs combining physical therapy, cognitive behavioral therapy (CBT), and mindfulness techniques to address the multifaceted nature of chronic pain and its impact on mental well-being.
Promising New Treatment Modalities
New treatment modalities show great potential for addressing both the physical and emotional aspects of chronic pain. These include:
- Neuromodulation techniques: These methods, such as transcranial magnetic stimulation (TMS) and spinal cord stimulation, offer promising avenues for modulating pain signals in the nervous system. These therapies can offer significant pain relief, which, in turn, can reduce the burden of pain-related distress and improve mood.
- Mindfulness-based interventions: Programs focusing on mindfulness and acceptance can help individuals develop coping mechanisms to manage pain-related distress and negative emotions. Mindfulness practices have demonstrated effectiveness in reducing anxiety and depression associated with chronic pain.
- Virtual reality (VR) therapies: VR environments can be used to create controlled and immersive experiences for pain management and mental health. This can provide a safe space for individuals to confront pain-related fears and anxieties, leading to increased coping skills and reduced pain perception.
The Need for Increased Research and Awareness
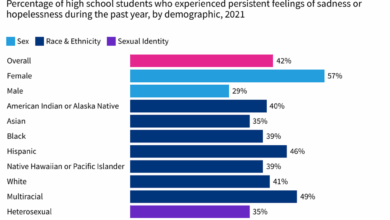
Research funding and public awareness of the connection between chronic pain and mental health are crucial for driving progress. The co-occurrence of these conditions demands more in-depth investigation into the underlying mechanisms and effective interventions. A greater understanding of this interplay is essential for creating targeted interventions and policies that support individuals and families affected by chronic pain.
Increased research will illuminate the specific vulnerabilities of certain demographics and provide data for tailoring treatment plans.
Promoting a Patient-Centered Approach
A truly patient-centered approach prioritizes individual needs, preferences, and values. This involves active listening, empathy, and shared decision-making. Empowering patients to take an active role in their care, through education and support groups, allows them to better manage their condition. This can significantly improve outcomes by fostering a sense of control and agency in managing the multifaceted aspects of chronic pain and its impact on their lives.
Furthermore, accessible and culturally sensitive care can address the needs of diverse patient populations more effectively.
Last Recap
In conclusion, chronic pain significantly impacts mental well-being. This exploration has highlighted the multifaceted nature of this issue, demonstrating the interconnectedness of physical and emotional health. By understanding the mechanisms, impacts, and available strategies, individuals facing chronic pain can navigate these challenges with more effective coping mechanisms and support. Ultimately, this journey underscores the importance of holistic approaches to care, recognizing that pain management extends beyond medication and therapy to encompass the emotional, social, and practical aspects of daily life.