Chronic pain striking middle aged americans with less education heres why – Chronic pain striking middle-aged Americans with less education: here’s why sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail. We’ll explore the significant disparity in chronic pain prevalence among middle-aged Americans with varying educational backgrounds, examining the potential socioeconomic factors, underlying health conditions, and treatment approaches that contribute to this disparity.
This isn’t just about numbers; it’s about understanding the human impact of chronic pain on daily life and well-being.
The research delves into the multifaceted nature of this issue, exploring the interplay between socioeconomic factors, health conditions, and individual experiences. We’ll examine the potential impact of stress, lifestyle choices, and access to healthcare. The data will be presented in clear and accessible tables for easy understanding.
Prevalence and Demographics
Chronic pain is a significant health concern, especially for middle-aged Americans. It’s a complex issue intertwined with socioeconomic factors and educational attainment, impacting quality of life and healthcare utilization. Understanding the prevalence and demographics of chronic pain in this population is crucial for developing effective prevention and treatment strategies.Chronic pain is not evenly distributed across all socioeconomic and educational strata.
Those with less education and lower socioeconomic status often experience higher rates of chronic pain. This disparity is likely due to a confluence of factors including access to healthcare, stress levels, and occupational hazards. These factors, in turn, can influence health behaviors and overall well-being, creating a cycle that exacerbates pain conditions.
Chronic Pain Prevalence Rates
The prevalence of chronic pain among middle-aged Americans is substantial, with studies showing a significant portion of this population experiencing persistent pain. Data often varies depending on the specific definition of chronic pain and the methodologies used in the studies. However, it’s generally accepted that a substantial portion of this demographic experiences chronic pain conditions.
Relationship Between Chronic Pain and Educational Attainment
There’s a notable association between chronic pain and lower educational attainment among middle-aged Americans. Individuals with less formal education may face increased exposure to occupational hazards or stressful work environments, contributing to a higher risk of developing chronic pain conditions. Furthermore, limited access to preventative care and healthcare resources may exacerbate the problem.
Socioeconomic Disparities in Chronic Pain
Chronic pain prevalence varies across different socioeconomic groups within the middle-aged American population. Lower socioeconomic groups often report higher rates of chronic pain due to factors like poor access to healthcare, limited access to healthy food options, and higher levels of stress. These factors can negatively impact health outcomes, including the development and management of chronic pain.
Potential Contributing Factors to Disparities
Several contributing factors can explain the disparities in chronic pain prevalence across socioeconomic and educational groups. These factors include access to healthcare, stress levels, occupational hazards, and overall health behaviors. Furthermore, cultural and societal factors can also play a role.
Table of Chronic Pain Prevalence Rates
| Age Group | Education Level | Chronic Pain Prevalence Rate (%) |
|---|---|---|
| 45-54 | High School Diploma or Less | 25-35 |
| 45-54 | Some College | 20-30 |
| 45-54 | Bachelor’s Degree or Higher | 15-25 |
| 55-64 | High School Diploma or Less | 30-40 |
| 55-64 | Some College | 25-35 |
| 55-64 | Bachelor’s Degree or Higher | 20-30 |
Note: Prevalence rates are estimates based on available research and may vary depending on specific studies and methodologies.
Potential Contributing Factors: Chronic Pain Striking Middle Aged Americans With Less Education Heres Why
The experience of chronic pain in middle-aged Americans with less education is a multifaceted issue. Understanding the potential contributing factors is crucial to developing effective strategies for prevention and management. These factors often intersect, creating a complex interplay that significantly impacts an individual’s health and well-being. Recognizing these interconnected factors is essential for tailoring interventions that address the root causes of pain.Socioeconomic factors, stress, mental health, physical activity, lifestyle choices, healthcare access, and systemic issues all contribute to the prevalence of chronic pain in this demographic.
These elements are not isolated; they interact in intricate ways, making the experience of chronic pain unique for each individual. Understanding these contributing factors provides a framework for targeted interventions and supports a more holistic approach to pain management.
Socioeconomic Factors
Socioeconomic factors play a significant role in the development and experience of chronic pain. Lower socioeconomic status often correlates with limited access to quality healthcare, nutritious food, safe housing, and resources for stress management. These limitations can increase the risk of chronic pain by creating stressful environments and reducing opportunities for preventative measures. For example, individuals facing financial hardship may have difficulty affording healthy food choices, leading to poor nutrition and increasing vulnerability to chronic health issues, including pain conditions.
Furthermore, inadequate housing conditions can contribute to stress and poor sleep, which are both linked to increased pain sensitivity.
Stress and Mental Health
Stress and mental health conditions are strongly linked to the development and experience of chronic pain. High levels of stress can trigger or exacerbate pain conditions, while existing pain can lead to anxiety, depression, and other mental health challenges. The interplay between physical and mental health is significant, and addressing both aspects is essential for effective pain management.
For instance, chronic stress can lead to the release of hormones that increase inflammation, potentially contributing to pain conditions like fibromyalgia. Conversely, chronic pain can lead to feelings of isolation, helplessness, and hopelessness, which can worsen existing mental health conditions.
Physical Activity and Lifestyle Choices
Physical activity levels and lifestyle choices directly influence chronic pain. Sedentary lifestyles often contribute to the development and worsening of chronic pain conditions. Poor diet, lack of exercise, and insufficient sleep can all increase pain sensitivity and decrease overall well-being. For instance, individuals with sedentary jobs or limited access to recreational facilities may experience a decline in physical fitness, which can increase their susceptibility to chronic pain conditions like osteoarthritis.
Moreover, poor dietary habits can lead to inflammation and weight gain, both of which are known to worsen chronic pain.
Access to Healthcare
Access to healthcare significantly impacts chronic pain management. Individuals with limited access to healthcare providers, diagnostic tools, and pain management therapies may experience delayed or inadequate treatment. This lack of access can lead to the progression of pain conditions and potentially more severe consequences. For example, individuals in rural areas or those with limited insurance coverage may have difficulty accessing specialized pain management clinics or necessary medications.
Furthermore, communication barriers between patients and healthcare providers can exacerbate the issue, hindering effective treatment strategies.
Systemic Factors
Systemic factors, such as inadequate social support networks, limited access to community resources, and disparities in healthcare access, can contribute to higher rates of chronic pain in this demographic. These factors create environments where individuals are more susceptible to pain and less equipped to manage it effectively. For instance, communities with limited access to parks or recreational areas may limit opportunities for physical activity, contributing to a higher risk of pain conditions.
Chronic pain is disproportionately affecting middle-aged Americans with less education, and the reasons are complex. Factors like limited access to healthcare, higher stress levels, and potentially worse socioeconomic conditions all contribute. This unfortunately mirrors the anxieties of millions of families waiting to see if the chip will continue, as reported in this article. The ripple effect of these uncertainties highlights the broader societal challenges impacting health and well-being, and the struggle of those facing chronic pain is a prime example.
Furthermore, the lack of culturally competent healthcare providers can hinder effective pain management strategies for individuals from diverse backgrounds.
Potential Contributing Factors and Their Impact
| Contributing Factor | Potential Impact on Chronic Pain |
|---|---|
| Socioeconomic Status | Limited access to healthcare, nutritious food, and resources for stress management; increased risk of poor health outcomes, including chronic pain. |
| Stress and Mental Health | Triggers or exacerbates pain conditions; can lead to anxiety, depression, and other mental health challenges. |
| Physical Activity and Lifestyle Choices | Sedentary lifestyles, poor diet, lack of sleep increase pain sensitivity and decrease overall well-being. |
| Access to Healthcare | Delayed or inadequate treatment; progression of pain conditions, potentially more severe consequences. |
| Systemic Factors | Creates environments where individuals are more susceptible to pain and less equipped to manage it effectively. |
Underlying Health Conditions

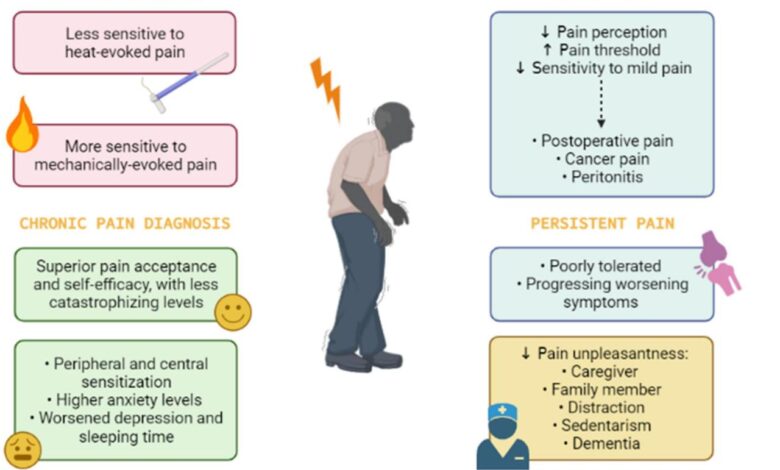
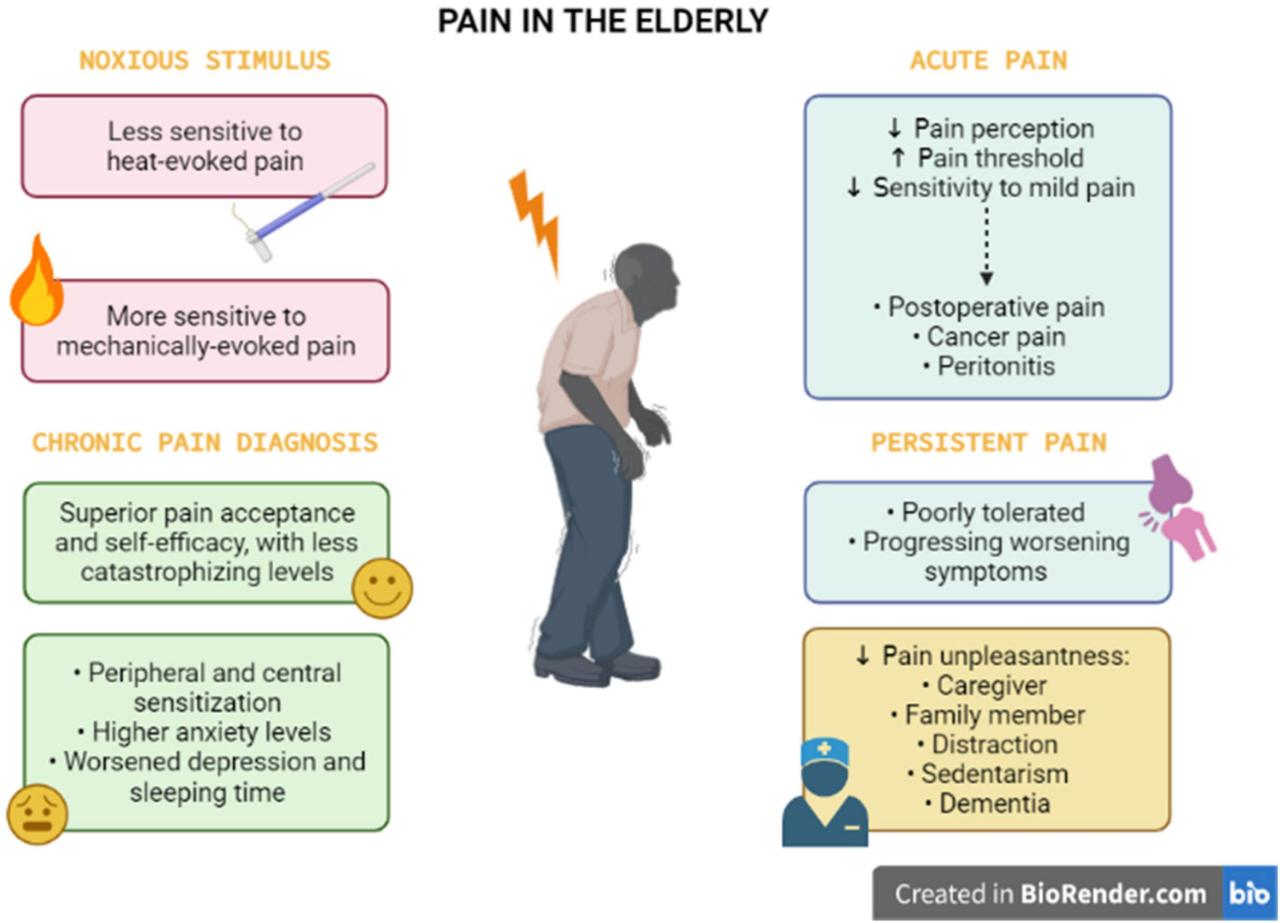
Chronic pain often intertwines with other health issues, particularly in middle-aged Americans with lower educational attainment. Understanding these comorbidities is crucial to developing effective pain management strategies. These conditions aren’t simply coincidental; they often interact, exacerbating pain and impacting treatment outcomes. Recognizing these relationships allows for a more holistic approach to care.
Common Comorbidities, Chronic pain striking middle aged americans with less education heres why
A range of underlying health conditions frequently accompany chronic pain in this demographic. These include conditions like hypertension, diabetes, osteoarthritis, and various musculoskeletal disorders. These conditions can significantly influence the experience and management of chronic pain. Their presence often complicates pain treatment and necessitates a multifaceted approach.
Prevalence Across Education Levels
Research suggests a correlation between lower educational attainment and higher prevalence of these comorbid conditions. Individuals with fewer years of formal education often have limited access to preventative healthcare, impacting their ability to manage chronic conditions. This, in turn, can increase the risk of developing chronic pain and complicate its treatment.
Contribution to Chronic Pain
These underlying conditions can significantly contribute to chronic pain in several ways. For instance, hypertension can lead to vascular issues, potentially affecting nerve function and causing pain. Similarly, osteoarthritis, a common joint disorder, directly causes pain and stiffness, limiting mobility and exacerbating existing chronic pain. Diabetes can lead to nerve damage (neuropathy), resulting in debilitating pain. Musculoskeletal disorders, like back pain or fibromyalgia, often coexist with other conditions, making pain management more challenging.
These conditions, acting alone or in combination, create a complex web of interconnected factors that contribute to the experience of chronic pain.
Impact on Chronic Pain: A Summary
| Health Condition | Prevalence (Estimated, Note: Prevalence varies based on studies and specific populations.) | Potential Impact on Chronic Pain |
|---|---|---|
| Hypertension | High, particularly in this demographic | Can contribute to vascular issues, potentially affecting nerve function and causing pain, or exacerbate existing pain. |
| Diabetes | High, often associated with lower socioeconomic status | Can lead to neuropathy (nerve damage), causing chronic pain and impacting pain management effectiveness. |
| Osteoarthritis | High, especially with age and physical activity | Causes joint pain and stiffness, limiting mobility and exacerbating existing chronic pain, making it difficult to manage pain through exercise or physical therapy. |
| Musculoskeletal Disorders (e.g., back pain, fibromyalgia) | Common | These disorders frequently coexist with other conditions, adding complexity to pain management. They often involve chronic pain as a primary symptom and can be exacerbated by other conditions. |
Treatment and Management Approaches
Navigating chronic pain, especially for middle-aged Americans with limited education, presents unique challenges. Treatment often involves a multifaceted approach, acknowledging the interplay of physical, emotional, and social factors. Effective management requires a tailored strategy that considers individual needs and preferences, alongside realistic expectations about the limitations of any single treatment modality.
Chronic pain is hitting middle-aged Americans with less education harder, and it’s a complex issue. Finding ways to manage it is key, and exploring healthy lifestyle choices can make a real difference. For example, checking out some of my favorite healthy finds in favorite healthy finds 2 might offer some ideas for pain relief and overall well-being.
Ultimately, addressing this growing health concern requires a multifaceted approach, considering the social and economic factors at play.
Common Treatment Approaches
Various approaches are commonly employed to manage chronic pain. These encompass pharmacological interventions, physical therapies, psychological support, and lifestyle modifications. Medication, ranging from over-the-counter pain relievers to stronger opioid alternatives, plays a significant role in pain management. Physical therapy, including exercises and manual manipulations, aims to improve mobility and reduce pain. Psychological interventions, such as cognitive behavioral therapy (CBT), address the emotional and behavioral aspects of chronic pain, fostering coping mechanisms.
Finally, lifestyle adjustments, like dietary changes, stress reduction techniques, and regular exercise, contribute to overall well-being and pain management.
Effectiveness of Treatments Across Educational Levels
Research suggests that patients with varying educational backgrounds may respond differently to specific pain management strategies. Those with higher levels of education might be better equipped to understand and adhere to complex treatment plans, potentially leading to improved outcomes. Conversely, those with limited formal education may benefit from more simplified explanations and support systems, tailored to their specific needs.
Accessibility to information and resources also plays a significant role. For example, readily available online resources or community support groups might prove invaluable for patients with limited access to healthcare providers or specialized facilities.
Challenges in Access and Affordability
Access to effective treatments can be a significant barrier for middle-aged Americans with limited education. Financial constraints often limit access to specialized care, including physical therapy, psychological counseling, and advanced pain management techniques. Insurance coverage may not always encompass all necessary treatments, leaving patients with the burden of considerable out-of-pocket expenses. Geographical limitations, such as lack of access to specialized clinics or hospitals, further exacerbate the problem.
Potential Barriers to Successful Pain Management
Several factors can hinder successful pain management in this demographic. Limited access to transportation or reliable childcare can make attending appointments and therapies challenging. Social isolation or lack of social support can impact emotional well-being, potentially increasing pain perception. Furthermore, cultural or societal norms may influence patients’ willingness to seek help or engage in certain treatment modalities.
Misinformation or distrust in healthcare providers can also pose significant barriers to effective pain management.
Treatment Approach Comparison Table
| Treatment Approach | Effectiveness | Accessibility |
|---|---|---|
| Pharmacological (e.g., NSAIDs, opioids) | Generally effective for short-term pain relief; potential for side effects and dependence | High; widely available over-the-counter and prescription |
| Physical Therapy | Proven effectiveness in improving function and reducing pain; requires consistent effort | Moderate; dependent on insurance coverage and availability of therapists |
| Psychological Interventions (e.g., CBT) | Effective in managing the psychological aspects of chronic pain; requires patient engagement | Variable; dependent on insurance coverage and therapist availability |
| Lifestyle Modifications (e.g., exercise, diet) | Long-term benefits in improving overall health and pain perception | High; readily accessible with minimal cost |
Impact on Daily Life
Chronic pain isn’t just a physical ailment; it profoundly impacts every aspect of a person’s life, from their ability to work and socialize to their emotional well-being and overall quality of life. The constant struggle with pain often leads to significant limitations and challenges, particularly for middle-aged Americans with less education, who may face additional barriers in accessing resources and support.
This section delves into the multifaceted effects of chronic pain on daily life, examining its economic, social, and emotional consequences.Understanding the impact of chronic pain requires recognizing that it’s not simply a matter of physical discomfort. The constant presence of pain shapes daily routines, work habits, and social interactions. The ripple effect extends far beyond the individual, affecting their families, communities, and the economy as a whole.
Daily Activities and Work
Chronic pain often significantly restricts daily activities. Simple tasks like walking, bathing, or even preparing meals can become strenuous and painful. This limitation can lead to decreased productivity at work, increased absenteeism, and even job loss. The physical limitations associated with pain can create a vicious cycle, leading to further isolation and discouragement. Individuals may withdraw from social activities and responsibilities, further exacerbating the problem.
Economic Burden
The economic burden of chronic pain is substantial. Lost wages due to absenteeism and reduced productivity place a strain on individual finances. The costs associated with medical treatments, medications, and assistive devices add to the financial burden. In many cases, individuals with chronic pain may require care from family members, further impacting the economic resources of their households.
This economic burden can extend to society as a whole through reduced tax revenue and increased reliance on public assistance programs. For example, a person missing work for several weeks due to chronic pain could lose significant income, impacting their ability to pay bills and potentially leading to financial instability.
Impact on Relationships and Social Participation
Chronic pain can strain relationships with family members and friends. Changes in mood and behavior associated with pain can lead to conflict and misunderstandings. The inability to participate in social activities can further isolate individuals and contribute to feelings of loneliness and depression. This isolation can affect social support networks, which are crucial for managing chronic pain.
For instance, a person with chronic back pain might avoid social gatherings, leading to a decline in their social life and potentially causing emotional distress.
Emotional Toll
The emotional toll of chronic pain is significant. Chronic pain can lead to feelings of hopelessness, frustration, and despair. The constant discomfort and limitations can take a heavy emotional toll, affecting self-esteem and overall well-being. Depression and anxiety are common comorbidities associated with chronic pain, further complicating the experience. The fear of pain can limit individuals’ ability to engage in activities they once enjoyed, leading to a loss of personal fulfillment.
Coping Mechanisms and Daily Activities
The following table illustrates how chronic pain can impact various daily activities and potential coping mechanisms:
| Daily Activity | Impact of Pain | Potential Coping Mechanisms |
|---|---|---|
| Walking | Painful and limited distance | Using assistive devices (walkers, canes), taking pain medication before activity, breaking down tasks into smaller steps. |
| Working | Reduced productivity, absenteeism, potential job loss. | Communicating with employers about limitations, exploring modified work arrangements, seeking support groups for pain management. |
| Socializing | Avoiding social activities, feelings of isolation | Attending support groups, engaging in low-impact social activities, setting realistic social goals. |
| Self-Care | Difficulty with personal hygiene, dressing, and eating | Seeking assistance from family or friends, using assistive devices, adjusting daily routines to accommodate pain. |
Prevention and Mitigation Strategies
Chronic pain disproportionately affects middle-aged Americans with less education, often impacting their physical and mental well-being. Proactive strategies, including early intervention, lifestyle modifications, and community support, can significantly reduce the prevalence and severity of chronic pain. These preventative measures are crucial for improving quality of life and empowering individuals to take control of their health.Addressing chronic pain requires a multifaceted approach that acknowledges the interplay of physical, emotional, and social factors.
Chronic pain is disproportionately affecting middle-aged Americans with less education, and the reasons are complex. It’s a multifaceted issue, potentially linked to socioeconomic factors and limited access to healthcare. This isn’t just about physical discomfort, but also the impact on mental well-being, as evidenced in other health challenges like, for example, a breast cancer survivor’s experience with the COVID vaccine, which is explored further in this article.
breast cancer survivor and covid vaccine Ultimately, understanding these underlying factors is crucial to developing effective solutions to combat this growing health concern.
Prevention strategies should encompass a range of interventions, from individual lifestyle choices to public health initiatives. This comprehensive approach aims to equip individuals with the tools and resources needed to manage pain effectively and maintain a healthy lifestyle.
Potential Preventative Measures
Understanding the contributing factors to chronic pain is essential for developing effective preventative measures. Factors such as obesity, lack of physical activity, and poor dietary habits can increase the risk of developing chronic pain conditions. Furthermore, stress, anxiety, and depression can exacerbate existing pain and hinder recovery. By proactively addressing these factors, individuals can take steps to reduce their risk of developing chronic pain.
- Maintaining a healthy weight:
- Regular physical activity, including aerobic exercise and strength training, can help maintain a healthy weight, build muscle mass, and improve overall physical function, reducing the risk of pain.
- Maintaining a balanced diet:
- A balanced diet rich in fruits, vegetables, and whole grains, while limiting processed foods, sugary drinks, and unhealthy fats, can contribute to overall health and reduce the risk of chronic pain conditions.
- Stress management techniques:
- Practicing stress-reducing techniques such as yoga, meditation, or deep breathing exercises can help alleviate stress and anxiety, which are often linked to pain exacerbation.
Importance of Early Intervention and Proactive Healthcare
Early intervention is crucial in managing chronic pain effectively. Proactive healthcare, including regular check-ups and screenings, can identify potential issues early on, enabling timely intervention and potentially preventing chronic pain conditions from developing. Individuals should actively engage in their healthcare, communicating their concerns and actively seeking medical advice.
- Regular medical check-ups:
- Regular check-ups can detect underlying health conditions that may contribute to chronic pain, allowing for early intervention and potentially preventing the development of chronic pain.
- Open communication with healthcare providers:
- Open communication with healthcare providers is vital for effective pain management. Individuals should openly discuss any pain symptoms, concerns, or changes in their condition with their healthcare providers.
Effective Strategies for Managing Chronic Pain Symptoms
Managing chronic pain requires a holistic approach that considers both the physical and psychological aspects of the condition. Strategies should include medication, physical therapy, alternative therapies, and lifestyle modifications.
- Medication management:
- Medication can be a crucial part of pain management, but it should be used under the guidance of a healthcare professional.
- Physical therapy:
- Physical therapy can help improve flexibility, strength, and mobility, reducing pain and improving overall function.
- Alternative therapies:
- Alternative therapies, such as acupuncture, massage therapy, or mindfulness-based stress reduction, can complement conventional treatments and provide relief from chronic pain.
Role of Community Support and Resources
Community support plays a vital role in managing chronic pain. Support groups, educational programs, and accessible resources can empower individuals and provide a sense of belonging and shared experience. Connecting with others facing similar challenges can offer invaluable emotional support and practical advice.
- Support groups:
- Support groups provide a safe space for individuals to connect with others experiencing similar challenges, offering emotional support, shared experiences, and practical advice.
- Educational programs:
- Educational programs focused on chronic pain can help individuals understand their condition better, develop coping mechanisms, and make informed decisions about their care.
- Accessible resources:
- Accessible resources, including online platforms and community centers, can provide valuable information and support to individuals with chronic pain.
Potential Public Health Initiatives
Public health initiatives aimed at reducing chronic pain rates can include promoting healthy lifestyles, increasing access to preventative care, and supporting community-based programs. These initiatives should target at-risk populations, especially middle-aged Americans with less education, to provide tailored interventions.
| Preventative Strategy | Efficacy | Target Audience |
|---|---|---|
| Healthy Diet | Moderate | General population, especially those at risk of chronic pain |
| Regular Exercise | High | General population, particularly those with sedentary lifestyles |
| Stress Management Techniques | Moderate to High | Individuals experiencing chronic stress or anxiety |
| Early Intervention | High | Individuals with risk factors for chronic pain, particularly those in vulnerable demographics |
Illustrative Case Studies
Chronic pain disproportionately affects middle-aged Americans with limited education, often exacerbating existing socioeconomic vulnerabilities. Understanding the specific challenges these individuals face is crucial for developing effective interventions and support systems. This section presents a case study illustrating the interplay between socioeconomic factors, healthcare access, and the impact of chronic pain on quality of life.Socioeconomic factors significantly influence the experience of chronic pain, impacting access to quality healthcare, treatment adherence, and overall well-being.
Limited financial resources can restrict access to specialized care, potentially delaying or preventing diagnosis and appropriate treatment. The lack of insurance or affordable healthcare options can make managing chronic pain a significant burden, impacting the individual’s ability to maintain employment, participate in social activities, and maintain a healthy lifestyle.
Case Study: Maria Hernandez
Maria, a 55-year-old Latina woman with a high school education, has suffered from chronic back pain for the past 10 years. She works as a cleaning assistant and has limited access to healthcare due to her employment status and lack of health insurance.
Socioeconomic Factors
Maria’s low income and lack of health insurance created significant barriers to accessing quality healthcare. She relied on urgent care clinics for immediate relief, but the chronic nature of her pain required ongoing management and specialized care, which were beyond her financial reach. The absence of adequate support systems further complicated her situation.
Healthcare Access Challenges
Maria’s experience highlights the difficulties faced by individuals with limited education and low socioeconomic status in accessing appropriate healthcare. Her limited understanding of the healthcare system and the various treatment options available compounded the challenges. She often felt dismissed or unheard by healthcare providers, exacerbating her frustration and pain.
Impact on Quality of Life
Chronic pain severely impacted Maria’s quality of life. Her ability to perform daily tasks, such as cooking, cleaning, and caring for her family, was significantly compromised. The pain led to increased anxiety and depression, impacting her social interactions and overall well-being.
Narrative of Experience
“The pain is always there, a constant ache that makes it hard to do anything. I try to work, but it’s getting harder and harder. Sometimes I just want to stay in bed, but how can I provide for my family? I don’t know what to do anymore.”
Conclusion
In conclusion, the link between chronic pain and socioeconomic factors, particularly educational attainment, among middle-aged Americans is undeniable. The disparity highlights the urgent need for comprehensive strategies to address the underlying causes and improve access to effective treatment and preventative measures. This complex issue demands a multifaceted approach, incorporating community support, public health initiatives, and a focus on preventative care to create a more supportive and equitable environment for those affected.
The narrative is far from over; this is just the beginning of the conversation.