Could Medicaid for All actually work? This complex question delves into the potential of a universal healthcare system based on the Medicaid model. It examines the core principles, potential variations in implementation, and the financial, administrative, and operational challenges. We’ll explore the potential benefits, considering equity and access, the impact on healthcare providers, and the long-term sustainability of such a system.
Get ready for a deep dive into the complexities of healthcare reform.
The concept of “Medicaid for All” proposes a significant overhaul of the current healthcare system in the United States, aiming to provide comprehensive coverage to all citizens. This model would expand the existing Medicaid program to encompass everyone, significantly altering the landscape of healthcare financing, delivery, and access. We’ll dissect the core components and examine the potential consequences for different stakeholders.
Defining Medicaid for All
A “Medicaid for All” system, in its most comprehensive form, envisions a nation where all citizens have access to comprehensive health coverage. This model builds upon the existing Medicaid program, expanding eligibility to encompass the entire population. It aims to eliminate financial barriers to healthcare, ensuring everyone receives necessary medical services, regardless of income or employment status. This contrasts with the current system where eligibility is often tied to income and employment.This system is not a simple, one-size-fits-all solution.
It encompasses various potential implementation strategies, ranging from a complete overhaul of the current system to a phased rollout, incorporating existing programs and regulations. The variations in implementation directly affect the potential impact on existing Medicaid programs and eligibility criteria. The long-term consequences, such as the financial burden on the government and the administrative complexities, are significant factors to consider.
Different countries offer examples of universal healthcare systems, providing insights into the successes and challenges of such models.
Core Principles of Medicaid for All
The core principles of a Medicaid for All system are rooted in the concept of universal access. This means ensuring that everyone has the right to healthcare, regardless of their ability to pay. Key features include a public health insurance program, potentially administered by a government agency or a public-private partnership. This program will likely be financed through a combination of general tax revenue and possibly payroll taxes.
A crucial element is the elimination of medical debt and the reduction of financial barriers to accessing healthcare services. These principles are central to ensuring equitable access to quality healthcare for all.
Variations in Implementation
Implementation strategies for a Medicaid for All system can range from a complete overhaul of the current system to a phased approach. A complete overhaul would involve immediately replacing all existing insurance programs with a single, nationwide Medicaid program. This approach necessitates a significant restructuring of the healthcare infrastructure and the creation of new administrative structures.
- A phased approach, on the other hand, would gradually expand Medicaid coverage to encompass more individuals over time. This method would likely involve incremental changes to eligibility criteria and funding mechanisms, minimizing the immediate financial burden on taxpayers and the transition process.
- Another approach would be to incorporate the current Medicaid programs into a broader universal healthcare system. This strategy might preserve some aspects of the current system while expanding eligibility and benefits to all.
Impact on Existing Medicaid Programs
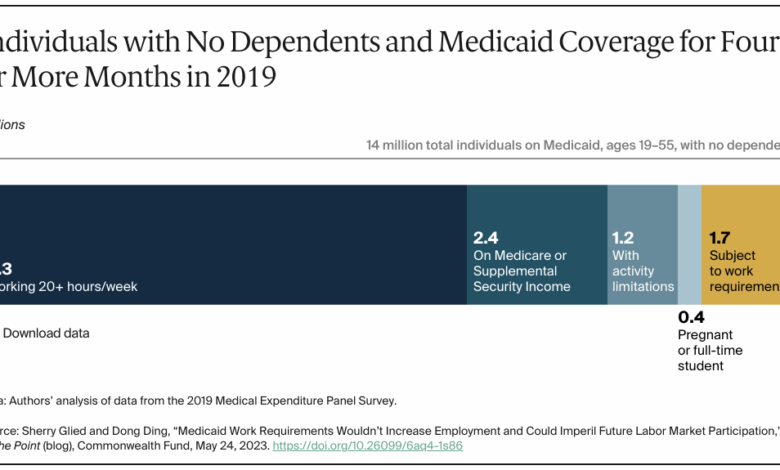
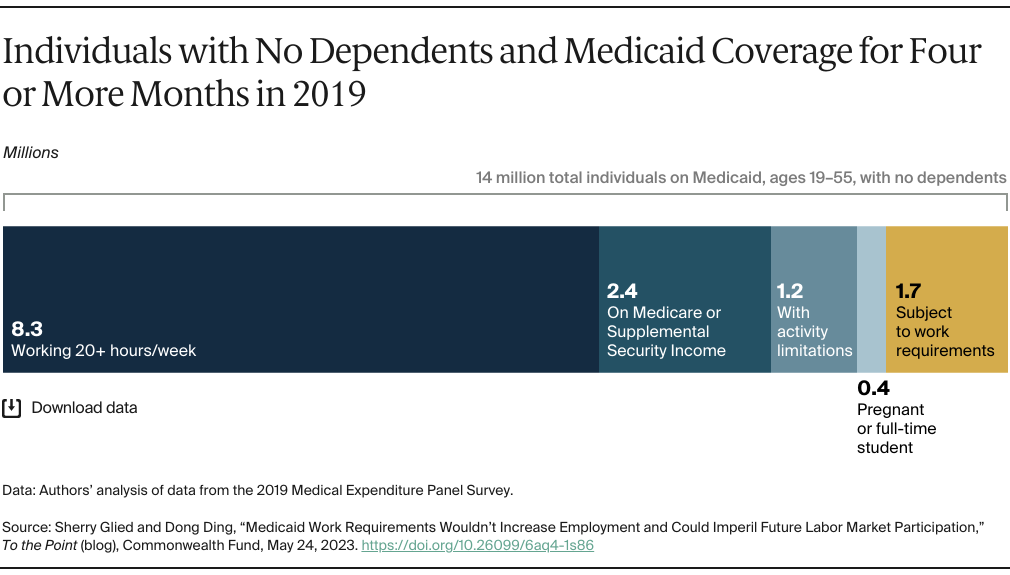
The introduction of a Medicaid for All system would have a substantial impact on existing Medicaid programs. The current system’s eligibility criteria and funding mechanisms would likely be adjusted to align with the principles of universal coverage. This adjustment could include an expansion of eligibility to cover a wider range of incomes, potentially leading to a significant increase in the number of enrollees.
The potential impact on the administrative burden on state governments and the allocation of resources is a crucial aspect to consider.
Examples of Universal Healthcare Systems
Various countries have successfully implemented universal healthcare systems. Canada’s system, for instance, provides universal coverage through a combination of provincial and federal programs. Similarly, the UK’s National Health Service (NHS) offers universal coverage funded primarily through general taxation. These systems, while similar in their goal of universal access, differ in their specific structures, funding models, and healthcare service delivery.
- Comparing the Canadian and UK systems with a potential “Medicaid for All” model in the US reveals both similarities and differences. All three systems prioritize universal access but vary in their funding mechanisms and levels of public control over the healthcare system. The impact of these variations on healthcare quality, efficiency, and cost control is a topic worthy of further exploration.
- Analyzing the implementation of these models in different contexts allows for a comprehensive understanding of the challenges and opportunities associated with achieving universal health coverage.
Financial Implications

The financial implications of a “Medicaid for All” system are a complex and often debated aspect of the proposal. Understanding the projected costs, potential revenue streams, and comparison to existing models is crucial for a comprehensive evaluation. This analysis delves into the financial landscape, exploring potential costs and potential savings, as well as the impact on taxpayers and different demographics.
Projected Costs
Estimating the precise cost of a “Medicaid for All” system is challenging, but various factors must be considered. Current healthcare spending, administrative costs, and potential savings all play a role. Different models and scenarios will produce different results. Historical data and current trends are vital to developing accurate estimations.
Factors Influencing Costs
Several key factors influence the projected costs of a “Medicaid for All” system. These include the current overall cost of healthcare in the nation, which is substantial, and administrative overhead, which will vary depending on the chosen model. Furthermore, the cost of expanding coverage to the uninsured will add to the financial burden. Potential savings, like reduced emergency room utilization and improved preventative care, are also significant considerations.
Comparison to Other Models
Comparing “Medicaid for All” to existing healthcare financing models, like the current system or a single-payer system, provides valuable context. Direct comparisons between models can help identify potential differences in cost structures and overall impact on taxpayers. For instance, a comprehensive comparison might highlight differences in administrative efficiency and the potential for reduced duplication of services. This comparison also provides a basis for evaluating potential savings and the financial impact on taxpayers.
Such comparisons help illustrate the complexities and potential trade-offs associated with various models.
Potential Tax Burdens
The potential impact on tax burdens is a critical concern. A “Medicaid for All” system will require substantial funding, likely resulting in changes to current tax policies or the introduction of new revenue streams. The precise amount of increased taxes or other financial burdens on individuals will depend on the chosen funding mechanisms. The potential for increased tax burdens or new tax policies needs to be thoroughly examined.
This also includes evaluating how potential changes in tax burdens might affect different socioeconomic groups. For instance, if new taxes are implemented, it’s crucial to consider how they will impact low-income individuals.
Demographic Cost Projections
| Demographic | Potential Cost | Explanation |
|---|---|---|
| Age (under 18) | Estimated lower cost per capita | Preventive care and lower medical needs are typical in younger populations. |
| Age (18-64) | Estimated higher cost per capita | This demographic typically has more complex medical needs and higher utilization rates. |
| Age (65+) | Estimated higher cost per capita | Higher rates of chronic conditions and associated medical expenses are expected. |
| Low-income | Estimated lower cost per capita | Potentially significant savings from reduced out-of-pocket expenses and increased preventative care. |
| Middle-income | Estimated moderate cost per capita | The impact on this group is a balancing act between costs and potential savings. |
| High-income | Estimated lower cost per capita | Potential savings from decreased uncompensated care and greater access to preventative care. |
| Individuals with pre-existing conditions | Estimated higher cost per capita | These individuals often have higher healthcare needs and associated costs. |
This table provides a general illustration of potential cost projections. Actual figures will vary based on numerous factors, and ongoing research is necessary to refine these projections.
Revenue Streams
A “Medicaid for All” system requires significant funding. Potential revenue streams could include increased taxes, such as a new healthcare tax or adjustments to existing taxes, or other innovative financial strategies. It is crucial to analyze different revenue streams to evaluate their potential impact on the economy and different socioeconomic groups. Furthermore, an assessment of the sustainability of these revenue streams is necessary to determine the long-term viability of the system.
Administrative and Operational Challenges
Implementing a “Medicaid for All” system presents significant administrative and operational hurdles, requiring careful planning and execution to ensure seamless service delivery. These challenges, while formidable, are not insurmountable. A well-structured approach can streamline processes and leverage existing infrastructure to create a robust and efficient system. Addressing these challenges head-on is crucial for ensuring equitable access to healthcare for all citizens.
Expanding Eligibility
Successfully expanding Medicaid eligibility to all citizens necessitates a comprehensive approach that involves streamlining the application process and ensuring accurate data collection. A simplified application form, accessible through various channels (online, in-person, phone), will be critical to ease the burden on applicants. Furthermore, robust data validation and verification systems are essential to prevent fraud and ensure accurate eligibility determinations.
Real-world examples from states with expanded Medicaid programs highlight the importance of these systems. For instance, some states have seen an increase in enrollment and have developed robust systems for managing the influx of new enrollees.
Managing Enrollment
Managing the enrollment of a vastly expanded population requires an efficient and user-friendly system. A centralized enrollment platform, integrated with existing databases, can facilitate seamless transitions and prevent duplication of efforts. This platform should be accessible across various channels, including mobile devices, ensuring accessibility for all. Moreover, the system must allow for ongoing updates to eligibility status, preventing unnecessary delays or disruptions in service.
The design should also accommodate various languages and cultural needs to ensure inclusivity.
Coordinating Care
Effective coordination of care is crucial for maintaining the quality and continuity of healthcare services. A system-wide electronic health record (EHR) system can help facilitate communication between providers and ensure a holistic view of patient care. This would allow for better communication and reduced duplication of services. Furthermore, establishing clear referral pathways and guidelines can help streamline transitions between providers and ensure continuity of care.
Examples of successful interoperability projects between different healthcare systems can provide valuable insights for implementing similar solutions.
Streamlining Processes and Improving Efficiency
Streamlining processes and improving efficiency are essential for the long-term sustainability of a “Medicaid for All” system. Leveraging technology to automate tasks such as eligibility verification and claim processing can reduce administrative burdens and free up resources for patient care. Implementing standardized protocols and procedures can enhance efficiency and reduce errors. Furthermore, the use of data analytics can help identify areas for improvement and optimize resource allocation.
Thinking about Medicaid for all? It’s a fascinating concept, but the recent spike in measles cases, like why this could be the worst year for measles in a decade , raises some serious questions about the health infrastructure needed to support such a system. Could it actually work, or are we overlooking some crucial elements? It’s a complex puzzle, and one that needs careful consideration before we start building.
Potential Solutions to Mitigate Challenges
Addressing the distribution and management of resources requires a multi-pronged approach. Investing in advanced technology and robust infrastructure can help improve efficiency and reduce costs. Training and development programs for healthcare providers and administrators are crucial for ensuring smooth transitions and minimizing errors. Developing clear protocols and guidelines for resource allocation can prevent unnecessary delays and improve service delivery.
Thinking about Medicaid for all? It’s a complex issue, and while there are hurdles to overcome, it’s worth considering the long-term health benefits. For example, choosing healthy habits early, like avoiding excessive drinking and smoking when young, can significantly impact your overall health, including the health of your heart. Drinking and smoking when young can prematurely age your heart.
Ultimately, ensuring access to preventative care through a system like Medicaid for all could potentially lead to a healthier, more resilient population.
Integration Strategies with Existing Healthcare Systems
Integrating “Medicaid for All” with existing healthcare systems requires a phased approach. A phased implementation, starting with pilot programs in specific regions or communities, can help identify potential challenges and refine the system before a broader rollout. Developing clear communication channels and collaboration mechanisms between different stakeholders, including providers, administrators, and patients, can help ensure smooth integration. A collaborative approach, engaging all stakeholders in the planning and implementation process, can help overcome challenges and ensure successful integration.
Potential Benefits and Outcomes: Could Medicaid For All Actually Work
A “Medicaid for All” system, while complex, promises significant benefits for individuals and society. It’s not just about access to healthcare; it’s about improving overall well-being, reducing disparities, and boosting economic productivity. This section explores the potential positive impacts of such a system.
Improved Health Outcomes
Universal access to healthcare, a cornerstone of a “Medicaid for All” system, is anticipated to lead to improved health outcomes across the population. This includes earlier diagnoses and treatments, potentially preventing chronic conditions and mitigating their severity. The elimination of financial barriers to care will encourage individuals to seek preventive care, fostering healthier lifestyles and better overall well-being.
Studies from countries with universal healthcare systems show a positive correlation between access and health outcomes.
Reduced Healthcare Disparities
Current healthcare systems often exacerbate existing disparities, with marginalized communities facing disproportionate barriers to accessing care. A “Medicaid for All” system aims to address these disparities by ensuring everyone has equal access to quality care, regardless of socioeconomic status, race, or ethnicity. This equitable access is crucial for promoting health equity and closing the health gap. Historically disadvantaged groups will experience significant gains in health outcomes.
Increased Economic Productivity
Improved health outcomes directly translate into increased economic productivity. When individuals are healthier, they are more likely to participate fully in the workforce, contributing more to the economy. Reduced absenteeism due to illness and enhanced cognitive function will boost productivity across various sectors. The potential increase in labor participation is a significant economic benefit, contributing to a stronger overall economy.
Impact on Workforce Participation
The link between health and workforce participation is undeniable. A healthier population is more likely to participate in the workforce, contributing to the economy. “Medicaid for All” systems are projected to increase the workforce participation rate, especially among individuals who previously faced barriers to employment due to lack of health insurance or inadequate access to care.
Comparison to the Status Quo
| Factor | Status Quo | Medicaid for All |
|---|---|---|
| Health Outcomes | Significant disparities in health outcomes based on socioeconomic status and access to care. | Improved health outcomes across the population, reducing disparities. |
| Healthcare Disparities | Marginalized communities face disproportionate barriers to care. | Reduced healthcare disparities through equitable access to quality care. |
| Economic Productivity | Reduced productivity due to illness and healthcare-related financial burdens. | Increased economic productivity through a healthier and more engaged workforce. |
| Workforce Participation | Lower workforce participation rates among those without insurance or adequate access to care. | Increased workforce participation rates due to improved health and reduced financial burdens. |
Evidence from Other Countries
Several countries with universal healthcare systems have demonstrated the positive impacts of such systems. Canada, for example, has shown improvements in life expectancy and reduced infant mortality rates. Other countries, such as the UK and Germany, have also seen improvements in health outcomes and reduced healthcare disparities. This evidence underscores the potential benefits of a “Medicaid for All” system in the United States.
Robust data from these examples illustrates the correlation between universal healthcare and positive outcomes.
Equity and Access Considerations
A “Medicaid for All” system, while promising universal access to healthcare, necessitates careful consideration of equity and access for diverse demographic groups. Ignoring historical disparities in healthcare access and outcomes could perpetuate existing inequalities, potentially undermining the system’s overall effectiveness and creating new challenges. This section delves into the potential impact on various groups, potential disparities, and strategies for ensuring equitable access.
Potential Impact on Demographic Groups, Could medicaid for all actually work
The potential impact of a “Medicaid for All” system will vary significantly across different demographic groups. Racial and ethnic minorities, low-income individuals, and people with disabilities often face systemic barriers to healthcare access, including implicit bias in the healthcare system, lack of culturally competent care, and financial constraints. A well-designed system would actively address these disparities to ensure equitable access to quality care.
Potential Disparities and Strategies for Equitable Access
Potential disparities may arise from variations in healthcare needs, access to transportation, language barriers, and cultural sensitivities. To ensure equitable access, the system needs to proactively address these factors. This could include culturally competent healthcare providers, translation services, transportation assistance programs, and community health workers who can bridge cultural gaps and address specific needs. Financial assistance programs can also help reduce the financial burden on low-income individuals and families.
Strategies to Address Historical and Existing Disparities
Addressing historical and existing disparities requires a multi-pronged approach. Implementing culturally competent training programs for healthcare professionals can help mitigate implicit bias. Dedicated resources for underserved communities, including community health centers and mobile clinics, can improve access to care. The system should actively involve communities in the design and implementation of programs, ensuring that solutions are tailored to their specific needs and preferences.
For example, providing resources for language access services and culturally sensitive materials in multiple languages can improve health literacy and engagement.
Ongoing Monitoring and Evaluation
Ongoing monitoring and evaluation are crucial to identify and address emerging inequities. This includes tracking disparities in access to care, treatment outcomes, and health outcomes among different demographic groups. Regular data collection and analysis will allow for the identification of areas where the system is not functioning equitably and the implementation of targeted interventions to address those specific issues.
This proactive approach ensures the system evolves to meet the needs of all populations, rather than simply perpetuating existing inequalities. Regular surveys and feedback mechanisms from patients can provide valuable insights into the experiences of different groups, and provide early warning signals of potential disparities.
Potential Impact on Healthcare Providers
A “Medicaid for All” system would fundamentally reshape the healthcare landscape, presenting both challenges and opportunities for providers. The shift from a largely fee-for-service model to one emphasizing preventative care and comprehensive coverage would necessitate adjustments across the board. This will require a careful consideration of the potential ramifications for reimbursement structures, operational efficiency, and the overall quality of care.
Thinking about Medicaid for all? It’s a complex issue, and while it could potentially revolutionize healthcare access, there are hurdles to overcome. A new app, like the new app helps type 2 diabetes community , shows how innovative solutions can target specific health needs, potentially providing valuable lessons for broader healthcare reform. Ultimately, the success of Medicaid for all depends on careful planning and implementation.
Reimbursement Rate Changes
The current fee-for-service system often incentivizes volume over value. A Medicaid for All system, focusing on comprehensive care and preventative measures, might reduce the emphasis on high-volume, low-complexity procedures. This could lead to a significant shift in reimbursement rates, potentially impacting hospitals and physicians who rely on these services for revenue. For instance, if preventative care and chronic disease management become more central, reimbursement for primary care physicians could increase while rates for specialized, high-cost procedures could decrease.
Transitioning to value-based care models, where payment is tied to patient outcomes and health improvements, would be crucial.
Service Demands and Staffing Needs
A significant increase in the insured population under a Medicaid for All system would undoubtedly place greater demands on healthcare services. This would likely require an increase in the number of primary care physicians, mental health professionals, and other specialists. Hospitals might need to expand capacity, potentially through new facilities or increased bed availability. Furthermore, the growing demand for telehealth services would necessitate investment in infrastructure and staff training.
Changes to the Healthcare Provider Landscape
The current landscape, often characterized by competition and profit-driven incentives, could undergo a transformation. Hospitals and clinics may need to re-evaluate their service offerings, potentially shifting toward community-based health centers and preventive care programs. Integration with existing community health programs and collaborations with public health agencies would become crucial. A move away from individualistic practice models toward team-based care models could also be seen.
Altered Business Models
The current business models of healthcare providers, often based on high-volume, fee-for-service structures, would need significant adaptation. This transition might involve incorporating alternative payment models, such as capitation, where providers are paid a fixed amount per patient per period. Collaboration and coordination among providers, particularly in the area of primary care, will be crucial for ensuring efficient and effective care delivery.
Long-Term Sustainability
A “Medicaid for All” system, while promising significant improvements in healthcare access and equity, faces substantial long-term challenges. Sustaining such a comprehensive program requires careful consideration of evolving healthcare costs, technological advancements, and the potential for public support to remain strong. Adaptability and foresight are crucial to ensure the system’s viability over time.The long-term financial viability of a Medicaid for All system hinges on effective cost management and innovative funding strategies.
The program’s success hinges on the ability to anticipate and address future healthcare demands and the ongoing evolution of healthcare technologies.
Potential Future Challenges
Maintaining affordability and accessibility in the face of rising healthcare costs is a primary concern. Technological advancements, such as new treatments and procedures, often come with increased costs, and the healthcare system must adapt to these changes. Furthermore, the demographics of the population, including the aging population and chronic disease prevalence, can influence healthcare costs. Adapting to these demographic shifts is a critical component of long-term sustainability.
Adapting to Evolving Healthcare Needs
The healthcare landscape is constantly changing, with new technologies and treatment approaches emerging regularly. A Medicaid for All system must be flexible enough to integrate these advancements while controlling costs. This could involve incentivizing the adoption of cost-effective technologies, supporting research into innovative treatments, and ensuring that healthcare providers are equipped to handle these new procedures. The system needs to be responsive to the evolving needs of the population and stay ahead of the curve in healthcare technology.
Maintaining Financial Viability
Implementing cost-containment measures is essential. This could include negotiating lower drug prices, promoting preventative care, and improving the efficiency of administrative processes. Exploring alternative funding models, such as increased taxes or expanding the pool of contributors, could provide additional revenue streams. Government transparency and accountability are crucial to maintaining public trust in the system’s financial management.
Importance of Ongoing Policy Adjustments
Regular evaluation and adjustments to policies are vital. The system must be able to respond to changing economic conditions, healthcare costs, and technological advancements. Ongoing policy refinement and modifications, based on feedback and performance data, are crucial to ensure the system’s long-term viability. Adapting to the evolving needs of the population and the healthcare industry will ensure the program’s enduring success.
A flexible framework is needed to address unexpected challenges and leverage opportunities for improvement.
Last Recap
Ultimately, the feasibility of “Medicaid for All” hinges on a delicate balance between ambitious goals and pragmatic realities. While the potential benefits, such as improved health outcomes and reduced disparities, are compelling, the financial, administrative, and operational hurdles are substantial. The long-term sustainability of such a system remains a crucial question that must be addressed. The discussion highlights the critical need for comprehensive planning, careful consideration of potential challenges, and proactive strategies to address concerns and maximize the potential benefits of such a sweeping change to the healthcare system.