Depression after heart attack is a significant concern for many survivors. This often-overlooked aspect of cardiac recovery impacts emotional well-being, affecting everything from daily routines to relationships. Understanding the complex interplay between physical and mental health is crucial for effective treatment and support.
This article explores the multifaceted nature of depression following a heart attack. We’ll delve into the underlying mechanisms, identify common symptoms, examine risk factors, and discuss various treatment approaches, ultimately emphasizing the importance of holistic care and support systems.
Understanding the Link Between Heart Attack and Depression
A heart attack is a life-altering event, and the emotional toll can be profound. The experience often leads to a range of psychological responses, including depression, that may need professional attention. This can significantly impact recovery and long-term well-being. The link between a heart attack and depression is complex, stemming from both physiological and psychological factors.The physiological impact of a heart attack can directly influence the development of depression.
The stress response triggered during and after a heart attack can lead to hormonal imbalances, including elevated cortisol levels. These changes can affect mood regulation and increase vulnerability to depressive symptoms. Furthermore, the physical pain, limitations, and potential for future health complications can significantly impact a person’s sense of self-worth and ability to function. This can be a catalyst for feelings of sadness, hopelessness, and despair.
Physiological Mechanisms of Depression After a Heart Attack
Heart attacks can trigger a cascade of physiological changes that increase the risk of depression. Inflammation, a natural response to injury, can also affect mood and contribute to depressive symptoms. Furthermore, hormonal imbalances, like changes in cortisol and other stress hormones, can disrupt the delicate balance of neurotransmitters in the brain, affecting mood regulation. These physiological responses can interact with pre-existing vulnerabilities, exacerbating the risk of depression.
Psychological Factors Contributing to Depression
Fear of recurrence, loss of function, and social isolation are significant psychological factors that contribute to depression following a heart attack. The fear of another heart attack can lead to anxiety, worry, and avoidance behaviors, impacting daily life. Loss of function, such as reduced physical activity or difficulty performing daily tasks, can lead to feelings of helplessness and decreased self-esteem.
Social isolation, due to limitations in physical activity or fear of burdening others, can further contribute to feelings of loneliness and despair.
The Role of PTSD and Depression Overlap
The experience of a heart attack can be profoundly traumatic, and the emotional distress associated with it can overlap with post-traumatic stress disorder (PTSD). PTSD is characterized by intrusive thoughts, flashbacks, and avoidance behaviors, all of which can be present in individuals experiencing depression after a heart attack. Individuals may experience significant emotional distress related to the event, leading to anxiety, fear, and difficulty coping.
The overlap between PTSD and depression in this context necessitates a comprehensive approach to treatment, addressing both the psychological trauma and depressive symptoms.
Factors Influencing Depression After a Heart Attack
| Factor | Mechanism | Symptoms | Management Strategies |
|---|---|---|---|
| Fear of Recurrence | Anxiety, worry, avoidance behaviors | Sleep disturbances, irritability, difficulty concentrating | Cognitive Behavioral Therapy (CBT), relaxation techniques, support groups |
| Loss of Function | Helplessness, decreased self-esteem, reduced self-efficacy | Loss of interest in activities, fatigue, feelings of worthlessness | Physical therapy, occupational therapy, support groups, medication (as needed) |
| Social Isolation | Loneliness, feelings of burden, social withdrawal | Withdrawal from social activities, sadness, feelings of isolation | Social support groups, counseling, encouraging social interaction |
| Inflammation and Hormonal Changes | Disruption of neurotransmitter balance, mood dysregulation | Irritability, changes in appetite, sleep disturbances | Anti-inflammatory medications (as needed), stress management techniques, healthy lifestyle changes |
Identifying Symptoms and Types of Depression
Navigating the emotional landscape after a heart attack can be challenging. Depression can arise as a reaction to the physical and psychological impact of the event, and it’s crucial to understand the nuanced ways it might manifest. Recognizing the symptoms and types of depression can help individuals and their loved ones seek appropriate support and treatment.Depression following a heart attack is not simply a continuation of pre-existing depressive tendencies.
Dealing with depression after a heart attack can be incredibly tough, but it’s not unique. Seeing how a Microsoft data scientist, after losing a newborn son, channeled their skills into tackling Sudden Infant Death Syndrome (SIDS) in this inspiring project really highlights the power of resilience and redirecting passion. It’s a reminder that even in the face of devastating loss, individuals can find ways to contribute positively, just like the impact a heart attack can have on an individual’s mental health.
Instead, it’s often a complex response to the significant life changes, fear, and uncertainty that accompany a major medical event. Symptoms may vary from person to person and can differ significantly from typical depressive episodes. This understanding is vital for accurate diagnosis and effective intervention.
Common Symptoms of Post-Heart Attack Depression
Understanding the potential symptoms of depression after a heart attack is key to early intervention. Common symptoms can include persistent sadness, feelings of hopelessness, and loss of interest in activities that were once enjoyable. Individuals might experience changes in appetite or sleep patterns, fatigue, and difficulty concentrating. These symptoms can impact daily life and overall well-being.
- Persistent sadness and hopelessness: This encompasses a profound sense of sadness that lingers and doesn’t seem to lift, often accompanied by feelings of hopelessness and despair about the future. This differs from the occasional sadness that is a normal human emotion.
- Loss of interest in activities: A noticeable decrease in interest in hobbies, social engagements, or previously enjoyed activities. This might involve withdrawing from loved ones or avoiding once-pleasurable pursuits.
- Changes in sleep and appetite: Significant shifts in sleep patterns, such as insomnia or excessive sleeping, and changes in appetite, either increased or decreased, are common indicators.
- Fatigue and lack of energy: A persistent feeling of tiredness and exhaustion, even with adequate rest, can signal a deeper underlying issue.
- Difficulty concentrating: Problems with focus, memory, and decision-making are frequently reported by individuals experiencing post-heart attack depression.
Less Common Symptoms of Post-Heart Attack Depression
While the above symptoms are common, depression after a heart attack can manifest in less typical ways. These less common symptoms can be subtle and may not be immediately recognized as indicators of depression.
Dealing with depression after a heart attack can be tough, especially when navigating the emotional rollercoaster. It’s important to remember that you’re not alone, and seeking support is crucial. Recent news about the Fischer Price sleeper toy recall, which you can learn more about here , highlights how significant events can impact our well-being. This, in turn, emphasizes the need for a supportive network and proper mental healthcare during this difficult time.
The journey to recovery is unique, but focusing on positive steps and seeking professional guidance is key to managing this type of emotional challenge.
- Anxiety and irritability: Feelings of anxiety, restlessness, and irritability can be part of the emotional experience. These might be mistaken for other issues or not linked to the heart attack.
- Physical symptoms: Unexplained physical aches and pains, such as headaches or muscle tension, can accompany depression. These symptoms are often dismissed as unrelated or attributed to physical recovery from the heart attack itself.
- Withdrawal and isolation: Individuals might withdraw from social interactions and isolate themselves, further exacerbating their feelings of sadness and hopelessness.
- Difficulty with decision-making: Struggles with everyday decisions and an inability to make choices may suggest an underlying emotional issue.
Types of Depression and Their Potential Relationship to Heart Attack
Depression isn’t a single entity; various types exist. Understanding these types can help in identifying and addressing the specific needs of individuals experiencing depression after a heart attack.
- Major Depressive Disorder (MDD): Characterized by a persistent and pervasive low mood, loss of interest in activities, and significant impairment in daily functioning. A heart attack can trigger or exacerbate MDD, particularly if the individual has a pre-existing vulnerability to this condition.
- Persistent Depressive Disorder (PDD): Also known as dysthymia, this involves a chronic low mood that lasts for at least two years. A heart attack can act as a stressor, potentially intensifying or prolonging the symptoms of PDD in vulnerable individuals.
Comparison of Symptoms
| Symptom | Depression after Heart Attack | Typical Depression |
|---|---|---|
| Sadness | Profound, persistent, often linked to heart attack experience | Variable intensity, may be episodic |
| Loss of Interest | Often related to activities previously enjoyed, but impacted by heart attack | Broad range of activities affected |
| Sleep Changes | Disrupted sleep patterns may be related to stress and anxiety | Insomnia or hypersomnia common |
| Appetite Changes | Related to emotional state and potential impact on diet | Increased or decreased appetite |
| Fatigue | Exhaustion may be heightened by the physical and emotional toll | Feeling tired and lacking energy |
Risk Factors and Protective Factors
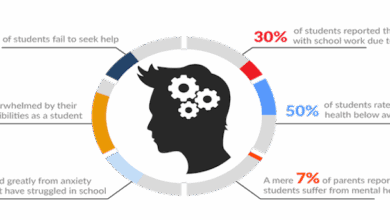
Post-heart attack depression is a significant concern, impacting recovery and overall well-being. Understanding the factors that contribute to its development, as well as those that can mitigate the risk, is crucial for proactive interventions and improved patient outcomes. This section delves into the interplay between various elements and their impact on the likelihood of experiencing depression after a heart attack.
Risk Factors Associated with Post-Heart Attack Depression
Several factors increase the vulnerability to depression following a heart attack. Recognizing these risk factors allows healthcare professionals and patients to proactively address potential challenges.
- Pre-existing mental health conditions: Individuals with a history of anxiety, depression, or other mental health issues are at a higher risk for developing depression after a heart attack. The stress and trauma associated with the heart attack can exacerbate pre-existing conditions, leading to a more severe depressive episode. For example, a patient with a history of mild anxiety may experience a significant increase in anxiety symptoms following a heart attack, potentially progressing to clinically significant depression.
- Social support: Inadequate social support systems can be a significant risk factor. Limited social connections and a lack of emotional or practical assistance can increase feelings of isolation and vulnerability, making individuals more susceptible to depression. A patient lacking a strong support network may struggle with emotional processing of the event and its implications, potentially leading to feelings of hopelessness and helplessness.
- Socioeconomic factors: Financial strain, lack of access to quality healthcare, and social isolation can contribute to depression risk. These factors can compound the stress of a heart attack, creating a difficult environment for emotional recovery. For example, a patient facing job loss or significant financial burdens following a heart attack might experience heightened stress, increasing the risk of depression.
Protective Factors Mitigating Post-Heart Attack Depression
Conversely, certain factors can help protect against post-heart attack depression. These protective factors are vital for promoting emotional well-being and facilitating a smoother recovery process.
Dealing with depression after a heart attack can be tough, and it’s important to remember you’re not alone. It’s a common struggle, often overlooked. Justin Baldoni, in his recent interview, interview with justin baldoni , discussed the importance of mental wellness, which resonates deeply with those navigating similar challenges. This emphasizes the need for open conversations and support systems for anyone facing depression following a heart attack.
- Strong social support networks: Robust social support systems provide crucial emotional and practical assistance during the recovery process. Family, friends, and community networks can offer encouragement, practical help, and a sense of belonging, reducing the isolation and stress associated with the heart attack. A patient with a strong support network is more likely to experience a sense of security and receive needed emotional and practical assistance.
- Access to quality healthcare: Comprehensive and supportive healthcare can significantly mitigate the risk of post-heart attack depression. Regular follow-up appointments, access to mental health services, and a supportive healthcare team can provide essential resources and guidance during recovery. A patient with access to quality healthcare and support services will have a higher likelihood of experiencing effective emotional recovery.
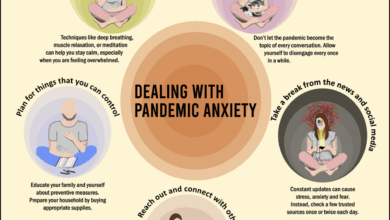
- Coping mechanisms: Developing and utilizing healthy coping mechanisms is crucial for managing stress and emotional distress. Techniques like mindfulness, relaxation exercises, and stress management strategies can significantly improve emotional resilience and reduce the risk of depression. A patient who employs healthy coping strategies is better equipped to manage the emotional challenges associated with a heart attack and its aftermath.
Impact of Lifestyle Choices on Depression Risk, Depression after heart attack
Lifestyle choices play a crucial role in the development of depression after a heart attack. Healthy choices can bolster resilience and emotional well-being.
- Diet: A balanced and nutritious diet rich in fruits, vegetables, and whole grains provides essential nutrients to support overall health and well-being. Nutritional deficiencies can contribute to feelings of fatigue and low mood, increasing vulnerability to depression. For example, a diet rich in antioxidants can support the body’s natural stress response, reducing the likelihood of experiencing a depressive episode.
- Exercise: Regular physical activity can improve mood, reduce stress, and promote overall emotional well-being. Exercise releases endorphins, which have mood-boosting effects, making it an effective tool in managing stress and depression. For instance, a patient who incorporates regular exercise into their routine will likely experience a more positive outlook and reduced feelings of sadness.
Risk Factors, Protective Factors, and Their Impact on Depression Risk
| Risk Factor | Protective Factor | Impact on Depression Risk |
|---|---|---|
| Pre-existing mental health conditions | Strong social support networks | Increases risk |
| Inadequate social support | Access to quality healthcare | Increases risk |
| Socioeconomic factors | Coping mechanisms | Increases risk |
| Unhealthy diet | Regular exercise | Increases risk |
Treatment Approaches and Strategies
Coping with depression after a heart attack requires a multifaceted approach that considers the unique needs of the individual. Effective treatment strategies encompass a range of interventions, from medication and psychotherapy to lifestyle modifications. A holistic and collaborative approach involving various healthcare professionals is crucial for optimal outcomes.A comprehensive treatment plan for post-heart attack depression is tailored to address the specific symptoms and underlying causes.
This personalized approach acknowledges the interplay between physical and emotional well-being, recognizing that the recovery journey is unique for each individual.
Medication
Medication plays a significant role in managing depressive symptoms following a heart attack. Selective serotonin reuptake inhibitors (SSRIs) are frequently prescribed due to their generally favorable safety profile in cardiovascular patients. However, careful consideration of potential drug interactions with existing medications for heart conditions is essential. The dosage and type of medication are determined by a psychiatrist in consultation with the cardiologist, based on the patient’s specific medical history and response to treatment.
Close monitoring of the patient’s condition during medication adjustments is vital to ensure safety and effectiveness.
Psychotherapy
Psychotherapy provides crucial support and tools for managing the emotional distress associated with depression. Cognitive Behavioral Therapy (CBT) is particularly effective in helping patients identify and modify negative thought patterns and behaviors that contribute to depression. Interpersonal Therapy (IPT) focuses on improving interpersonal relationships, which can be crucial for recovery and emotional well-being. These therapies are often delivered by psychologists or other mental health professionals in conjunction with other treatment approaches.
Lifestyle Interventions
Lifestyle changes can significantly impact the management of depression. Regular exercise, a balanced diet, and stress management techniques are essential components of a comprehensive treatment plan. These interventions can enhance physical and mental well-being, promoting overall recovery. Encouraging participation in support groups or joining a community that shares similar experiences can provide valuable social support and emotional resilience.
Multidisciplinary Approach
A collaborative approach involving cardiologists, psychiatrists, psychologists, and other healthcare professionals is paramount. This multidisciplinary team ensures that the patient receives coordinated care addressing both the physical and mental health aspects of their recovery. Cardiologists can monitor the patient’s overall health, while psychiatrists can prescribe and manage medications for depression. Psychologists provide therapy, focusing on cognitive and behavioral techniques.
The combined expertise of this team creates a supportive environment that optimizes treatment outcomes.
Treatment Options Table
| Treatment Option | Potential Benefits | Potential Drawbacks |
|---|---|---|
| Medication (e.g., SSRIs) | Effective in reducing depressive symptoms, often with a relatively quick onset of action. | Potential for side effects, including nausea, insomnia, and sexual dysfunction. May interact with other medications. Requires careful monitoring and adjustments by a psychiatrist. |
| Cognitive Behavioral Therapy (CBT) | Helps patients identify and challenge negative thought patterns, leading to improved mood and coping mechanisms. | Can be time-consuming, may not be suitable for all individuals, and requires active participation. |
| Interpersonal Therapy (IPT) | Addresses interpersonal issues contributing to depression, fostering healthier relationships. | May not be suitable for all individuals, may require time to see noticeable improvements, and requires active participation. |
| Lifestyle Interventions (exercise, diet, stress management) | Promotes overall physical and mental well-being, can complement other treatments. | Requires commitment and sustained effort, and may not be sufficient on its own for severe depression. |
Impact on Quality of Life
The aftermath of a heart attack can be profoundly challenging, and depression significantly exacerbates the struggle for a fulfilling life. Beyond the physical recovery, patients often face a cascade of emotional and social hurdles that diminish their overall quality of life. This section will delve into the multifaceted impact of post-heart attack depression, exploring its effects on daily activities, relationships, and long-term well-being.Depression following a heart attack can profoundly affect various aspects of a patient’s life, impacting their physical, emotional, and social well-being.
The emotional toll can lead to feelings of hopelessness, worthlessness, and isolation, hindering their ability to engage in activities they once enjoyed. These challenges can ripple through daily life, affecting everything from personal care to work performance and relationships.
Impact on Daily Activities
Depression can significantly hinder a patient’s ability to perform everyday tasks. Motivation and energy levels plummet, making even simple activities like showering, dressing, or preparing meals feel overwhelming. This reduced capacity to manage daily routines can create a vicious cycle, leading to feelings of helplessness and further exacerbating depressive symptoms. Individuals may withdraw from social interactions and hobbies, compounding the isolation and hindering their ability to engage in activities that could promote recovery and well-being.
Impact on Relationships
Depression can strain relationships with loved ones. Irritability, withdrawal, and difficulty communicating can lead to misunderstandings and conflicts. Patients might become withdrawn, neglecting their social connections, which further isolates them and intensifies their emotional distress. A lack of emotional support can impede the healing process and lead to long-term relationship challenges. For example, a patient who once enjoyed lively conversations might now struggle to engage in social gatherings, impacting their social network and creating distance from loved ones.
Impact on Work Performance
Depression can significantly affect work performance, even for individuals who were highly productive before the heart attack. Reduced concentration, difficulty focusing, and fatigue can make it challenging to complete tasks effectively. A decreased ability to engage with colleagues and manage work-related stress can further exacerbate the situation, leading to potential job loss or career setbacks. These consequences can create a significant financial and emotional burden, impacting the patient’s ability to cope with the aftermath of the heart attack.
Impact on Physical Health
Depression can negatively impact the physical recovery process after a heart attack. It can manifest as sleep disturbances, decreased appetite, and a weakened immune system, which hinders the healing process. The stress hormones released due to depression can further strain the cardiovascular system, potentially increasing the risk of future health problems. For instance, a patient might experience difficulty adhering to prescribed medication schedules or engaging in recommended physical activities, delaying their recovery and potentially jeopardizing their long-term health.
Long-Term Consequences of Untreated Depression
Untreated depression following a heart attack can have severe long-term consequences. It can lead to increased risk of recurrent heart problems, poorer physical health outcomes, and a diminished quality of life. The chronic stress associated with depression can place significant strain on the cardiovascular system, increasing the risk of complications. This cycle of depression and cardiovascular issues can be detrimental, impacting not only physical well-being but also emotional and social functioning.
A sustained lack of support and treatment can lead to long-term disability and significant financial burden on the individual and the healthcare system.
Table: Impact of Depression on Life After Heart Attack
| Aspect of Life | Impact of Depression |
|---|---|
| Daily Activities | Reduced motivation, difficulty completing tasks, decreased energy, withdrawal from routines |
| Relationships | Irritability, withdrawal, communication difficulties, social isolation, strained connections |
| Work Performance | Reduced concentration, difficulty focusing, fatigue, decreased productivity, potential job loss |
| Physical Health | Sleep disturbances, decreased appetite, weakened immune system, potential for increased risk of heart complications |
| Overall Well-being | Increased risk of recurrent heart problems, poorer physical health outcomes, diminished quality of life |
Support Systems and Resources

Navigating the emotional landscape after a heart attack can be challenging, especially when depression arises. A robust support system is crucial for recovery and well-being. It provides a network of understanding and encouragement, offering a lifeline during difficult times. This network helps patients feel less isolated and better equipped to cope with the physical and emotional aftermath of the event.A strong support system plays a vital role in managing depression after a heart attack.
The emotional and mental toll of this experience can be immense. Having supportive individuals to confide in, share experiences with, and receive encouragement from significantly improves a patient’s ability to heal. This network can help with practical tasks, emotional validation, and motivation to continue treatment.
Importance of Family and Friends
Family and friends often form the immediate and most accessible support network. Their understanding, empathy, and willingness to offer practical assistance are invaluable. Family members can provide emotional support, practical help with daily tasks, and encourage adherence to medical recommendations. Friends can offer companionship, shared activities, and a listening ear, reducing feelings of isolation. Open communication and a willingness to listen without judgment are key elements of this support.
Support Groups for Heart Conditions and Mental Health
Support groups specifically designed for individuals with heart conditions and mental health challenges can provide a unique and valuable resource. These groups offer a safe space for sharing experiences, coping strategies, and learning from others who understand the unique challenges faced. They allow patients to connect with peers who have firsthand knowledge of the emotional and psychological impact of a heart attack.
Sharing experiences and coping mechanisms can be incredibly beneficial for those struggling with depression.
Examples of Support Groups
Many hospitals and community organizations host support groups for heart patients. These groups may focus on specific aspects of recovery, such as adjusting to lifestyle changes or managing anxiety. Some groups may combine cardiac rehabilitation with mental health support, offering a comprehensive approach to recovery. Specific groups may be focused on those with depression after a heart attack.
Online forums dedicated to heart health can also be invaluable resources for connecting with others who understand the challenges of recovery.
Available Resources
A variety of resources are available to patients experiencing depression after a heart attack. Helplines provide immediate support and guidance during times of crisis, while online forums offer a space for ongoing discussion and connection. Community organizations often provide counseling, support groups, and educational programs tailored to patients’ needs. These resources are vital for navigating the emotional complexities of recovery and finding pathways to well-being.
Table of Resources for Support and Information
| Category | Examples |
|---|---|
| Helplines | National Suicide Prevention Lifeline, local crisis hotlines |
| Online Forums | Online forums for heart patients, mental health communities |
| Community Organizations | Local hospitals, cardiac rehabilitation centers, mental health associations |
| Support Groups | Heart attack survivors support groups, depression support groups |
| Professional Support | Therapists, counselors, psychiatrists specializing in cardiac patients |
Outcome Summary: Depression After Heart Attack

In conclusion, depression after a heart attack is a serious but manageable challenge. Recognizing the symptoms, understanding the contributing factors, and accessing appropriate treatment are vital steps toward recovery and a higher quality of life. Support networks, both formal and informal, play a critical role in navigating this complex experience.