Depression anxiety and ipf – Depression, anxiety, and IPF: a complex interplay where a progressive lung disease significantly impacts mental well-being. This exploration delves into the intricate connection between these conditions, examining symptoms, impacts, coping strategies, and treatment approaches. Understanding the shared challenges and unique experiences of those living with IPF and co-occurring mental health issues is crucial for effective support and care.
We’ll uncover the common symptoms of depression and anxiety, highlighting how they manifest differently in IPF patients. The unique psychological challenges of living with a progressive lung disease like IPF will be explored, along with the impact of fear, uncertainty, and treatment side effects. Ultimately, we’ll offer actionable strategies for managing mental health, including various support systems, relaxation techniques, and the role of therapy in holistic care.
Introduction to Depression, Anxiety, and IPF

Depression and anxiety are common mental health conditions affecting millions worldwide. They can significantly impact daily life, relationships, and overall well-being. Understanding these conditions is crucial, especially when considering their potential connection to other health issues. Idiopathic Pulmonary Fibrosis (IPF), a progressive lung disease, presents unique challenges, and its interplay with mental health deserves careful attention.This exploration delves into the overlap between these conditions, examining symptoms, shared risk factors, and potential physiological links.
The goal is to increase awareness and understanding of the complex relationship between mental and physical health in the context of IPF.
Overview of Depression and Anxiety
Depression and anxiety are distinct yet interconnected mental health conditions. Depression is characterized by persistent sadness, loss of interest, and feelings of hopelessness. Anxiety, on the other hand, involves excessive worry, fear, and physical tension. While they have different presentations, they can co-occur and significantly influence each other.
Common Symptoms of Depression and Anxiety
Depression often manifests in a constellation of symptoms including persistent sadness, loss of interest in activities, changes in appetite and sleep patterns, fatigue, feelings of worthlessness or guilt, difficulty concentrating, and recurrent thoughts of death or suicide. Anxiety symptoms can range from excessive worry and nervousness to physical sensations like rapid heartbeat, shortness of breath, and trembling. These symptoms can vary in intensity and duration, impacting daily functioning.
Connection Between Mental Health Conditions and IPF
Patients with IPF frequently experience co-occurring mental health conditions like depression and anxiety. The progressive nature of IPF, coupled with the physical limitations and potential for respiratory distress, creates significant psychological stress. The fear of the unknown, the limitations imposed by the disease, and the impact on quality of life can lead to these mental health challenges.
Shared Risk Factors Between IPF and Depression/Anxiety
Several risk factors are associated with both IPF and mental health conditions. Chronic illness, such as IPF, can lead to increased stress and anxiety. The uncertainty surrounding a progressive disease and the potential for future complications are significant stressors. Moreover, financial strain associated with medical expenses and potential loss of income can contribute to both IPF-related challenges and the development of mental health issues.
Potential Physiological Links Between IPF and Mental Health Conditions
The exact physiological mechanisms linking IPF to mental health conditions are not fully understood. However, inflammation, a key component in the progression of IPF, is also implicated in the development of some mental health conditions. Furthermore, the physical discomfort, shortness of breath, and fatigue associated with IPF can significantly impact mood and psychological well-being. There may also be a role for neuroendocrine factors and the immune system in this complex relationship.
Key Differences Between Depression and Anxiety Symptoms
| Characteristic | Depression | Anxiety | Examples |
|---|---|---|---|
| Mood | Persistent sadness, hopelessness, loss of interest | Excessive worry, nervousness, fear | Feeling constantly down, losing interest in hobbies; Excessive worry about future events, feeling dread. |
| Physical Symptoms | Fatigue, changes in appetite or sleep, loss of energy | Muscle tension, restlessness, rapid heartbeat, shortness of breath | Feeling constantly tired, significant weight loss or gain, trouble sleeping; Muscle aches, trembling, rapid heart rate. |
| Cognitive Symptoms | Difficulty concentrating, negative thoughts, feelings of worthlessness | Racing thoughts, intrusive thoughts, difficulty relaxing | Trouble focusing, dwelling on negative experiences, feeling inadequate; Constant racing thoughts, repetitive worries, difficulty calming down. |
| Behavioral Symptoms | Withdrawal from social activities, decreased motivation | Avoidance of feared situations, excessive reassurance-seeking | Isolation, reduced interest in socializing, decreased productivity; Avoiding certain places or people, seeking constant reassurance from others. |
Impact of IPF on Mental Health: Depression Anxiety And Ipf
Living with idiopathic pulmonary fibrosis (IPF) presents a unique set of challenges extending far beyond the physical limitations of the disease. The progressive nature of IPF, coupled with its impact on breathing and overall well-being, can significantly affect mental health. Understanding the psychological toll of IPF is crucial for both patients and healthcare providers to offer comprehensive support and improve quality of life.The psychological challenges associated with a progressive lung disease like IPF are multifaceted and often intertwined.
The constant awareness of the disease’s progression, the uncertainty about its future course, and the potential for reduced life expectancy can induce significant anxiety and fear. These emotional responses, combined with the physical symptoms, can create a vicious cycle that further diminishes mental well-being.
Psychological Challenges of IPF
IPF patients frequently experience a range of psychological distress. These include heightened levels of anxiety, depression, and feelings of isolation. The progressive nature of the disease and the associated decline in lung function can contribute to feelings of helplessness and hopelessness. The unpredictable nature of the disease and the potential for future exacerbations can fuel anxiety and fear.
Emotional and Social Consequences
The emotional and social consequences of living with IPF are significant. Patients may experience feelings of isolation due to their reduced ability to participate in social activities and maintain relationships. Changes in physical appearance and stamina can impact self-esteem and body image. These changes can affect social interactions and relationships, leading to feelings of isolation and loneliness.
Financial concerns, related to the cost of treatment and potential loss of income, further compound the emotional burden.
Fear and Uncertainty in IPF
Fear and uncertainty are significant contributors to depression and anxiety in IPF patients. The progressive nature of the disease and the lack of a cure create a constant sense of vulnerability and unpredictability. Patients may experience fear about the future, the impact on their loved ones, and the potential for worsening symptoms. The uncertainty surrounding the disease’s progression and its effects on daily life can lead to feelings of anxiety and stress.
Impact of Treatment Side Effects
Treatment for IPF can also have a significant impact on mental health. Certain medications used to manage IPF can cause side effects that affect mood, sleep, and energy levels. These side effects can further exacerbate existing mental health concerns and contribute to feelings of fatigue and hopelessness. It is important to acknowledge the role that these side effects play in the patient’s overall experience and to develop strategies to mitigate their impact.
Dealing with depression, anxiety, and IPF can be tough, especially during the holidays. Finding healthy ways to cope is key, and that’s where holiday self-care comes in. Exploring the soothing effects of warming holiday spices, like cinnamon and ginger, can be a wonderful addition to your routine. Check out this article on holiday spices for festive self care for some inspiring ideas.
These simple additions can make a real difference in managing those tough feelings, helping you navigate the holiday season with a bit more ease and focus, ultimately benefiting your overall health and well-being, especially when dealing with depression, anxiety, and IPF.
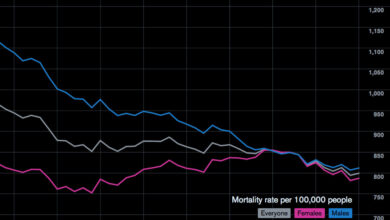
Demographic Differences in IPF Impact
The impact of IPF on mental health can vary based on demographic factors such as age and gender. Younger patients may experience more difficulty adjusting to the diagnosis and its implications for their future, while older patients may face challenges related to pre-existing mental health conditions and social isolation. Women may experience unique emotional responses due to the societal expectations and roles they fulfill.
However, further research is needed to fully understand the nuances of these demographic differences.
Emotional Responses to Stressors
| Stressor | IPF Patient Emotional Response | Healthy Individual Emotional Response | Comparison |
|---|---|---|---|
| Diagnosis of IPF | Fear, anxiety, denial, sadness | Shock, uncertainty, concern, worry | IPF patients experience a greater intensity of negative emotions, possibly due to the progressive and life-threatening nature of the disease. |
| Progressive decline in lung function | Hopelessness, helplessness, loss of control | Frustration, difficulty adapting, concern about future | IPF patients often experience a more profound sense of loss and a greater struggle with coping mechanisms. |
| Treatment side effects | Irritability, fatigue, sleep disturbances, mood changes | Potential for temporary discomfort, adjustments to lifestyle | IPF treatment side effects can significantly impact daily functioning and mental well-being. |
| Social isolation | Loneliness, isolation, decreased social engagement | Potential for temporary social withdrawal, adjustments in social circles | IPF patients may experience a more severe and prolonged sense of social isolation due to the limitations imposed by the disease. |
Coping Strategies and Support Systems
Living with Idiopathic Pulmonary Fibrosis (IPF) can significantly impact mental well-being, often leading to feelings of anxiety and depression. Understanding effective coping mechanisms and accessing supportive resources is crucial for managing these emotional challenges alongside the physical demands of IPF. This section explores practical strategies and valuable support systems to navigate the emotional landscape of this complex condition.
Effective Coping Mechanisms for Depression and Anxiety
Managing depression and anxiety is vital for individuals with IPF. A multifaceted approach encompassing various strategies is often most beneficial. These strategies can include regular exercise, maintaining a healthy diet, engaging in enjoyable activities, and prioritizing sufficient sleep. Mindfulness practices, such as meditation and deep breathing, can also be profoundly helpful in reducing stress and promoting emotional regulation.
Seeking professional help through therapy is also a valuable component of managing these conditions. Remember, seeking support is a sign of strength, not weakness.
Support Groups and Resources for IPF Patients
Numerous support groups and resources are available to provide comfort and guidance for IPF patients and their families. These groups offer a safe space for sharing experiences, receiving encouragement, and learning coping strategies from others facing similar challenges. Online forums, local support groups, and professional organizations dedicated to IPF can be invaluable sources of information and emotional support.
Practical Strategies for Stress Reduction and Emotional Regulation
Stress reduction techniques are essential for individuals with IPF. Implementing these techniques can significantly impact emotional well-being. Deep breathing exercises, progressive muscle relaxation, and guided imagery are powerful tools for calming the mind and body. Establishing a consistent daily routine, including regular sleep schedules and enjoyable activities, can also contribute to stress management. Creating a supportive and understanding environment within the home and social circle is crucial.
The Role of Therapy in Supporting Mental Well-being
Therapy can play a significant role in supporting the mental well-being of individuals with IPF. A therapist can provide a safe space to discuss emotional challenges, develop coping mechanisms, and address any underlying mental health concerns. Therapy can also offer strategies for managing stress, improving communication, and enhancing overall emotional regulation. It’s important to remember that therapy is a personalized process, and the specific benefits can vary based on individual needs and goals.
Examples of Support Groups and Their Potential Benefits
| Type of Support Group | Potential Benefits | Examples of Resources | Considerations |
|---|---|---|---|
| Online Forums | Anonymity, accessibility, 24/7 support, broad reach | IPF patient forums on social media or dedicated websites | Potential for impersonal interactions, lack of face-to-face connection |
| Local Support Groups | Face-to-face interaction, shared experiences, community building | Local hospitals, community centers, or patient advocacy groups | Limited accessibility, schedules might not align |
| Support Groups Led by Healthcare Professionals | Expert guidance, tailored support, structured sessions | Pulmonary clinics, rehabilitation centers | Potential cost or limited availability |
| Family Support Groups | Shared experience, emotional support for family members | Specialized support groups for caregivers or family members | Specific needs of family members may require tailored support |
Relaxation Techniques for Anxiety Reduction (Tailored for IPF)
Relaxation techniques can be particularly beneficial for individuals with IPF. These techniques can help to manage anxiety and improve overall well-being. Prioritizing gentle activities that don’t exacerbate lung function is key.
Dealing with depression, anxiety, and idiopathic pulmonary fibrosis (IPF) can be incredibly challenging. It’s important to stay informed about all aspects of health, especially when it comes to potential risks and preventative measures. For example, recent news about Zika’s limited travel potential in the USA ( zika wont travel far in usa ) might seem unrelated, but understanding the broader health landscape can help us better cope with our own struggles.
Ultimately, focusing on our own well-being and staying proactive in managing IPF and mental health is key.
- Deep Breathing Exercises: These techniques involve slow, deep inhalations and exhalations, promoting relaxation and reducing feelings of panic. Adjust breathing patterns to accommodate limitations caused by IPF.
- Progressive Muscle Relaxation: This involves systematically tensing and releasing different muscle groups, promoting physical and mental relaxation. Focus on gentle movements to avoid straining.
- Guided Imagery: This technique involves visualizing calming or peaceful scenes, promoting relaxation and reducing anxiety. Ensure imagery focuses on gentle, calming environments and sensations.
- Mindfulness Meditation: This involves focusing on the present moment, promoting awareness and reducing overthinking. Practice in short sessions, adjusting to limitations caused by IPF.
Treatment Approaches and Interventions
Living with Idiopathic Pulmonary Fibrosis (IPF) can be incredibly challenging, not just physically but also mentally. The relentless nature of the disease, coupled with the uncertainty of its progression, can lead to significant emotional distress. Understanding and addressing these emotional concerns is crucial for optimizing treatment outcomes and improving overall quality of life for IPF patients.Effective treatment for depression and anxiety in IPF patients requires a multifaceted approach that considers both the physical and mental aspects of the illness.
Medical interventions for IPF itself can have a profound impact on a patient’s mental well-being. For example, the side effects of certain medications or the progressive nature of the disease can exacerbate pre-existing anxiety or contribute to the development of depression. Therefore, a holistic approach to care, integrating mental health support with medical interventions, is essential for managing IPF patients effectively.
Medical Interventions and Their Impact on Mental Health
Medical interventions for IPF, such as medications to slow disease progression, oxygen therapy, and pulmonary rehabilitation, can have a complex interplay with a patient’s mental health. While these interventions are vital for managing the physical symptoms, they can also impact mood and emotional well-being. For example, the side effects of some medications, such as fatigue or changes in appetite, can trigger or worsen depressive symptoms.
Similarly, the progressive nature of the disease, and the uncertainty it brings about future health, can contribute to anxiety and stress.
Role of Mental Health Professionals
Mental health professionals, including psychologists, psychiatrists, and social workers, play a critical role in managing IPF patients. They can provide specialized support to address the unique emotional challenges faced by these patients. This includes helping patients cope with the diagnosis, manage stress and anxiety, and improve their overall emotional well-being. Furthermore, mental health professionals can help patients and their families navigate the complexities of IPF care, offering valuable insights and strategies for adapting to the disease’s impact on daily life.
Dealing with depression, anxiety, and Idiopathic Pulmonary Fibrosis (IPF) can be incredibly challenging. The search for effective treatments is ongoing, and recent advancements in regenerative medicine, such as those explored in regenerative medicine has bright future , offer a glimmer of hope. While there’s still a long road ahead, these promising avenues for treatment could significantly improve the lives of those affected by these conditions.
Holistic Approach to Care
A holistic approach to IPF care recognizes the interconnectedness of physical and mental health. This means integrating mental health support into the overall treatment plan, alongside standard medical interventions. This integration ensures that patients receive comprehensive care that addresses both their physical and emotional needs. For example, a treatment plan might include regular sessions with a therapist, coupled with medication management and pulmonary rehabilitation.
Integration of Mental Health Support into IPF Treatment Plans, Depression anxiety and ipf
Integrating mental health support into IPF treatment plans is essential for optimizing patient outcomes. This involves close collaboration between medical professionals and mental health specialists. For instance, a patient’s physician might recommend therapy sessions alongside prescribed medications for IPF, recognizing the potential for mental health conditions to influence adherence to treatment plans and overall quality of life.
Summary of Therapies
This table summarizes various types of therapies and their potential benefits for IPF patients:
| Therapy Type | Description | Potential Benefits | Considerations |
|---|---|---|---|
| Cognitive Behavioral Therapy (CBT) | Focuses on identifying and changing negative thought patterns and behaviors. | Improved mood regulation, reduced anxiety, enhanced coping skills. | Requires active participation and commitment from the patient. |
| Acceptance and Commitment Therapy (ACT) | Helps patients accept difficult emotions and commit to valued actions. | Increased resilience, improved emotional regulation, enhanced sense of purpose. | May require longer-term engagement and practice. |
| Mindfulness-Based Stress Reduction (MBSR) | Focuses on present moment awareness and relaxation techniques. | Reduced stress, improved emotional regulation, enhanced coping mechanisms. | Requires consistent practice and may benefit from group settings. |
| Support Groups | Provide a platform for sharing experiences and support with others facing similar challenges. | Increased social connection, reduced feelings of isolation, shared coping strategies. | Requires a safe and supportive environment, facilitated by a skilled leader. |
Understanding the Symptoms

Navigating the complexities of IPF often involves a delicate dance between physical and mental well-being. Recognizing the symptoms of depression and anxiety, particularly when intertwined with the physical manifestations of IPF, can be challenging for both patients and healthcare professionals. This crucial understanding empowers proactive intervention and ensures optimal care.Identifying depression and anxiety in IPF patients requires a nuanced approach, going beyond the typical presentation of these conditions in the general population.
The overlapping symptoms, often masked by the IPF’s own symptoms, can lead to misdiagnosis or delayed intervention. This section delves into the specific hurdles in diagnosis and highlights the importance of open communication.
Challenges in Identifying Depression and Anxiety in IPF
The overlapping symptoms of IPF and mental health conditions pose a significant diagnostic hurdle. Fatigue, shortness of breath, and chest pain, common IPF symptoms, can easily mimic the symptoms of depression and anxiety. This overlap can lead to a misdiagnosis or delay in treatment for both conditions.
Mimicking Symptoms of IPF and Mental Health Conditions
Physical symptoms of IPF can often mimic mental health symptoms. For example, fatigue associated with IPF can be indistinguishable from the fatigue of depression. Similarly, shortness of breath, a hallmark of IPF, can be misinterpreted as anxiety-induced hyperventilation. This ambiguity highlights the crucial role of a thorough medical history and physical examination to differentiate between the two.
Importance of Open Communication
Open and honest communication between patients and healthcare providers is paramount in accurately identifying and treating both IPF and associated mental health concerns. Patients should feel comfortable discussing any emotional or psychological distress, while healthcare providers should actively inquire about these issues during routine checkups. This collaborative approach fosters a supportive environment where concerns can be addressed promptly and effectively.
Comparison of Symptom Presentation
The presentation of depression and anxiety in IPF patients often differs from the typical presentation in the general population. Patients with IPF might exhibit symptoms like irritability, withdrawal, or difficulty concentrating, alongside their physical symptoms. The intensity and frequency of these symptoms can vary significantly from person to person, further complicating diagnosis.
Impact of Delayed Diagnosis
Delayed diagnosis of depression and anxiety in IPF patients can have significant negative consequences. Untreated mental health conditions can exacerbate physical symptoms, leading to decreased quality of life and potentially impacting treatment adherence for IPF. Early intervention, therefore, is critical for managing both conditions effectively.
Contrasting Symptoms of Depression
| Typical Symptom of Depression | Possible Masked Symptoms due to IPF | Example of Overlap | Diagnostic Considerations |
|---|---|---|---|
| Loss of interest or pleasure in activities | Fatigue and shortness of breath limiting activity | A patient loses interest in hobbies due to breathlessness and fatigue from IPF. | Careful evaluation of baseline activity levels and comparing them to prior levels to identify a change. |
| Changes in appetite or sleep | Appetite changes due to medication side effects or physical discomfort | A patient experiences decreased appetite due to nausea from IPF medication or pain. | Assessment of medication side effects, pain levels, and any recent changes in appetite or sleep patterns. |
| Feelings of worthlessness or guilt | Feelings of hopelessness and helplessness due to the prognosis of IPF. | A patient feels worthless due to the impact of IPF on their life and ability to participate in daily activities. | Differentiating between the impact of the disease and underlying feelings of worthlessness. |
| Difficulty concentrating or making decisions | Cognitive impairment due to hypoxia or medication side effects | A patient struggles to focus due to shortness of breath or medication. | Evaluation of cognitive function and consideration of potential underlying causes. |
Long-Term Management and Prognosis
Living with idiopathic pulmonary fibrosis (IPF) presents unique challenges, extending beyond the physical limitations of the disease. The impact on mental health, including depression and anxiety, requires ongoing attention and proactive management. Understanding the long-term implications and factors influencing prognosis is crucial for patients and their support systems.Maintaining a positive outlook and coping effectively with the progressive nature of IPF are essential aspects of long-term well-being.
A comprehensive approach to management necessitates addressing the psychological dimensions of the disease alongside the physical. This involves not only recognizing the symptoms but also fostering resilience and a supportive environment.
Importance of Long-Term Mental Health Monitoring
Regular monitoring of mental health is paramount for IPF patients. This involves ongoing assessments to identify and address emerging emotional challenges. Early intervention for depression or anxiety can prevent their escalation and significantly improve quality of life. Consistent communication with healthcare providers about mood changes, stress levels, and coping mechanisms is vital. This proactive approach allows for timely adjustments to treatment plans and supports.
Strategies for Maintaining Well-being Over Time
Sustaining well-being requires a multi-faceted approach. Adopting healthy lifestyle choices, including a balanced diet, regular exercise (as tolerated), and adequate sleep, can contribute significantly to emotional stability. Engaging in activities that promote relaxation, such as meditation, yoga, or spending time in nature, can also be beneficial. Building a strong support network, including family, friends, and support groups, is critical for emotional well-being and shared experiences.
Factors Influencing Prognosis
Several factors influence the prognosis of IPF patients, with mental health playing a crucial role. The severity of lung function impairment, the presence of co-occurring conditions (like depression and anxiety), and adherence to treatment plans are key factors. Additionally, the patient’s coping mechanisms, social support, and overall psychological resilience significantly impact the long-term trajectory of the disease. Studies have shown that individuals with strong support systems and effective coping strategies often have a more favorable prognosis.
Strategies for Long-Term Support
A robust support system is essential for IPF patients with co-occurring depression and anxiety. This includes:
- Regular therapy sessions with a mental health professional, providing a safe space for emotional processing and developing coping mechanisms.
- Support groups specifically designed for IPF patients, offering a platform for sharing experiences, providing encouragement, and reducing feelings of isolation.
- Access to educational resources about IPF and its impact on mental health, empowering patients with knowledge and reducing anxieties about the future.
- Encouraging open communication within families and with healthcare teams to address concerns and anxieties.
- Exploring complementary therapies like mindfulness or art therapy, which can aid in stress reduction and emotional regulation.
Lifestyle Changes for Mental Well-being
Lifestyle changes can significantly improve mental well-being in IPF patients. Examples include:
- Adopting a balanced diet rich in fruits, vegetables, and whole grains to provide essential nutrients and maintain energy levels.
- Engaging in regular physical activity, tailored to individual abilities and limitations, to improve mood and reduce stress. Walking, gentle exercises, or water therapy can be helpful.
- Prioritizing sufficient sleep to allow the body and mind to rest and recover, promoting overall well-being.
- Establishing a daily routine to maintain a sense of structure and control, reducing feelings of uncertainty and anxiety.
- Seeking out hobbies and activities that bring joy and fulfillment, like reading, listening to music, or spending time in nature, to foster positive emotions and distract from anxieties.
Last Recap
In conclusion, depression, anxiety, and IPF are deeply intertwined. The impact of IPF on mental well-being is substantial, demanding a holistic approach to care. We’ve examined the symptoms, challenges, and potential solutions. Recognizing the importance of early intervention, open communication, and tailored support systems is key to improving the lives of those facing these conditions. This exploration underscores the need for a comprehensive understanding of the interconnectedness of physical and mental health in the context of IPF.