Depression treatment how genetic testing can help find the right medication – Depression treatment: how genetic testing can help find the right medication. This innovative approach to mental health care promises a more personalized and effective treatment path for individuals struggling with depression. By analyzing an individual’s genetic makeup, we can identify predispositions and potential responses to various antidepressant medications. This knowledge empowers doctors to tailor treatment plans, potentially minimizing trial-and-error and side effects.
This exploration delves into the science behind genetic testing in depression treatment, examining the role of genes in medication response, the complexities of gene-environment interactions, and the ethical considerations surrounding this emerging field. We’ll also look at real-world case studies to illustrate how genetic information can be used to optimize treatment strategies.
Introduction to Depression Treatment and Genetic Factors
Depression, a pervasive mental health condition, significantly impacts millions worldwide. It’s characterized by persistent sadness, loss of interest in activities, changes in sleep and appetite, and feelings of hopelessness. This widespread affliction profoundly affects individuals’ daily lives, relationships, and overall well-being. The impact extends beyond the individual, impacting families and communities.Genetic factors play a crucial role in both the development and response to depression treatment.
While environmental factors undoubtedly contribute, inherited predispositions can influence an individual’s vulnerability to experiencing depressive episodes. Understanding the interplay of genes and environment is essential for developing personalized treatment strategies. The complex interaction between genes and life experiences, known as gene-environment interaction, makes predicting an individual’s response to treatment challenging. This is where genetic testing can offer valuable insights.
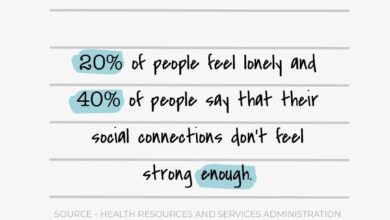
Prevalence and Impact of Depression
The global prevalence of depression underscores its significant impact on public health. Studies consistently show a substantial portion of the population experiences depressive episodes at some point in their lives. This prevalence highlights the urgent need for effective prevention and treatment strategies. The impact of depression extends beyond the individual, affecting their families, careers, and relationships.
The Role of Genetics in Depression
Genetic predisposition is a crucial factor in depression. Certain genes influence neurotransmitter systems and brain structure, potentially increasing susceptibility to the condition. The genetic basis for depression is multifaceted, involving numerous genes and complex interactions. While no single gene directly causes depression, inherited factors contribute to an individual’s risk.
Gene-Environment Interactions in Depression
The interaction between genetic predisposition and environmental factors is crucial in understanding depression. Environmental stressors, such as trauma, abuse, or significant life events, can trigger depressive episodes in individuals with a genetic predisposition. This intricate interplay emphasizes the importance of considering both genetic and environmental influences when developing personalized treatment plans. For example, an individual with a genetic predisposition might experience a depressive episode after a stressful life event, while another individual without the genetic predisposition might not.
Types of Genetic Testing in Medicine
Various types of genetic testing are utilized in medicine, each with unique applications and limitations. These tests can provide insights into an individual’s genetic makeup, helping to identify potential health risks and tailor treatment strategies. The increasing accessibility of genetic testing has led to a wider range of applications in various medical fields.
Comparison of Genetic Testing Types
| Type | Process | Accuracy | Cost | Limitations |
|---|---|---|---|---|
| Genome-wide association studies (GWAS) | Analyze variations across the entire genome to identify associations with a specific trait (e.g., depression). | High, but associations are often weak. | Moderate to high. | Limited ability to pinpoint specific genes; often requires large sample sizes. |
| Gene sequencing | Determine the precise order of DNA bases in a gene or genes. | High. | High. | Can be expensive and may not identify all relevant genes. |
| Pharmacogenetic testing | Identify variations in genes that influence drug metabolism and response. | Moderate to high, depending on the specific gene. | Moderate. | May not predict response to all medications; requires clinical interpretation. |
This table provides a comparative overview of different genetic testing methods. Each approach has unique strengths and weaknesses, influencing its suitability for specific applications. The choice of testing method depends on the specific clinical question and resources available.
Genetic Markers and Medication Response
Understanding how your genes interact with antidepressants is crucial for personalized treatment. While many factors influence a person’s response to medication, genetic variations play a significant role in how the body metabolizes and reacts to different drugs. This knowledge allows for a more targeted approach, potentially leading to more effective treatment and fewer side effects.Genetic testing can help identify variations in your genes that might influence your response to different antidepressants.
This information can be used to tailor your treatment plan, selecting the most effective medication and dosage for your individual needs. By understanding how your genes impact the effectiveness of various antidepressants, doctors can optimize treatment strategies and potentially reduce the trial-and-error process often associated with finding the right medication.
Genetic Variations and Antidepressant Metabolism
Genetic variations can affect the enzymes responsible for metabolizing antidepressants. Variations in these genes can alter how quickly or slowly the body breaks down a medication. This, in turn, impacts the concentration of the drug in the bloodstream and, ultimately, its effectiveness. For instance, if a gene variant leads to slower metabolism, the medication may stay in the system longer, potentially increasing the risk of side effects.
Conversely, faster metabolism may result in the medication not staying in the system long enough to be effective.
Specific Genes and Their Potential Impact
Several genes have been identified as potentially influencing antidepressant response. One example is the CYP2D6 gene, which plays a key role in metabolizing many antidepressants, including selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants. Variations in this gene can significantly affect the breakdown rate of these medications. Another important gene is the SLC6A4 gene, which codes for the serotonin transporter protein.
Variations in this gene could affect the amount of serotonin available in the brain, influencing the effectiveness of SSRIs. Furthermore, variations in genes involved in neurotransmitter pathways, such as the serotonin and norepinephrine transporters, could influence the body’s response to specific medications.
Pharmacogenomics in Depression Treatment
Pharmacogenomics is the study of how genes affect a person’s response to medication. In depression treatment, pharmacogenomics aims to use genetic information to predict which antidepressant medications are most likely to be effective for an individual and to identify potential side effects. This personalized approach to treatment can lead to faster and more effective treatment outcomes. It’s important to remember that genetic variations are just one piece of the puzzle in determining medication response.
Other factors, such as age, lifestyle, and co-occurring conditions, also play a significant role.
Potential Interactions Between Genetic Variations and Antidepressant Medications
| Gene | Variation | Medication | Expected Response | Potential Side Effects |
|---|---|---|---|---|
| CYP2D6 | Poor Metabolizer | Fluoxetine (Prozac) | Increased risk of adverse effects due to higher drug concentration. | Nausea, dizziness, serotonin syndrome |
| CYP2D6 | Ultra-Rapid Metabolizer | Paroxetine (Paxil) | Medication may not reach therapeutic levels, requiring higher doses or alternative medications. | Less pronounced or absent therapeutic effect. |
| SLC6A4 | Specific Variation | Sertraline (Zoloft) | Potentially altered serotonin levels, influencing effectiveness and side effects. | Potential for serotonin syndrome or other serotonin-related issues. |
| COMT | Val60Met | Venlafaxine (Effexor) | Possible reduced effectiveness due to altered dopamine metabolism. | Potential for reduced mood improvement. |
Note: This table is for illustrative purposes only and does not represent an exhaustive list. Individual responses to medications can vary significantly. Always consult with a healthcare professional for personalized recommendations.
The Role of Genetic Testing in Treatment Selection: Depression Treatment How Genetic Testing Can Help Find The Right Medication

Genetic testing is rapidly evolving as a potential tool to personalize depression treatment. While not a cure-all, understanding the genetic underpinnings of a person’s response to medication can significantly improve treatment outcomes. This approach moves beyond a one-size-fits-all strategy, offering a more targeted and potentially more effective path toward recovery.The genetic information, combined with a thorough clinical assessment, can help clinicians make more informed decisions about the most appropriate medication and dosage, potentially reducing trial-and-error periods and side effects.
So, depression treatment and how genetic testing can help pinpoint the right medication is fascinating. It’s a real game-changer, potentially avoiding trial-and-error with different drugs. However, we need to be aware of the big business of medical misinformation, the big business of medical misinformation out there, making it crucial to rely on reputable sources and qualified professionals when researching these advancements.
Ultimately, responsible use of genetic testing in depression treatment can be a powerful tool for improved outcomes.
This personalized approach is particularly valuable in cases where standard treatments haven’t yielded the desired results.
Potential Benefits of Genetic Testing in Antidepressant Selection
Genetic variations can influence how individuals metabolize and respond to antidepressants. This means some people may metabolize a medication too quickly, requiring higher doses or different medications, while others might metabolize it too slowly, leading to adverse effects. Genetic testing can identify these variations, potentially predicting an individual’s likelihood of response to specific medications. This predictive power can lead to more effective and efficient treatment plans, reducing the time it takes to find the right medication.
Personalizing Treatment Plans with Genetic Information
Genetic testing can significantly personalize treatment plans by providing insights into an individual’s unique genetic makeup. This information allows clinicians to tailor the treatment strategy to the specific needs of the patient. For example, if a genetic test indicates a higher likelihood of a particular side effect with a certain medication, the clinician can choose an alternative that is less likely to cause those issues.
This approach minimizes the risk of adverse reactions and improves patient compliance with the treatment plan.
Importance of Patient Consent and Data Privacy in Genetic Testing
Patient consent is paramount when considering genetic testing for depression treatment. Individuals should be fully informed about the purpose, potential benefits, risks, and limitations of the test. Data privacy is equally crucial. Strict protocols must be in place to protect the confidentiality and security of the genetic information obtained. This includes measures to prevent unauthorized access and ensure the data is used only for the intended purpose of treatment.
Methods for Integrating Genetic Data into Treatment Decisions
Different methods exist for incorporating genetic data into treatment decisions. One approach involves using genetic information to guide the selection of a specific antidepressant, taking into account the patient’s genetic predisposition to metabolize certain medications. Another method involves adjusting the dosage of a chosen medication based on genetic markers associated with metabolism rates. Ultimately, the best method will depend on the specific genetic findings and the patient’s clinical presentation.
Finding the right medication for depression can be a real challenge, but genetic testing is offering exciting possibilities. It can help pinpoint the specific genetic variations that might be influencing how your body responds to different drugs. This kind of personalized approach could be incredibly helpful, just like how understanding the underlying causes of recurrent miscarriages is critical – for example, test the cause of many miscarriages to identify potential genetic factors.
Ultimately, this precision medicine approach promises a more effective and tailored treatment plan for depression.
Limitations of Genetic Testing in Depression Treatment
Genetic testing, while promising, is not a perfect predictor of treatment response. Environmental factors, lifestyle choices, and other individual differences can also influence a person’s response to medication. Further, the accuracy and predictive power of genetic tests are constantly evolving. Current tests may not fully capture the complexity of the genetic factors influencing depression or medication response.
Clinicians must exercise caution and interpret genetic results within the broader context of the patient’s overall health and history.
Steps in Incorporating Genetic Testing Results into a Treatment Plan
| Step | Action | Rationale |
|---|---|---|
| 1 | Obtain informed consent from the patient | Ensuring the patient understands the test’s purpose, potential benefits, risks, and limitations, and agrees to participate. |
| 2 | Analyze genetic test results | Identify genetic variations relevant to medication response. |
| 3 | Consult with a genetic counselor or clinician experienced in pharmacogenomics | Interpret the genetic results within the context of the patient’s clinical presentation and medical history. |
| 4 | Develop a personalized treatment plan | Incorporate the genetic information into the selection of antidepressant medication and dosage. |
| 5 | Monitor treatment response and adjust as needed | Ensure the treatment plan remains effective and addresses any emerging issues. |
Challenges and Ethical Considerations of Genetic Testing
Unveiling the genetic underpinnings of depression offers a promising avenue for personalized treatment, but navigating the associated challenges and ethical considerations is crucial. The intricate interplay of genes, environment, and individual experiences makes interpreting genetic data for depression complex, demanding careful consideration of potential biases and misinterpretations. This necessitates a thoughtful approach to ensure responsible and equitable application of genetic testing in mental health care.
Interpreting Complex Genetic Data
Genetic data related to depression is often multifaceted and not easily translated into definitive predictions of medication response. Numerous genes and complex interactions contribute to the development and manifestation of depression. Simple genetic markers, while potentially offering some insight, may not fully capture the intricate interplay of biological and environmental factors. For instance, a specific genetic variant might increase susceptibility to depression, but environmental stressors can significantly influence its expression.
The nuanced relationship between genes and depression requires sophisticated analytical methods and a comprehensive understanding of the individual’s complete medical and lifestyle history.
Potential for Misinterpretation and Misuse
Genetic information, especially when incompletely understood, can be misinterpreted, leading to potentially harmful outcomes. Misinterpretations can stem from a lack of clear understanding of genetic interactions and the limitations of current knowledge. Furthermore, the misuse of genetic information, such as discrimination in insurance or employment based on predispositions, is a significant ethical concern. The potential for stigmatization based on genetic profiles must be addressed proactively to prevent the perpetuation of harmful stereotypes.
Ethical Implications of Using Genetic Information
Using genetic information for treatment decisions raises significant ethical questions. Informed consent becomes paramount, ensuring individuals fully understand the potential benefits, limitations, and risks associated with genetic testing. The potential for genetic discrimination, including the denial of insurance coverage or employment opportunities based on a perceived genetic predisposition, demands stringent legal safeguards. Transparency in the interpretation and application of genetic findings is essential to build trust and ensure responsible use of this powerful tool.
Potential Biases in Genetic Testing Data
Genetic testing data may reflect existing societal biases and inequalities. For example, studies used to develop testing algorithms might not represent the diversity of the population, leading to inaccurate or ineffective results for individuals from underrepresented groups. Furthermore, the interpretation of genetic data might be influenced by implicit biases in clinical practice, which can lead to unequal access to appropriate treatments.
Careful consideration of diverse populations is essential to ensure that genetic testing benefits all individuals equitably.
Addressing Ethical Concerns in Genetic Testing
Addressing ethical concerns surrounding genetic testing for depression requires a multi-faceted approach. Establishing clear guidelines and regulations for the use of genetic information is vital. Public education and awareness campaigns can promote understanding of genetic testing, its limitations, and the potential for bias. Establishing robust ethical review boards can ensure that genetic testing protocols and interpretations adhere to established standards and principles.
Table of Ethical Considerations and Potential Solutions
| Concern | Explanation | Potential Solution |
|---|---|---|
| Misinterpretation of complex genetic data | Genetic results can be misinterpreted due to the complexity of gene interactions and environmental influences. | Develop comprehensive guidelines for interpreting genetic data in the context of depression, emphasizing the importance of considering environmental and lifestyle factors alongside genetic markers. |
| Misuse of genetic information | Genetic information could be misused in contexts like insurance or employment decisions. | Implement strict regulations and legal safeguards to prevent discrimination based on genetic predispositions. |
| Bias in genetic testing data | Existing societal biases may be reflected in the development and interpretation of genetic testing data. | Ensure diverse representation in the populations used for developing genetic testing algorithms and interpret results with caution, acknowledging potential biases and considering environmental factors. |
| Lack of informed consent | Individuals may not fully understand the implications of genetic testing for depression. | Provide comprehensive, accessible, and culturally sensitive information about genetic testing to promote informed consent and empower individuals to make informed decisions. |
Future Directions and Research

The journey to understanding depression and its treatment is an ongoing quest. Genetic testing, while providing valuable insights, is still a relatively young field. The future holds immense promise as researchers delve deeper into the intricate interplay between genes, environmental factors, and individual responses to treatment. We can anticipate a future where personalized treatments become even more sophisticated, leading to better outcomes and a more holistic approach to mental health.
The Potential of Combining Genetic Data with Clinical Factors
Integrating genetic data with other clinical factors, such as age, gender, family history, lifestyle, and even environmental exposures, is a key area of focus. This integrative approach can provide a richer understanding of individual vulnerability and resilience to depression. By considering the full spectrum of influencing factors, clinicians can move beyond a simple genetic predisposition and tailor treatment strategies that address the unique needs of each patient.
Finding the right medication for depression can be tricky, but genetic testing is offering some exciting possibilities. It can help pinpoint the specific genetic factors influencing a person’s response to different treatments. Interestingly, similar to how genetics might impact depression treatment, studies have shown a correlation between childhood bullying and later substance abuse issues. For example, research suggests children who bully are more likely to use alcohol or drugs later in life, children who bully more likely to use alcohol drugs later in life.
Ultimately, understanding these complex links can help us tailor treatments and interventions to better support mental health across the lifespan, from early childhood development to adult care.
For instance, a patient with a genetic predisposition to depression, coupled with a history of childhood trauma, might benefit from a combined therapy approach that integrates medication with trauma-focused counseling. This personalized strategy recognizes that genetic predisposition interacts with environmental influences to shape an individual’s experience with depression.
Developing More Personalized and Effective Treatments
The potential for developing more personalized and effective treatments is substantial. By understanding how specific genetic variations influence a person’s response to different medications, researchers can predict which treatments are most likely to be effective and reduce the time and resources spent on ineffective therapies. This targeted approach promises to optimize treatment outcomes, potentially reducing the need for trial-and-error approaches and minimizing side effects.
Consider a scenario where a patient is found to have a specific genetic marker associated with a higher risk of side effects from a particular antidepressant. By knowing this, the doctor can explore alternative medications that are more likely to be well-tolerated.
Innovative Research Strategies
Several innovative research strategies are emerging to advance genetic-based depression treatments. One promising approach is the use of large-scale genomic studies to identify new genetic variants associated with depression and treatment response. These studies can involve analyzing the genetic data of thousands of individuals to pinpoint subtle correlations that might have been missed in smaller studies. Another strategy focuses on developing sophisticated bioinformatic tools to analyze complex genetic interactions and predict treatment outcomes with greater accuracy.
This involves using powerful computer algorithms to interpret the vast amounts of genetic data, revealing subtle patterns that might otherwise remain hidden. Furthermore, exploring the interaction of genetic factors with environmental stressors is gaining traction. Research efforts are underway to identify specific environmental triggers that exacerbate depression in individuals with particular genetic predispositions.
Key Research Areas in Genetic Influences on Depression
| Area | Description | Potential Impact |
|---|---|---|
| Identification of Novel Genetic Variants | Pinpointing specific genes and variations associated with depression and treatment response. | Development of more precise diagnostic tools and targeted therapies. |
| Exploration of Gene-Environment Interactions | Investigating how genetic predispositions interact with environmental factors to influence depression risk and treatment outcomes. | Improved understanding of the complex etiology of depression and development of preventive strategies. |
| Development of Predictive Models | Creating algorithms that predict individual responses to different treatments based on genetic and clinical data. | Optimized treatment selection, reduced trial-and-error, and improved patient outcomes. |
| Personalized Treatment Strategies | Tailoring treatment plans based on individual genetic profiles and clinical characteristics. | Enhanced efficacy of interventions, reduced side effects, and improved patient adherence. |
Case Studies and Examples
Personalized medicine is rapidly changing the landscape of depression treatment. Genetic testing, when integrated thoughtfully, can provide crucial insights into an individual’s unique response to medication, potentially leading to faster symptom relief and fewer side effects. By understanding the genetic underpinnings of depression and its treatment, we can move towards a more precise and effective approach to care.This section explores hypothetical case studies, illustrating how genetic data can inform treatment decisions and enhance patient outcomes.
We’ll examine the process of incorporating genetic information into a treatment plan, including crucial patient counseling components.
Hypothetical Case Study 1: Identifying a Candidate for Selective Serotonin Reuptake Inhibitors (SSRIs)
“A 25-year-old female, Sarah, presents with symptoms consistent with major depressive disorder. Her family history suggests a predisposition to depression. Genetic testing reveals a specific genetic variant associated with a heightened response to SSRIs.”
Sarah’s genetic profile, coupled with her symptoms and family history, suggests a strong likelihood of positive response to SSRIs. This information allows the clinician to prioritize SSRIs as the initial treatment option, potentially accelerating symptom reduction. The genetic data also helps to predict potential side effects, allowing for proactive monitoring and dose adjustments. Further, this information provides a basis for tailoring treatment to individual needs, potentially reducing trial-and-error periods and optimizing outcomes.
Integrating Genetic Information into Treatment Plans, Depression treatment how genetic testing can help find the right medication
The integration of genetic data into a treatment plan requires a careful, multi-step process. First, the genetic test results must be interpreted by a qualified clinician with expertise in both genetics and mental health. This ensures accurate interpretation of complex genetic information within the context of the patient’s overall health and circumstances. Crucially, the clinician must explain the results in a way that is clear and understandable to the patient, addressing any concerns or anxieties they may have.Second, the results are integrated into a broader treatment plan.
The patient’s existing medical history, lifestyle factors, and preferences are taken into account. The discussion with the patient focuses on the potential benefits and risks of incorporating genetic information, emphasizing that genetic predispositions are not deterministic.
Patient Counseling and Informed Consent
Comprehensive patient counseling is paramount when incorporating genetic information into treatment. This process involves:
- Explaining the rationale behind genetic testing and its potential impact on treatment decisions.
- Detailing the limitations of genetic testing and the importance of considering non-genetic factors.
- Discussing the potential benefits and risks of using genetic information to personalize treatment.
- Ensuring the patient’s understanding of the test results and how they relate to their individual situation.
- Obtaining informed consent for the use of genetic information in the treatment plan.
Open communication and shared decision-making are essential to ensure patient empowerment and adherence to the treatment plan.
Potential Benefits and Risks
Genetic testing for depression treatment offers numerous potential benefits, including:
- Faster symptom relief by targeting the most effective medication.
- Reduced trial-and-error periods, leading to more efficient treatment.
- Minimizing side effects by identifying individuals at higher risk.
- Improved patient outcomes through personalized treatment strategies.
However, it’s important to acknowledge potential risks:
- Misinterpretation of genetic data without adequate clinical expertise.
- Potential for genetic discrimination or stigmatization.
- Cost of genetic testing and the need for equitable access.
- The need for ongoing research to fully understand the complex interplay between genes and depression.
Careful consideration of these potential benefits and risks is crucial for responsible implementation of genetic testing in depression treatment.
End of Discussion
In conclusion, depression treatment is moving towards a more personalized future, leveraging genetic testing to enhance treatment effectiveness. While challenges and ethical considerations remain, the potential for improved outcomes and reduced side effects is significant. As research progresses and ethical frameworks solidify, genetic testing holds promise for revolutionizing how we approach and treat depression.