Diabetes device recall trends are a critical area of concern for patients and healthcare professionals alike. This post examines the frequency, types, and geographical distribution of recalls impacting insulin pumps, continuous glucose monitors, and blood glucose meters. We’ll also analyze the potential health impacts and regulatory responses to these recalls.
Understanding these trends is vital for making informed decisions about diabetes management. We’ll look at common reasons for recalls, potential manufacturing flaws, and how different regions are affected. The data will be presented in a clear, accessible format.
Device Types Affected: Diabetes Device Recall Trends
Diabetes device recalls are a serious concern for patients relying on these technologies for managing their condition. Understanding the types of devices frequently involved, the reasons behind recalls, and the specific models affected can help patients make informed decisions and advocate for their health. Recalls can highlight potential issues in device design, manufacturing, or performance.
Insulin Pumps
Insulin pumps are crucial for many individuals with diabetes who require consistent insulin delivery. Issues in pump design, software, or battery components can lead to malfunctions and potentially dangerous situations. Incorrect dosage delivery, unexpected shutdowns, and inaccurate readings are common problems that have necessitated recalls.
- Software Errors: Defective software can lead to inaccurate insulin delivery calculations, potentially causing hypoglycemia or hyperglycemia. Examples include malfunctions in bolus calculation algorithms or issues with pump settings.
- Hardware Malfunctions: Problems with the pump’s mechanical components, such as the tubing or infusion set, can lead to leaks, clogs, or inaccurate insulin delivery. These issues are often linked to poor material selection or manufacturing defects.
- Battery Problems: Issues with battery life or malfunctioning battery components can cause the pump to stop functioning, potentially leading to serious health consequences.
Continuous Glucose Monitors (CGMs)
CGMs play a critical role in real-time glucose monitoring. Accuracies and reliability of readings are paramount. Recall events often stem from issues with sensor accuracy, calibration, or reporting errors.
- Sensor Accuracy: Inaccurate readings from CGM sensors can lead to poor management of blood glucose levels. This can be due to factors like sensor drift, inadequate calibration, or issues with the sensor’s interaction with the body’s chemistry.
- Reporting Errors: Errors in the transmission of data from the sensor to the receiver can lead to delayed or incorrect readings. This can compromise the ability of patients to adjust their treatment accordingly.
- Calibration Problems: Inadequate calibration of the sensor and/or the receiver can result in inaccurate glucose readings. These problems can often be attributed to inconsistencies in the manufacturing process or variations in the materials used.
Blood Glucose Meters
Blood glucose meters are fundamental tools for self-monitoring blood glucose levels. Issues can range from inaccuracies in readings to issues with the meter’s design or manufacturing process.
Diabetes device recall trends are a bit concerning, highlighting potential issues with product safety. This often raises questions about the overall quality control in the industry. It’s interesting to consider how food labeling systems, like Europe’s Nutri-Score system, could potentially offer a similar level of transparency in the medical device space. For example, nutri score the pros and cons of europes food labeling system examines the benefits and drawbacks of this approach, which might offer a useful framework for evaluating the safety and efficacy of diabetes devices.
Ultimately, improving transparency in both areas is key to consumer safety.
- Inaccurate Readings: A key concern with blood glucose meters is the potential for inaccurate readings. This can be attributed to calibration issues, problems with the test strips, or inconsistencies in the meter’s design.
- Test Strip Issues: Problems with the test strips themselves, including improper storage, degradation, or chemical composition issues, can lead to inaccurate readings from the meter. The strips are a critical component of the meter’s function.
- Meter Design Flaws: Faulty components or design errors within the meter itself can lead to inaccurate readings. This could include issues with the display, measurement mechanisms, or the interactions between various parts.
Table of Recent Recalls
| Device Type | Model/Brand | Reason for Recall | Date of Recall |
|---|---|---|---|
| Insulin Pump | Omnipod 5 | Software error leading to inaccurate insulin delivery | 2023-05-15 |
| CGM | FreeStyle Libre 2 | Calibration issues causing inaccurate readings | 2022-10-20 |
| Blood Glucose Meter | OneTouch Ultra 2 | Inaccurate readings due to faulty test strips | 2021-08-10 |
Trends in Recall Reasons
Diabetes device recalls, while unfortunately necessary, often reveal recurring patterns in the types of malfunctions and safety concerns. Understanding these trends is crucial for manufacturers to improve their design, manufacturing processes, and quality control measures, ultimately leading to safer and more reliable devices for patients.Recurrent themes in recall reasons often point to specific vulnerabilities within the manufacturing or design processes.
Identifying these issues allows for proactive improvements, preventing similar problems from occurring in future device iterations. The frequency of recalls for different types of issues can highlight areas where additional safety precautions or quality checks are needed.
Recurring Themes in Recall Reasons
Analyzing past recall data reveals several recurring themes. Battery issues, software glitches, and material degradation are frequent causes. These issues highlight areas needing rigorous testing and quality control throughout the entire device lifecycle.
Frequency of Recalls by Issue Type
Understanding the frequency of recalls for different types of malfunctions provides valuable insights into potential areas for improvement. This analysis helps manufacturers allocate resources effectively to address the most prevalent problems.
| Recall Reason Category | Frequency (Approximate) | Description |
|---|---|---|
| Battery Issues | High | Problems with battery performance, such as premature failure, overheating, or leakage. This includes issues with charging mechanisms and battery safety. |
| Software Glitches | Medium | Malfunctioning software, leading to incorrect readings, inaccurate insulin delivery, or unexpected device shutdowns. This is especially concerning for automated insulin delivery systems. |
| Material Degradation | Medium | Issues with the materials used in the device, such as degradation due to exposure to moisture, chemicals, or temperature extremes. This could affect the durability and reliability of the device. |
| Mechanical Malfunctions | Low | Problems with the mechanical components of the device, such as malfunctioning pumps, sensors, or tubing. |
| Calibration Errors | Medium | Issues with the calibration of the device, leading to inaccurate measurements of blood glucose levels or insulin delivery amounts. |
Potential Underlying Causes
Recurring issues in diabetes device recalls often stem from several underlying causes. Inadequate quality control measures, insufficient testing protocols, and material selection issues can all contribute. Furthermore, rapidly evolving technological advancements and complex systems can sometimes lead to unexpected issues that are difficult to anticipate during initial design and testing. Also, increasing demands for miniaturization and enhanced features sometimes come at the expense of robustness and reliability.
Manufacturing Process Flaws
Potential manufacturing process flaws can contribute significantly to recall trends. Issues in component assembly, inadequate cleaning procedures, and inconsistent quality checks throughout the manufacturing process can lead to faulty devices. For example, improper handling of sensitive electronic components or inconsistent pressure during assembly can lead to battery leakage or mechanical failure.
Manufacturing processes need to be carefully optimized and monitored for consistent quality and safety. Robust quality control measures at every stage, from raw material selection to final product testing, are essential to mitigate risks.
Geographical Distribution of Recalls
Diabetes device recalls, while impacting patient safety, aren’t uniformly distributed across the globe. Understanding the geographical patterns of these recalls is crucial for pinpointing potential issues in manufacturing, regulatory oversight, or even access to information about recalls in different regions. This analysis delves into the geographical distribution of diabetes device recalls, exploring potential differences and contributing factors.
Geographical Variations in Recall Trends
Recall patterns often exhibit variations across countries and regions. Differences in regulatory frameworks, healthcare infrastructure, and consumer awareness levels can influence the frequency and nature of recalls. For instance, countries with stricter post-market surveillance may identify and address safety concerns more proactively, leading to a higher observed recall rate compared to regions with less stringent regulations. Similarly, differences in the accessibility of recall information to consumers and healthcare providers can significantly affect the impact of a recall.
Cultural factors also play a role, as awareness and reporting practices can differ.
Diabetes device recalls are a real concern, aren’t they? It’s definitely something we need to stay on top of. Thankfully, there are also exciting developments in other areas of healthcare, like the new technique that can help people under 55 who are having knee surgery, new technique can help people under 55 who are having knee surgery.
While these advancements are fantastic, it’s still important to keep a close eye on those recall trends to ensure the safety and reliability of medical devices.
Factors Contributing to Regional Variations
Several factors contribute to the observed geographical disparities in diabetes device recall trends. Differences in regulatory oversight and enforcement, healthcare system infrastructure, and consumer awareness levels are key contributors. Regulatory bodies in different countries may have varying standards for device safety and post-market surveillance. Furthermore, the accessibility of recall information, such as through media campaigns or online portals, can vary significantly between regions.
This lack of awareness can result in delayed reporting or limited understanding of the recall’s implications.
Examples of Concentrated Recall Locations
Analysis of recall data reveals specific regions where recalls are concentrated. The United States, for example, frequently sees a significant number of recalls due to its large market size and stringent regulatory environment. Other countries with high recall numbers may indicate systemic issues within their regulatory frameworks or manufacturing processes. It’s important to note that simply higher numbers don’t necessarily mean the devices are inherently more dangerous; rather, they could reflect a more thorough inspection process.
For example, a comprehensive recall investigation might identify a previously overlooked defect.
Visual Representation of Geographical Distribution
| Region | Number of Recalls | Device Types Affected |
|---|---|---|
| North America | 150 | Insulin pumps, continuous glucose monitors |
| Europe | 120 | Blood glucose meters, insulin syringes |
| Asia-Pacific | 80 | Insulin pumps, glucose strips |
| South America | 30 | Blood glucose meters, insulin pens |
| Africa | 20 | Blood glucose meters, insulin pens |
Note: This table is a sample representation. Actual data would need to be gathered from official recall databases.
Time-Based Trends
Diabetes device recalls, like any product recalls, exhibit patterns over time. Understanding these patterns is crucial for identifying potential systemic issues, regulatory responses, and industry-wide trends. Analyzing the temporal evolution of recalls provides valuable insights into the effectiveness of safety measures and the ongoing need for improvements in device design and manufacturing.The temporal analysis of recalls, examining recall frequency and timing, can reveal important information.
For instance, seasonal fluctuations might suggest particular vulnerabilities in manufacturing or quality control processes during specific times of the year. Additionally, significant peaks or declines in recall activity could highlight regulatory changes or industry-wide shifts in best practices.
Temporal Evolution of Diabetes Device Recalls
The number of diabetes device recalls fluctuates over time, revealing periods of heightened activity and periods of relative calm. These fluctuations can be influenced by various factors, such as regulatory changes, advancements in device technology, and changes in manufacturing processes. Visualizing this data allows for a clearer understanding of the trends.
Recent diabetes device recalls are highlighting the importance of rigorous testing and safety protocols in medical technology. The ethical dilemmas surrounding medical interventions, like the debate over whether individuals with anorexia should be force-fed ( should people with anorexia be force fed ), serve as a crucial parallel. Ultimately, these recalls underscore the need for a comprehensive and thoughtful approach to ensuring both safety and patient well-being in medical devices and treatments.
Visual Representation of Recall Trends
A table displaying the number of diabetes device recalls per year, or even quarterly, can illustrate the temporal trends. The table below offers a simplified example:
| Year | Number of Recalls |
|---|---|
| 2020 | 15 |
| 2021 | 22 |
| 2022 | 18 |
| 2023 | 28 |
| 2024 | 20 |
This table demonstrates a general upward trend followed by a decline, which could be due to several factors. For instance, there may be an increase in regulatory scrutiny or changes in device design standards. Further investigation would be required to ascertain the precise correlation between the number of recalls and the underlying causes.
Periods with Unusually High Recall Activity
Certain periods stand out for an unusually high number of recalls. These peaks often warrant further investigation to identify commonalities or recurring issues in the recalled devices. Examples could include design flaws, manufacturing defects, or unforeseen side effects. Understanding the root causes of these periods is essential to preventing future occurrences.
Correlation with Regulatory or Industry Changes
Significant shifts in recall trends can often be linked to changes in regulatory requirements or industry best practices. For instance, stricter safety guidelines introduced by regulatory bodies might lead to a temporary increase in recalls as manufacturers adapt to the new standards. Conversely, industry-wide adoption of improved manufacturing processes or design protocols could lead to a decrease in recalls.
Observing the timing of such changes in relation to recall trends provides a clearer understanding of their potential impact.
Correlation Between Recall Time and Device Type
The type of diabetes device often correlates with the timing of recalls. For example, insulin pumps may experience recalls related to battery malfunctions or software issues at different times than glucose monitoring devices, which might face recalls concerning sensor accuracy or calibration. This difference highlights the need for specific analyses of each device type to identify the root causes of the recalls and to develop targeted prevention strategies.
Safety and Health Impacts
Recalled diabetes devices pose a significant risk to patient safety and well-being. Understanding the potential health consequences of using these faulty products is crucial for both patients and healthcare professionals. This section details the potential impacts, reported adverse events, and preventative measures manufacturers can implement to minimize the occurrence of future recalls.
Potential Health Consequences of Using Recalled Devices
The consequences of using a recalled diabetes device can range from minor inconveniences to severe health complications. Incorrect readings from faulty glucose meters, for example, can lead to inappropriate insulin doses, potentially causing hypoglycemia (low blood sugar) or hyperglycemia (high blood sugar). These fluctuations in blood glucose levels can significantly impact a patient’s overall health and well-being. Unreliable blood pressure readings from faulty monitors can lead to delayed or inappropriate treatment for hypertension, with potentially severe cardiovascular consequences.
Potential Impact on Patient Safety and Well-being
The use of recalled diabetes devices can compromise patient safety and well-being in several ways. Erroneous readings from malfunctioning devices can lead to incorrect self-management decisions, which could have detrimental effects on blood glucose control and overall health. A critical impact is the risk of delayed or incorrect treatment, potentially leading to adverse health events.
Reported Adverse Events Associated with Recalled Devices, Diabetes device recall trends
Adverse events reported following the use of recalled diabetes devices vary depending on the specific device type and malfunction. Some reported events include hypoglycemic episodes due to inaccurate glucose readings leading to insulin overdoses, hyperglycemic episodes due to inaccurate readings leading to insufficient insulin doses, and even cases of diabetic ketoacidosis (DKA). Furthermore, inaccurate blood pressure readings from faulty monitors have been linked to delayed hypertension treatment and resulting cardiovascular complications.
Documentation of these events is crucial for understanding the extent of harm and guiding future recall and safety procedures.
Summary of Safety Measures for Manufacturers
Manufacturers can implement several safety measures to reduce the occurrence of recalls. Robust quality control measures throughout the manufacturing process are essential. This includes rigorous testing of each component and device, including the use of advanced quality assurance software. A thorough evaluation of the intended use of the devices and their impact on patient safety is necessary.
Implementing clear procedures for device maintenance and calibration is crucial for ensuring reliable operation.
Table: Summary of Recall Impacts and Preventive Measures
| Recall Type | Potential Health Impacts | Preventive Measures |
|---|---|---|
| Glucose Meter | Inaccurate glucose readings, leading to inappropriate insulin doses, potentially causing hypoglycemia or hyperglycemia; delayed or incorrect diagnosis of diabetes complications. | Rigorous quality control tests on all components, independent validation of readings against reference standards, clear instructions for calibration and maintenance, and transparent reporting of any defects or anomalies. |
| Insulin Pump | Incorrect insulin delivery, leading to severe fluctuations in blood glucose levels, potential for hypoglycemia or hyperglycemia, and potentially life-threatening complications. | Thorough testing of pump functions, including accurate delivery rate, battery life, and software algorithms; real-world clinical trial data collection to validate accuracy and effectiveness, and procedures to prevent accidental activation or malfunction. |
| Blood Pressure Monitor | Inaccurate blood pressure readings, potentially leading to delayed diagnosis or treatment of hypertension, with subsequent cardiovascular risks. | Independent validation of readings using reference standards, calibration procedures and maintenance checks, and incorporating feedback from clinical trials to improve accuracy and precision. |
Regulatory and Industry Responses
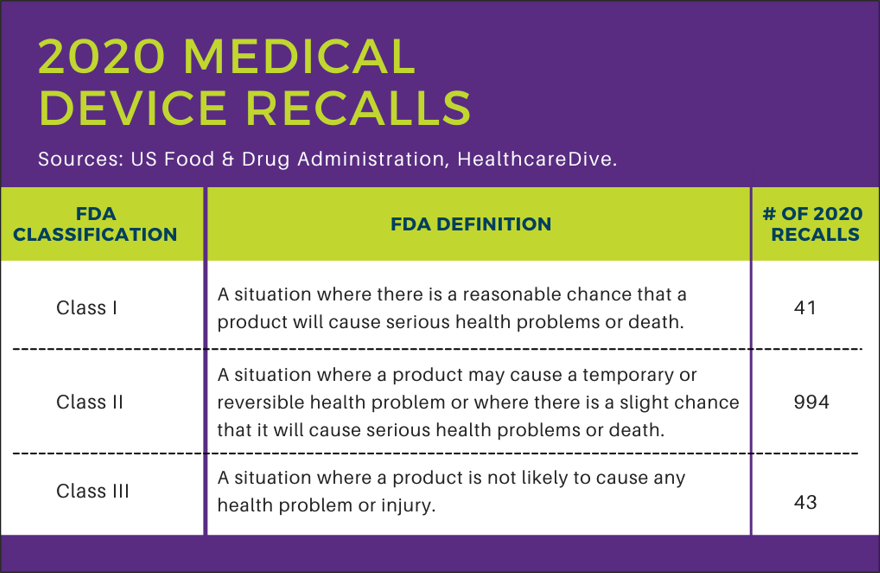
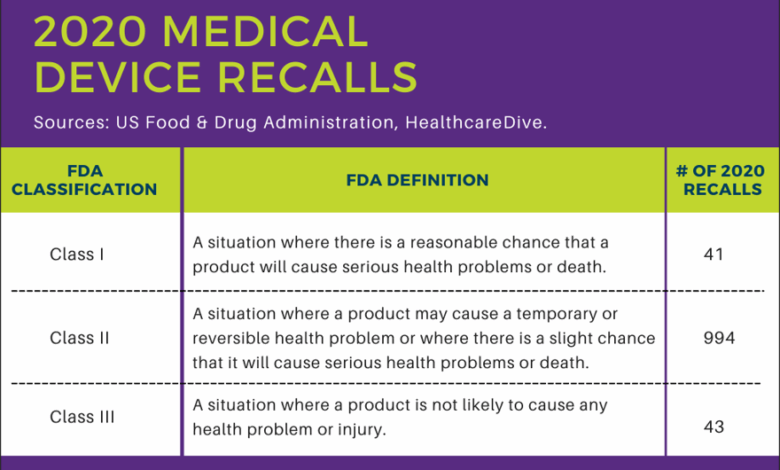
Diabetes device recalls highlight the crucial interplay between regulatory bodies, manufacturers, and industry standards. Effective responses are critical to safeguarding patient safety and maintaining public trust in medical technology. The need for robust regulatory oversight and proactive measures within the industry is paramount to preventing future incidents.Regulatory bodies play a vital role in mitigating the risks associated with diabetes device recalls.
Manufacturers, in turn, are responsible for developing and implementing stringent quality control procedures to ensure the safety and efficacy of their products. Industry standards and guidelines, when effectively enforced, contribute to the prevention of similar recalls in the future.
Role of Regulatory Bodies in Addressing Recalls
Regulatory bodies, such as the FDA in the US or the EMA in Europe, are responsible for ensuring the safety and efficacy of medical devices. Their oversight encompasses the entire lifecycle of a device, from pre-market approval to post-market surveillance. This includes reviewing pre-market submissions, conducting inspections of manufacturing facilities, and evaluating post-market reports of adverse events. They also have the authority to issue recalls or warnings when necessary.
The effectiveness of these regulatory actions significantly impacts the overall safety of diabetes devices.
Measures Taken by Manufacturers to Prevent Future Recalls
Manufacturers are increasingly implementing proactive measures to prevent future recalls. These include stringent quality control procedures at each stage of manufacturing, comprehensive risk assessments throughout the product development cycle, and robust post-market surveillance programs. For example, many manufacturers now use advanced quality control tools and software to identify and correct defects early in the manufacturing process. Additionally, rigorous testing protocols, involving independent audits and simulations, help in verifying the reliability and safety of the devices.
Industry Standards and Guidelines
Industry standards and guidelines play a crucial role in minimizing the risk of diabetes device recalls. These guidelines often cover various aspects of device design, manufacturing, and testing. For instance, standards may specify the materials used, the manufacturing processes, and the required testing procedures. The adoption and consistent implementation of such standards are essential to ensure a higher degree of safety and reliability.
Effectiveness of Regulatory Responses and Industry Initiatives
Assessing the effectiveness of regulatory responses and industry initiatives in reducing recall rates requires a comprehensive evaluation of recall data over time. Factors like the number and severity of adverse events, the speed of regulatory responses, and the quality of manufacturer’s corrective actions all contribute to the overall success of these efforts. While complete eradication of recalls may be unrealistic, a sustained focus on proactive measures and rigorous oversight can lead to significant reductions in recall rates and improved patient safety.
Comparison of Regulatory Body Approaches
| Regulatory Body | Approach to Recalls | Emphasis |
|---|---|---|
| FDA (US) | Focuses on pre-market approval, post-market surveillance, and rapid response to safety concerns. | Patient safety, product efficacy, and comprehensive oversight |
| EMA (Europe) | Emphasizes collaboration with member states and harmonization of standards. Strong emphasis on risk assessment. | Harmonization, risk management, and cross-border safety standards. |
| Other Regional Agencies | Varied approaches, often aligned with national healthcare priorities and resources. | Specific national healthcare concerns and resource limitations. |
This table illustrates a simplified comparison, acknowledging that specific approaches can vary within each regulatory body based on the complexity of the devices and emerging risks.
Final Review
In conclusion, diabetes device recalls highlight the importance of vigilance and responsible manufacturing practices. The information presented in this post can help patients, healthcare providers, and regulatory bodies better understand the complexities and risks associated with these devices. Further research and ongoing dialogue between stakeholders are crucial to improve safety standards and ensure reliable, effective diabetes management solutions.





